Argininemia
A number sign (#) is used with this entry because argininemia is caused by homozygous or compound heterozygous mutation in the arginase-1 gene (ARG1; 608313) on chromosome 6q23.
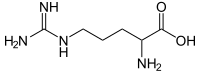
DescriptionArginase deficiency is an autosomal recessive inborn error of metabolism caused by a defect in the final step in the urea cycle, the hydrolysis of arginine to urea and ornithine.
Urea cycle disorders are characterized by the triad of hyperammonemia, encephalopathy, and respiratory alkalosis. Five disorders involving different defects in the biosynthesis of the enzymes of the urea cycle have been described: ornithine transcarbamylase deficiency (311250), carbamyl phosphate synthetase deficiency (237300), argininosuccinate synthetase deficiency, or citrullinemia (215700), argininosuccinate lyase deficiency (207900), and arginase deficiency.
Clinical FeaturesTerheggen et al. (1969, 1970) described 2 sisters, aged 18 months and 5 years, with spastic paraplegia, epileptic seizures, and severe mental retardation. The parents were related. Arginine levels were high in the blood and spinal fluid of the patients, with intermediate elevations in both parents and in 2 healthy sibs. Arginase activity in red cells was very low in the patients and intermediate in the parents. In 1971 another affected girl was born into the family observed by Terheggen et al. (1972, 1975). There was late introduction of a low protein diet, but the infant developed severe mental retardation, athetosis, and spasticity.
Cederbaum et al. (1977) reported a 7.5-year-old boy with progressive psychomotor retardation, behavior disturbance, and spasticity, who had growth arrest from age 3 years. Plasma arginine was increased, and red blood cell arginase activity was less than 1% of normal, whereas it was half-normal in both parents, 2 unaffected sibs, and in his paternal grandfather. Cederbaum et al. (1977) concluded that arginase deficiency is an autosomal recessive disorder. Michels and Beaudet (1978) reported an affected Mexican child with growth retardation, microcephaly, mental retardation, spasticity, and epileptiform discharges on EEG.
In the province of Quebec, Qureshi et al. (1983) identified an affected French Canadian family. Both parents showed activity of arginase 32 to 38% of normal. Walser (1983) stated that only 8 kindreds (with 13 patients) had been reported and that 4 of these (with 7 patients) were Spanish or Spanish-American. Jorda et al. (1986) described an unusually severe case of arginase deficiency in a Spanish infant who showed marked protein intolerance early in life. The levels of red cell arginase in the parents and 1 sister were consistent with heterozygosity. Brockstedt et al. (1990) described argininemia in a 4-year-old boy born of consanguineous Pakistani parents. He had microcephaly and spastic tetraplegia. Pregnancy and birth were uneventful and psychomotor development during the first 2 years of life were presumably normal. Vilarinho et al. (1990) described argininemia in a 5-year-old Portuguese boy who did not show spastic diplegia. His first manifestation, at 3.5 years of age, was a partial seizure for 15 minutes without loss of consciousness. Six months later he showed the same clinical features over a period of 15 days. The electroencephalogram showed partial left temporal and paracentral spikes. At 4.5 years of age he began to have episodes of vomiting, hypotonia, irritability, and ataxia.
In a patient dying with severe argininemia, Grody et al. (1989) demonstrated total absence of arginase I in tissues, whereas arginase II was increased about 4-fold in kidney. The patient, an offspring of first-cousin parents of Cambodian descent, died at 6 months of age. Although Southern blot analysis failed to show a substantial deletion in the ARG1 gene, no cross-reactive arginine I protein could be demonstrated by immunoprecipitation-competition and Western blot analysis. Induction studies in cell lines that express only the type II isozyme indicated that its activity could be enhanced several fold by exposure to elevated arginine levels. This presumably was the mechanism for the high level of the enzyme in the patient and explained the fact that there is persistent ureagenesis in this disorder.
Christmann et al. (1990) described a patient in whom the diagnosis of argininemia was first made at the age of 18 years when treatment with sodium valproate was initiated for seizures. The patient had psychomotor regression since the age of 15 months with paraparesis since she was 3 years old. By the age of 18, she was bedridden. Five days after the initiation of valproate therapy, she went into a state of stupor and was found to have marked hyperammonemia. 'Valproate sensitivity' has been observed also with ornithine transcarbamylase deficiency and citrullinemia, 2 other causes of hyperammonemia. Scheuerle et al. (1993) described 2 unrelated patients, aged 9 and 5 years, who had been thought to have cerebral palsy and were later found to have arginase deficiency. The experience suggested that the condition may be underdiagnosed because of its relatively mild symptoms. The authors noted that arginase deficiency does not commonly have the severe hyperammonemia seen with other urea cycle disorders.
Cowley et al. (1998) described an 18-year-old woman, born of related parents, who had been well as a child with normal growth and development. She presented for investigation of collapse with sudden onset of spastic diplegia. She had mild, tender hepatomegaly. Over the previous 6 months, she had been ill with episodic nausea and vomiting, and had experienced some degree of lower limb weakness over the previous 2 weeks. The spastic diplegia in this patient was considered stereotypical of arginase deficiency. No arginase activity was detected in liver tissue; red cell arginase activity was low normal.
Picker et al. (2003) described a rare neonatal and fatal presentation of arginase deficiency in a 2-day-old female with markedly elevated plasma arginine, lactate, and CSF glutamine, and modestly elevated blood ammonia, who developed hypertonia and tachypnea followed by intractable seizures and global cerebral edema. The infant also had an atypical presence of the ARG2 isozyme (107830) in the liver. Picker et al. (2003) suggested that the cerebral edema and the fatal course, both of which have been reported in older patients, were due to the increased intracellular osmolarity of the elevated glutamine.
Batshaw et al. (2014) reported the results of an analysis of 614 patients with urea cycle disorders (UCDs) enrolled in the Urea Cycle Disorders Consortium's longitudinal study protocol. Arginase deficiency occurred in 22 patients (3.5%).
Diez-Fernandez et al. (2018) summarized data on 112 reported patients with argininemia, including their own. The majority of patients had later-onset disease, and the severity of the disease ranged from no clinical symptoms to severe mental retardation, seizures, and spastic paraplegia. All patients with neonatal onset presented with peak arginine concentrations (pretreatment) of greater than 971 umol/l, whereas nearly all patients with later onset (98%) presented with initial arginine values of less than 971 umol/l. All patients identified by newborn screening had mild or no clinical symptoms. Ammonia was not typically elevated, highlighting that the urea cycle is not interrupted in argininemia.
Clinical ManagementQureshi et al. (1984) recommended a combination of benzoate with arginine restriction in the management of hyperargininemia. Bernar et al. (1986) reported the case of a 12-year-old boy with less marked elevations of plasma arginine and less severe intellectual impairment. Both were attributed to a self-selected low-protein diet. Therapy with sodium benzoate and dietary restriction caused an impressive improvement.
Diez-Fernandez et al. (2018) summarized data on 112 reported patients with argininemia, including their own. Patients are treated with nitrogen scavengers, severe restriction of natural protein, and essential amino acids supplementation. Enzyme replacement has also been used successfully. In patients with neonatal-onset argininemia under treatment, average arginine levels ranged between 163 and 489 umol/l, and in patients with late-onset disease under treatment, average arginine levels ranged between 163 and 381 umol/l. These data demonstrate the difficulty of achieving arginine levels under 200 umol/l, as has been recommended.
Molecular GeneticsIn a study of 20 persons homozygous or heterozygous for arginase deficiency, Grody et al. (1989) found no substantial structural ARG1 gene deletions or other rearrangements by Southern blot analysis.
In a Japanese girl with argininemia, Haraguchi et al. (1990) found compound heterozygosity for 2 frameshift deletions in the ARG1 gene (608313.0001-608313.0002).
In 11 patients with argininemia, 9 separate mutations representing 21 of the 22 mutant alleles were identified by Uchino et al. (1995) (see, e.g., 608313.0008-608313.0011). Four of these mutations, accounting for 64% of the mutant alleles, were expressed in vitro and were found to be severe or moderate. Patients with at least one 'moderate' mutant allele responded well to dietary treatment, whereas patients with 2 'severe' alleles did not respond to dietary treatment.
Diez-Fernandez et al. (2018) summarized data on all published and 12 novel ARG1 mutations, totaling 66 mutations from 112 patients. Missense mutations were the most common (30), followed by deletions (15), splicing (10), nonsense (7), duplications (2), insertions (1), and a translation initiation codon mutation. Most of the mutations (48) were found in single families, with 15 in up to 4 families and only 3 mutations (T134I; G235R, 608313.0006; and R21X, 608313.0012) found in 5, 14, and 16 families, respectively. The 30 missense mutations were distributed unevenly throughout the 8 exons, clustering in exons 1, 4, and 7. No clear genotype-phenotype correlation was observed. Even patients carrying homozygous 'devastating' mutations (e.g., nonsense and splicing) could develop later onset of the disease. Most ARG1 mutations led to late-onset disease; 6 mutations were associated with neonatal-onset disease (I8K, G106R, c.466-2A-G, c.77delA, c.262_265delAAGA (608313.0001), and c.647_648ins32).
Animal ModelShih et al. (1972) found high blood arginine levels and low red cell arginase in Macaca fascicularis monkeys in the New England Regional Primate Center, indicating arginase deficiency.
Iyer et al. (2002) produced Arg1-knockout mice that duplicated several pathobiologic aspects of human argininemia.
Deignan et al. (2008) stated that several guanidino compounds, which are direct or indirect metabolites of arginine, are elevated in the blood of uremic patients and in the plasma and cerebrospinal fluid of hyperargininemic patients. They found that the guanidino compounds alpha-keto-delta-guanidinovaleric acid, alpha-N-acetylarginine, and argininic acid were increased in brain tissue from the Arg1-deficient mouse model of hyperargininemia. Several guanidino compounds were also elevated in plasma, liver, and kidney. Deignan et al. (2008) concluded that guanidino compounds may be the neuropathogenic agents responsible for complications in arginase deficiency.
Population GeneticsThe prevalence of argininemia is estimated to be 1 in 1,100,000 (Testai and Gorelick, 2010).
HistoryThe observation that researchers working with the Shope virus have low blood arginine led to the use of Shope virus in the treatment of this disorder. Rogers et al. (1973) reported an induction of arginase activity by inoculation of the Shope virus into tissue cultures of an argininemic patient's fibroblasts.