Rheumatoid Arthritis

Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body. The disease may also affect other parts of the body. This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart. Fever and low energy may also be present. Often, symptoms come on gradually over weeks to months.
While the cause of rheumatoid arthritis is not clear, it is believed to involve a combination of genetic and environmental factors. The underlying mechanism involves the body's immune system attacking the joints. This results in inflammation and thickening of the joint capsule. It also affects the underlying bone and cartilage. The diagnosis is made mostly on the basis of a person's signs and symptoms. X-rays and laboratory testing may support a diagnosis or exclude other diseases with similar symptoms. Other diseases that may present similarly include systemic lupus erythematosus, psoriatic arthritis, and fibromyalgia among others.
The goals of treatment are to reduce pain, decrease inflammation, and improve a person's overall functioning. This may be helped by balancing rest and exercise, the use of splints and braces, or the use of assistive devices. Pain medications, steroids, and NSAIDs are frequently used to help with symptoms. Disease-modifying antirheumatic drugs (DMARDs), such as hydroxychloroquine and methotrexate, may be used to try to slow the progression of disease. Biological DMARDs may be used when disease does not respond to other treatments. However, they may have a greater rate of adverse effects. Surgery to repair, replace, or fuse joints may help in certain situations. Most alternative medicine treatments are not supported by evidence.
RA affects about 24.5 million people as of 2015. This is between 0.5 and 1% of adults in the developed world with 5 and 50 per 100,000 people newly developing the condition each year. Onset is most frequent during middle age and women are affected 2.5 times as frequently as men. It resulted in 38,000 deaths in 2013, up from 28,000 deaths in 1990. The first recognized description of RA was made in 1800 by Dr. Augustin Jacob Landré-Beauvais (1772–1840) of Paris. The term rheumatoid arthritis is based on the Greek for watery and inflamed joints.
Signs and symptoms
RA primarily affects joints, but it also affects other organs in more than 15–25% of cases. Associated problems include cardiovascular disease, osteoporosis, interstitial lung disease, infection, cancer, feeling tired, depression, mental difficulties, and trouble working.
Joints
Arthritis of joints involves inflammation of the synovial membrane. Joints become swollen, tender and warm, and stiffness limits their movement. With time, multiple joints are affected (polyarthritis). Most commonly involved are the small joints of the hands, feet and cervical spine, but larger joints like the shoulder and knee can also be involved.:1098 Synovitis can lead to tethering of tissue with loss of movement and erosion of the joint surface causing deformity and loss of function. The fibroblast-like synoviocytes (FLS), highly specialized mesenchymal cells found in the synovial membrane, have an active and prominent role in these pathogenic processes of the rheumatic joints.
RA typically manifests with signs of inflammation, with the affected joints being swollen, warm, painful and stiff, particularly early in the morning on waking or following prolonged inactivity. Increased stiffness early in the morning is often a prominent feature of the disease and typically lasts for more than an hour. Gentle movements may relieve symptoms in early stages of the disease. These signs help distinguish rheumatoid from non-inflammatory problems of the joints, such as osteoarthritis. In arthritis of non-inflammatory causes, signs of inflammation and early morning stiffness are less prominent. The pain associated with RA is induced at the site of inflammation and classified as nociceptive as opposed to neuropathic. The joints are often affected in a fairly symmetrical fashion, although this is not specific, and the initial presentation may be asymmetrical.:1098
As the pathology progresses the inflammatory activity leads to tendon tethering and erosion and destruction of the joint surface, which impairs range of movement and leads to deformity. The fingers may suffer from almost any deformity depending on which joints are most involved. Specific deformities, which also occur in osteoarthritis, include ulnar deviation, boutonniere deformity (also "buttonhole deformity", flexion of proximal interphalangeal joint and extension of distal interphalangeal joint of the hand), swan neck deformity (hyperextension at proximal interphalangeal joint and flexion at distal interphalangeal joint) and "Z-thumb." "Z-thumb" or "Z-deformity" consists of hyperextension of the interphalangeal joint, fixed flexion and subluxation of the metacarpophalangeal joint and gives a "Z" appearance to the thumb.:1098 The hammer toe deformity may be seen. In the worst case, joints are known as arthritis mutilans due to the mutilating nature of the deformities.
Skin
The rheumatoid nodule, which is sometimes in the skin, is the most common non-joint feature and occurs in 30% of people who have RA. It is a type of inflammatory reaction known to pathologists as a "necrotizing granuloma". The initial pathologic process in nodule formation is unknown but may be essentially the same as the synovitis, since similar structural features occur in both. The nodule has a central area of fibrinoid necrosis that may be fissured and which corresponds to the fibrin-rich necrotic material found in and around an affected synovial space. Surrounding the necrosis is a layer of palisading macrophages and fibroblasts, corresponding to the intimal layer in synovium and a cuff of connective tissue containing clusters of lymphocytes and plasma cells, corresponding to the subintimal zone in synovitis. The typical rheumatoid nodule may be a few millimetres to a few centimetres in diameter and is usually found over bony prominences, such as the elbow, the heel, the knuckles, or other areas that sustain repeated mechanical stress. Nodules are associated with a positive RF (rheumatoid factor) titer, ACPA, and severe erosive arthritis. Rarely, these can occur in internal organs or at diverse sites on the body.
Several forms of vasculitis occur in RA, but are mostly seen with long-standing and untreated disease. The most common presentation is due to involvement of small- and medium-sized vessels. Rheumatoid vasculitis can thus commonly present with skin ulceration and vasculitic nerve infarction known as mononeuritis multiplex.
Other, rather rare, skin associated symptoms include pyoderma gangrenosum, Sweet's syndrome, drug reactions, erythema nodosum, lobe panniculitis, atrophy of finger skin, palmar erythema, and skin fragility (often worsened by corticosteroid use).
Diffuse alopecia areata (Diffuse AA) occurs more commonly in people with rheumatoid arthritis. RA is also seen more often in those with relatives who have AA.
Lungs
Lung fibrosis is a recognized complication of rheumatoid arthritis. It is also a rare but well-recognized consequence of therapy (for example with methotrexate and leflunomide). Caplan's syndrome describes lung nodules in individuals with RA and additional exposure to coal dust. Exudative pleural effusions are also associated with RA.
Heart and blood vessels
People with RA are more prone to atherosclerosis, and risk of myocardial infarction (heart attack) and stroke is markedly increased. Other possible complications that may arise include: pericarditis, endocarditis, left ventricular failure, valvulitis and fibrosis. Many people with RA do not experience the same chest pain that others feel when they have angina or myocardial infarction. To reduce cardiovascular risk, it is crucial to maintain optimal control of the inflammation caused by RA (which may be involved in causing the cardiovascular risk), and to use exercise and medications appropriately to reduce other cardiovascular risk factors such as blood lipids and blood pressure. Doctors who treat people with RA should be sensitive to cardiovascular risk when prescribing anti-inflammatory medications, and may want to consider prescribing routine use of low doses of aspirin if the gastrointestinal effects are tolerable.
Blood
Anemia is by far the most common abnormality of the blood cells which can be caused by a variety of mechanisms. The chronic inflammation caused by RA leads to raised hepcidin levels, leading to anemia of chronic disease where iron is poorly absorbed and also sequestered into macrophages. The red cells are of normal size and color (normocytic and normochromic). A low white blood cell count usually only occurs in people with Felty's syndrome with an enlarged liver and spleen. The mechanism of neutropenia is complex. An increased platelet count occurs when inflammation is uncontrolled.
Other
Kidneys
Renal amyloidosis can occur as a consequence of untreated chronic inflammation. Treatment with penicillamine and gold salts are recognized causes of membranous nephropathy.
Eyes
The eye can be directly affected in the form of episcleritis or scleritis, which when severe can very rarely progress to perforating scleromalacia. Rather more common is the indirect effect of keratoconjunctivitis sicca, which is a dryness of eyes and mouth caused by lymphocyte infiltration of lacrimal and salivary glands. When severe, dryness of the cornea can lead to keratitis and loss of vision as well as being painful. Preventive treatment of severe dryness with measures such as nasolacrimal duct blockage is important.
Liver
Liver problems in people with rheumatoid arthritis may be due to the underlying disease process or as a result of the medications used to treat the disease. A coexisting autoimmune liver disease, such as primary biliary cirrhosis or autoimmune hepatitis may also cause problems.
Neurological
Peripheral neuropathy and mononeuritis multiplex may occur. The most common problem is carpal tunnel syndrome caused by compression of the median nerve by swelling around the wrist. Rheumatoid disease of the spine can lead to myelopathy. Atlanto-axial subluxation can occur, owing to erosion of the odontoid process and/or transverse ligaments in the cervical spine's connection to the skull. Such an erosion (>3mm) can give rise to vertebrae slipping over one another and compressing the spinal cord. Clumsiness is initially experienced, but without due care, this can progress to quadriplegia or even death.
Constitutional symptoms
Constitutional symptoms including fatigue, low grade fever, malaise, morning stiffness, loss of appetite and loss of weight are common systemic manifestations seen in people with active RA.
Bones
Local osteoporosis occurs in RA around inflamed joints. It is postulated to be partially caused by inflammatory cytokines. More general osteoporosis is probably contributed to by immobility, systemic cytokine effects, local cytokine release in bone marrow and corticosteroid therapy.
Cancer
The incidence of lymphoma is increased, although it is uncommon and associated with the chronic inflammation, not the treatment of RA. The risk of non-melanoma skin cancer is increased in people with RA compared to the general population, an association possibly due to the use of immunosuppression agents for treating RA.
Teeth
Periodontitis and tooth loss are common in people with rheumatoid arthritis.
Risk factors
RA is a systemic (whole body) autoimmune disease. Some genetic and environmental factors affect the risk for RA.
Genetic
A family history of RA increases the risk around three to five times; as of 2016, it was estimated that genetics may account for between 40 and 65% of cases of seropositive RA, but only around 20% for seronegative RA. RA is strongly associated with genes of the inherited tissue type major histocompatibility complex (MHC) antigen. HLA-DR4 is the major genetic factor implicated – the relative importance varies across ethnic groups.
Genome-wide association studies examining single-nucleotide polymorphisms have found around one hundred alleles associated with RA risk. Risk alleles within the HLA (particularly HLA-DRB1) genes harbor more risk than other loci. The HLA encodes proteins which controls recognition of self versus nonself molecules. Other risk loci include genes affecting co-stimulatory immune pathways, for example CD28 and CD40, cytokine signaling, lymphocyte receptor activation threshold (e.g., PTPN22), and innate immune activation appear to have less influence than HLA mutations.
Environmental
There are established epigenetic and environmental risk factors for RA. Smoking is an established risk factor for RA in Caucasian populations, increasing the risk three times compared to non-smokers, particularly in men, heavy smokers, and those who are rheumatoid factor positive. Modest alcohol consumption may be protective.
Silica exposure has been linked to RA.
Negative findings
No infectious agent has been consistently linked with RA and there is no evidence of disease clustering to indicate its infectious cause, but periodontal disease has been consistently associated with RA.
The many negative findings suggest that either the trigger varies, or that it might, in fact, be a chance event inherent with the immune response.
Pathophysiology
RA primarily starts as a state of persistent cellular activation leading to autoimmunity and immune complexes in joints and other organs where it manifests. The clinical manifestations of disease are primarily inflammation of the synovial membrane and joint damage, and the fibroblast-like synoviocytes play a key role in these pathogenic processes. Three phases of progression of RA are an initiation phase (due to non-specific inflammation), an amplification phase (due to T cell activation), and chronic inflammatory phase, with tissue injury resulting from the cytokines, IL–1, TNF-alpha and IL–6.
Non-specific inflammation
Factors allowing an abnormal immune response, once initiated, become permanent and chronic. These factors are genetic disorders which change regulation of the adaptive immune response. Genetic factors interact with environmental risk factors for RA, with cigarette smoking as the most clearly defined risk factor.
Other environmental and hormonal factors may explain higher risks for women, including onset after childbirth and hormonal medications. A possibility for increased susceptibility is that negative feedback mechanisms – which normally maintain tolerance – are overtaken by positive feedback mechanisms for certain antigens, such as IgG Fc bound by rheumatoid factor and citrullinated fibrinogen bound by antibodies to citrullinated peptides (ACPA - Anti–citrullinated protein antibody). A debate on the relative roles of B-cell produced immune complexes and T cell products in inflammation in RA has continued for 30 years, but neither cell is necessary at the site of inflammation, only autoantibodies to IgGFc, known as rheumatoid factors and ACPA, with ACPA having an 80% specificity for diagnosing RA. As with other autoimmune diseases, people with RA have abnormally glycosylated antibodies, which are believed to promote joint inflammation.
Amplification in the synovium
Once the generalized abnormal immune response has become established – which may take several years before any symptoms occur – plasma cells derived from B lymphocytes produce rheumatoid factors and ACPA of the IgG and IgM classes in large quantities. These activate macrophages through Fc receptor and complement binding, which is part of the intense inflammation in RA. Binding of an autoreactive antibody to the Fc receptors is mediated through the antibody's N-glycans, which are altered to promote inflammation in people with RA.
This contributes to local inflammation in a joint, specifically the synovium with edema, vasodilation and entry of activated T-cells, mainly CD4 in microscopically nodular aggregates and CD8 in microscopically diffuse infiltrates. Synovial macrophages and dendritic cells function as antigen-presenting cells by expressing MHC class II molecules, which establishes the immune reaction in the tissue.
Chronic inflammation


The disease progresses by forming granulation tissue at the edges of the synovial lining, pannus with extensive angiogenesis and enzymes causing tissue damage. The fibroblast-like synoviocytes have a prominent role in these pathogenic processes. The synovium thickens, cartilage and underlying bone disintegrate, and the joint deteriorates, with raised calprotectin levels serving as a biomarker of these events.
Cytokines and chemokines attract and accumulate immune cells, i.e. activated T- and B cells, monocytes and macrophages from activated fibroblast-like synoviocytes, in the joint space. By signalling through RANKL and RANK, they eventually trigger osteoclast production, which degrades bone tissue. The fibroblast-like synoviocytes that are present in the synovium during rheumatoid arthritis display altered phenotype compared to the cells present in normal tissues. The aggressive phenotype of fibroblast-like synoviocytes in rheumatoid arthritis and the effect these cells have on the microenvironment of the joint can be summarized into hallmarks that distinguish them from healthy fibroblast-like synoviocytes. These hallmark features of fibroblast-like synoviocytes in rheumatoid arthritis are divided into 7 cell-intrinsic hallmarks and 4 cell-extrinsic hallmarks. The cell-intrinsic hallmarks are: reduced apoptosis, impaired contact inhibition, increased migratory invasive potential, changed epigenetic landscape, temporal and spatial heterogeneity, genomic instability and mutations, and reprogrammed cellular metabolism. The cell-extrinsic hallmarks of FLS in RA are: promotes osteoclastogenesis and bone erosion, contributes to cartilage degradation, induces synovial angiogenesis, and recruits and stimulates immune cells.
Diagnosis
Imaging


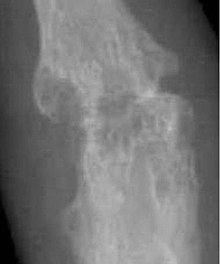
X-rays of the hands and feet are generally performed when many joints affected. In RA, there may be no changes in the early stages of the disease or the x-ray may show osteopenia near the joint, soft tissue swelling, and a smaller than normal joint space. As the disease advances, there may be bony erosions and subluxation. Other medical imaging techniques such as magnetic resonance imaging (MRI) and ultrasound are also used in RA.
Technical advances in ultrasonography like high-frequency transducers (10 MHz or higher) have improved the spatial resolution of ultrasound images depicting 20% more erosions than conventional radiography. Color Doppler and power Doppler ultrasound are useful in assessing the degree of synovial inflammation as they can show vascular signals of active synovitis. This is important, since in the early stages of RA, the synovium is primarily affected, and synovitis seems to be the best predictive marker of future joint damage.
Blood tests
When RA is clinically suspected, a physician may test for rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs measured as anti-CCP antibodies). It is positive in 75-85%, but a negative RF or CCP antibody does not rule out RA, rather, the arthritis is called seronegative, which is in about 15-25% of people with RA. During the first year of illness, rheumatoid factor is more likely to be negative with some individuals becoming seropositive over time. RF is a non-specific antibody and seen in about 10% of healthy people, in many other chronic infections like hepatitis C, and chronic autoimmune diseases such as Sjögren's syndrome and systemic lupus erythematosus. Therefore, the test is not specific for RA.
Hence, new serological tests check for anti-citrullinated protein antibodies ACPAs. These tests are again positive in 61-75% of all RA cases, but with a specificity of around 95%. As with RF, ACPAs are many times present before symptoms have started.
The by far most common clinical test for ACPAs is the anti-cyclic citrullinated peptide (anti CCP) ELISA. In 2008 a serological point-of-care test for the early detection of RA combined the detection of RF and anti-MCV with a sensitivity of 72% and specificity of 99.7%.
Other blood tests are usually done to differentiate from other causes of arthritis, like the erythrocyte sedimentation rate (ESR), C-reactive protein, full blood count, kidney function, liver enzymes and other immunological tests (e.g., antinuclear antibody/ANA) are all performed at this stage. Elevated ferritin levels can reveal hemochromatosis, a mimic of RA, or be a sign of Still's disease, a seronegative, usually juvenile, variant of rheumatoid arthritis.
Classification criteria
In 2010, the 2010 ACR / EULAR Rheumatoid Arthritis Classification Criteria were introduced.
The new criterion is not a diagnostic criterion but a classification criterion to identify disease with a high likelihood of developing a chronic form. However a score of 6 or greater unequivocally classifies a person with a diagnosis of rheumatoid arthritis.
These new classification criteria overruled the "old" ACR criteria of 1987 and are adapted for early RA diagnosis. The "new" classification criteria, jointly published by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) establish a point value between 0 and 10. Four areas are covered in the diagnosis:
- joint involvement, designating the metacarpophalangeal joints, proximal interphalangeal joints, the interphalangeal joint of the thumb, second through fifth metatarsophalangeal joint and wrist as small joints, and shoulders, elbows, hip joints, knees, and ankles as large joints:
- Involvement of 1 large joint gives 0 points
- Involvement of 2–10 large joints gives 1 point
- Involvement of 1–3 small joints (with or without involvement of large joints) gives 2 points
- Involvement of 4–10 small joints (with or without involvement of large joints) gives 3 points
- Involvement of more than 10 joints (with involvement of at least 1 small joint) gives 5 points
- serological parameters – including the rheumatoid factor as well as ACPA – "ACPA" stands for "anti-citrullinated protein antibody":
- Negative RF and negative ACPA gives 0 points
- Low-positive RF or low-positive ACPA gives 2 points
- High-positive RF or high-positive ACPA gives 3 points
- acute phase reactants: 1 point for elevated erythrocyte sedimentation rate, ESR, or elevated CRP value (c-reactive protein)
- duration of arthritis: 1 point for symptoms lasting six weeks or longer
The new criteria accommodate to the growing understanding of RA and the improvements in diagnosing RA and disease treatment. In the "new" criteria serology and autoimmune diagnostics carries major weight, as ACPA detection is appropriate to diagnose the disease in an early state, before joints destructions occur. Destruction of the joints viewed in radiological images was a significant point of the ACR criteria from 1987. This criterion no longer is regarded to be relevant, as this is just the type of damage that treatment is meant to avoid.
Differential diagnoses
| Type | WBC per mm3 | % neutrophils | Viscosity | Appearance |
|---|---|---|---|---|
| Normal | <200 | 0 | High | Transparent |
| Osteoarthritis | <5000 | <25 | High | Clear yellow |
| Trauma | <10,000 | <50 | Variable | Bloody |
| Inflammatory | 2,000-50,000 | 50-80 | Low | Cloudy yellow |
| Septic arthritis | >50,000 | >75 | Low | Cloudy yellow |
| Gonorrhea | ~10,000 | 60 | Low | Cloudy yellow |
| Tuberculosis | ~20,000 | 70 | Low | Cloudy yellow |
| Inflammatory = gout, rheumatoid arthritis, rheumatic fever | ||||
Several other medical conditions can resemble RA, and need to be distinguished from it at the time of diagnosis:
- Crystal induced arthritis (gout, and pseudogout) – usually involves particular joints (knee, MTP1, heels) and can be distinguished with an aspiration of joint fluid if in doubt. Redness, asymmetric distribution of affected joints, pain occurs at night and the starting pain is less than an hour with gout.
- Osteoarthritis – distinguished with X-rays of the affected joints and blood tests, older age, starting pain less than an hour, asymmetric distribution of affected joints and pain worsens when using joint for longer periods.
- Systemic lupus erythematosus (SLE) – distinguished by specific clinical symptoms and blood tests (antibodies against double-stranded DNA)
- One of the several types of psoriatic arthritis resembles RA – nail changes and skin symptoms distinguish between them
- Lyme disease causes erosive arthritis and may closely resemble RA – it may be distinguished by blood test in endemic areas
- Reactive arthritis – asymmetrically involves heel, sacroiliac joints and large joints of the leg. It is usually associated with urethritis, conjunctivitis, iritis, painless buccal ulcers, and keratoderma blennorrhagica.
- Axial spondyloarthritis (including ankylosing spondylitis) – this involves the spine, although an RA-like symmetrical small-joint polyarthritis may occur in the context of this condition.
- Hepatitis C – RA-like symmetrical small-joint polyarthritis may occur in the context of this condition. Hepatitis C may also induce rheumatoid factor auto-antibodies.
Rarer causes which usually behave differently but may cause joint pains:
- Sarcoidosis, amyloidosis, and Whipple's disease can also resemble RA.
- Hemochromatosis may cause hand joint arthritis.
- Acute rheumatic fever can be differentiated by a migratory pattern of joint involvement and evidence of antecedent streptococcal infection.
- Bacterial arthritis (such as by Streptococcus) is usually asymmetric, while RA usually involves both sides of the body symmetrically.
- Gonococcal arthritis (a bacterial arthritis) is also initially migratory and can involve tendons around the wrists and ankles.
Sometimes arthritis is in an undifferentiated stage (i.e. none of the above criteria is positive), even if synovitis is witnessed and assessed with ultrasound imaging.
Monitoring progression
Many tools can be used to monitor remission in rheumatoid arthritis.
- DAS28: Disease Activity Score of 28 joints (DAS28) is widely used as an indicator of RA disease activity and response to treatment. Joints included are (bilaterally): proximal interphalangeal joints (10 joints), metacarpophalangeal joints (10), wrists (2), elbows (2), shoulders (2) and knees (2). When looking at these joints, both the number of joints with tenderness upon touching (TEN28) and swelling (SW28) are counted. The erythrocyte sedimentation rate (ESR) is measured and the affected person makes a subjective assessment (SA) of disease activity during the preceding 7 days on a scale between 0 and 100, where 0 is "no activity" and 100 is "highest activity possible". With these parameters, DAS28 is calculated as:
From this, the disease activity of the affected person can be classified as follows:
| Current DAS28 |
DAS28 decrease from initial value | |||
|---|---|---|---|---|
| > 1.2 | > 0.6 but ≤ 1.2 | ≤ 0.6 | ||
| ≤ 3.2 | Inactive | Good improvement | Moderate improvement | No improvement |
| > 3.2 but ≤ 5.1 | Moderate | Moderate improvement | Moderate improvement | No improvement |
| > 5.1 | Very active | Moderate improvement | No improvement | No improvement |
It is not always a reliable indicator of treatment effect. One major limitation is that low-grade synovitis may be missed.
- Other: Other tools to monitor remission in rheumatoid arthritis are: ACR-EULAR Provisional Definition of Remission of Rheumatoid arthritis, Simplified Disease Activity Index and Clinical Disease Activity Index. Some scores do not require input from a healthcare professional and allow self-monitoring by the person, like HAQ-DI.
Prevention
There is no known prevention for the condition other than the reduction of risk factors.
Management
There is no cure for RA, but treatments can improve symptoms and slow the progress of the disease. Disease-modifying treatment has the best results when it is started early and aggressively. The results of a recent systematic review found that combination therapy with tumor necrosis factor (TNF) and non-TNF biologics plus methotrexate (MTX) resulted in improved disease control, Disease Activity Score (DAS)-defined remission, and functional capacity compared with a single treatment of either methotrexate or a biologic alone.
The goals of treatment are to minimize symptoms such as pain and swelling, to prevent bone deformity (for example, bone erosions visible in X-rays), and to maintain day-to-day functioning. This is primarily addressed with disease-modifying antirheumatic drugs (DMARDs); dosed physical activity; analgesics and physical therapy may be used to help manage pain. RA should generally be treated with at least one specific anti-rheumatic medication. The use of benzodiazepines (such as diazepam) to treat the pain is not recommended as it does not appear to help and is associated with risks.
Lifestyle
Regular exercise is recommended as both safe and useful to maintain muscles strength and overall physical function. Physical activity is beneficial for people with rheumatoid arthritis who experience fatigue, although there was little to no evidence to suggest that exercise may have an impact on physical function in the long term, a study found that carefully dosed exercise has shown significant improvements in patients with RA. Moderate effects have been found for aerobic exercises and resistance training on cardiovascular fitness and muscle strength in RA. Furthermore, physical activity had no detrimental side effects like increased disease activity in any exercise dimension. It is uncertain if eating or avoiding specific foods or other specific dietary measures help improve symptoms. Occupational therapy has a positive role to play in improving functional ability in people with rheumatoid arthritis. Weak evidence supports the use of wax baths (thermotherapy) to treat arthritis in the hands.
Educational approaches that inform people about tools and strategies available to help them cope with rheumatoid arthritis may improve a person's psychological status and level of depression in the shorter-term. The use of extra-depth shoes and molded insoles may reduce pain during weight-bearing activities such as walking. Insoles may also prevent the progression of bunions.
Disease modifying agents
Disease-modifying antirheumatic drugs (DMARDs) are the primary treatment for RA. They are a diverse collection of drugs, grouped by use and convention. They have been found to improve symptoms, decrease joint damage, and improve overall functional abilities. DMARDs should be started early in the disease as they result in disease remission in approximately half of people and improved outcomes overall.
The following drugs are considered as DMARDs: methotrexate, hydroxychloroquine, sulfasalazine, leflunomide, TNF-alpha inhibitors (certolizumab, infliximab and etanercept), abatacept, and anakinra. Rituximab and tocilizumab are monoclonal antibodies and are also DMARDs. Use of tocilizumab is associated with a risk of increased cholesterol levels.
Hydroxychloroquine, apart from its low toxicity profile, is considered effective in the moderate RA treatment.
The most commonly used agent is methotrexate with other frequently used agents including sulfasalazine and leflunomide. Leflunomide is effective when used from 6–12 months, with similar effectiveness to methotrexate when used for 2 years. Sulfasalazine also appears to be most effective in the short-term treatment of rheumatoid arthritis. Sodium aurothiomalate (gold) and cyclosporin are less commonly used due to more common adverse effects. However, cyclosporin was found to be effective in the progressive RA when used up to one year. Agents may be used in combinations however, people may experience greater side effects. Methotrexate is the most important and useful DMARD and is usually the first treatment. A combined approach with methotrexate and biologics improves ACR50, HAQ scores and RA remission rates. Triple therapy consisting of methotrexate, sulfasalazine and hydroxychloroquine may also effectively control disease activity. Adverse effects should be monitored regularly with toxicity including gastrointestinal, hematologic, pulmonary, and hepatic. Side effects such as nausea, vomiting or abdominal pain can be reduced by taking folic acid.
A 2015 Cochrane review found rituximab with methotrexate to be effective in improving symptoms compared to methotrexate alone. Rituximab works by decreasing levels of B-cells (immune cell that is involved in inflammation). People taking rituximab had improved pain, function, reduced disease activity and reduced joint damage based on x-ray images. After 6 months, 21% more people had improvement in their symptoms using rituximab and methotrexate.
Biological agents should generally only be used if methotrexate and other conventional agents are not effective after a trial of three months. They are associated with a higher rate of serious infections as compared to other DMARDs. Biological DMARD agents used to treat rheumatoid arthritis include: tumor necrosis factor alpha (TNFα) blockers such as infliximab; interleukin 1 blockers such as anakinra, monoclonal antibodies against B cells such as rituximab, and tocilizumab T cell co-stimulation blocker such as abatacept. They are often used in combination with either methotrexate or leflunomide. Biologic monotherapy or tofacitinib with methotrexate may improve ACR50, RA remission rates and function. Abatacept should not be used at the same time as other biologics. In those who are well controlled (low disease activity) on TNF blockers, decreasing the dose does not appear to affect overall function. Discontinuation of TNF blockers (as opposed to gradually lowering the dose) by people with low disease activity may lead to increased disease activity and may affect remission, damage that is visible on an x-ray, and a person's function. People should be screened for latent tuberculosis before starting any TNF blockers therapy to avoid reactivation of tuberculosis.
TNF blockers and methotrexate appear to have similar effectiveness when used alone and better results are obtained when used together. Golimumab is effective when used with methotraxate. TNF blockers may have equivalent effectiveness with etanercept appearing to be the safest. Injecting etanercept, in addition to methotrexate twice a week may improve ACR50 and decrease radiographic progression for up to 3 years. Abatacept appears effective for RA with 20% more people improving with treatment than without but long term safety studies are yet unavailable. Adalimumab slows the time for the radiographic progression when used for 52 weeks. However, there is a lack of evidence to distinguish between the biologics available for RA. Issues with the biologics include their high cost and association with infections including tuberculosis. Use of biological agents may reduce fatigue. The mechanism of how biologics reduce fatigue is unclear.
Anti-inflammatory and analgesic agents
Glucocorticoids can be used in the short term and at the lowest dose possible for flare-ups and while waiting for slow-onset drugs to take effect. Combination of glucocorticoids and conventional therapy has shown a decrease in rate of erosion of bones. Steroids may be injected into affected joints during the initial period of RA, prior to the use of DMARDs or oral steroids.
Non-NSAID drugs to relieve pain, like paracetamol may be used to help relieve the pain symptoms; they do not change the underlying disease. The use of paracetamol may be associated with the risk of developing ulcers.
NSAIDs reduce both pain and stiffness in those with RA but do not affect the underlying disease and appear to have no effect on people's long term disease course and thus are no longer first line agents. NSAIDs should be used with caution in those with gastrointestinal, cardiovascular, or kidney problems. Rofecoxib was withdrawn from the global market as its long-term use was associated to an increased risk of heart attacks and strokes. Use of methotrexate together with NSAIDs is safe, if adequate monitoring is done. COX-2 inhibitors, such as celecoxib, and NSAIDs are equally effective. A 2004 Cochrane review found that people preferred NSAIDs over paracetamol. However, it is yet to be clinically determined whether NSAIDs are more effective than paracetamol.
The neuromodulator agents topical capsaicin may be reasonable to use in an attempt to reduce pain. Nefopam by mouth and cannabis are not recommended as of 2012 as the risks of use appear to be greater than the benefits.
Limited evidence suggests the use of weak oral opioids but the adverse effects may outweigh the benefits.
Alternatively, physical therapy has been tested and shown as an effective aid in reducing pain in patients with RA. As most RA is detected early and treated aggressively, physical therapy plays more of a preventative and compensatory role, aiding in pain management alongside regular rheumatic therapy.
Surgery
Especially for affected fingers, hands, and wrists, synovectomy may be needed to prevent pain or tendon rupture when drug treatment has failed. Severely affected joints may require joint replacement surgery, such as knee replacement. Postoperatively, physiotherapy is always necessary.:1080, 1103 There is insufficient evidence to support surgical treatment on arthritic shoulders.
Physiotherapy
For people with RA, physiotherapy may be used together with medical management. This may include cold and heat application, electronic stimulation, and hydrotherapy.
Physiotherapy promotes physical activity. In RA, physical activity like exercise in the appropriate dosage (frequency, intensity, time, type, volume, progression) and physical activity promotion is effective in improving cardiovascular fitness, muscle strength, and maintaining a long term active lifestyle. Physical activity promotion according to the public health recommendations should be an integral part of standard care for people with RA and other arthritic diseases.
Alternative medicine
In general, there is not enough evidence
