Fructose Intolerance, Hereditary
A number sign (#) is used with this entry because hereditary fructose intolerance is caused by homozygous or compound heterozygous mutation in the gene encoding aldolase B (ALDOB; 612724) on chromosome 9q31.
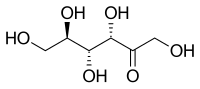
DescriptionFructose intolerance becomes apparent in infancy at the time of weaning, when fructose or sucrose is added to the diet. Clinical features include recurrent vomiting, abdominal pain, and hypoglycemia that may be fatal. Long-term exposure to fructose can result in liver failure, renal tubulopathy, and growth retardation. Older patients who survive infancy develop a natural avoidance of sweets and fruits. Ali et al. (1998) provided a detailed review of the biochemical, genetic, and molecular basis of aldolase B deficiency in hereditary fructose intolerance.
Clinical FeaturesChambers and Pratt (1956) first reported fructose intolerance in a 24-year-old woman who complained of nausea, abdominal pain, and faintness after ingesting sugar and fructose. She did not enjoy sweet tastes. The authors termed the phenomenon 'idiosyncrasy to fructose,' and postulated that some of the symptoms resulted from hypoglycemia (Ali et al., 1998).
Perheentupa and Pitkanen (1962) reported a severely affected infant who had recurrent hypoglycemia and vomiting after weaning, when fructose or sucrose was added to the diet. The symptoms resulted in marked malnutrition. However, the patient's 3-year-old brother only developed hepatomegaly and hypoglycemic shock after an oral test dose of fructose. He was otherwise clinically healthy, but showed a marked aversion to sweets and fruit.
Froesch et al. (1963) described 2 adults, aged 33 and 39 years, with fructose intolerance. In addition to the aversion to fructose-containing foods, both had a remarkable absence of dental caries. Swales and Smith (1966) described an affected 21-year-old man, and Kohlin and Melin (1968) reported adult cases.
Mass et al. (1966) reported a patient with fructose intolerance who had developed renal tubular acidosis. It was unclear to the authors whether this was an independent disorder or a complication of the fructosemia. Perheentupa and Raivio (1967) discussed hyperuricemia in this disorder.
Mandel et al. (1990) reported an infant with fructose intolerance in whom the diagnosis was delayed due to the finding of hemophagocytosis in the bone marrow. The authors noted that most, if not all, patients with fructose intolerance have neonatal hypoglycemia, lactic acidosis, and an abnormal fructose or glycerol loading test. Hypoglycemic attacks occur later in life and are associated with severe hyperuricemia and metabolic acidosis. Therapeutic measures include restriction of fructose intake and avoidance of prolonged fasting, particularly during febrile episodes.
Ali et al. (1998) noted that infants with fructose intolerance can have a severe reaction, including lethargy, seizures, and coma, if large quantities of sugar are ingested. In addition, persistent intake can lead to chronic toxicity, including liver and kidney damage. Those who survive the early period without correct diagnosis develop a self-protective aversion to the harmful sugars.
Esposito et al. (2010) reported 2 unrelated patients with fructose intolerance who were determined to be heterozygous for a mutation in the ALDOB gene. One patient with an R46W substitution (612724.0014) had mild hypoglycemia and ketosis after ingestion of fructose and a marked aversion to sweets and fruit. The second patient with a Y343H substitution (612724.0015) was hospitalized for a series of febrile episodes associated with sever liver dysfunction at age 8 months. She died 1 month later from unknown causes. In vitro functional expression studies of both variants showed variably compromised enzyme activity. The report emphasized that heterozygous ALDOB mutations may result in symptoms in some patients.
Clinical Variability
An adult form of fructose intolerance was reported by Lameire et al. (1978) in a Belgian patient. When a fructose solution was used for intravenous alimentation during management of viral meningitis, a 21-year-old man developed severe illness characterized by acute jaundice, gastrointestinal bleeding, hypoglycemia, proximal tubular acidosis, and disseminated intravascular coagulation. The renal disorder was characterized by glycosuria, amino aciduria, phosphaturia, and bicarbonaturia with high urinary pH despite metabolic acidosis. Liver fructose-1-phosphate aldolase activity was 30% of normal, and fructose-1,6-diphosphate aldolase activity was normal. In classic fructose intolerance, these values are 0 to 6% and 10 to 50% of normal, respectively. Thus, the patient appeared to have a mild form of the disorder, may have been heterozygous, and likely showed manifestations only because of the massive fructose infusion.
Biochemical FeaturesRichardson et al. (1979) reported the typical biochemical changes in an 18-year-old man with fructose intolerance after oral ingestion of fructose. He developed fructosemia, hypoglycemia, hypophosphatemia, hyperuricemia, and metabolic acidosis primarily due to lactic acidosis.
Jaeken et al. (1996) investigated the serum lysosomal enzymes beta-hexosaminidase (HEXA; 606869) and beta-glucuronidase (GUSB; 611499) in 2 patients with hereditary fructose intolerance and found abnormalities identical to those in carbohydrate-deficient glycoprotein syndrome type I (see CDGIb; 602579), but different from those in untreated galactosemia (230400). In studies in rat liver, they found that fructose-1-phosphate was a potent competitive inhibitor of phosphomannose isomerase, the first enzyme of the N-glycosylation pathway, thus explaining the N-glycosylation disturbances in hereditary fructose intolerance.
InheritanceHereditary fructose intolerance is an autosomal recessive disorder (Ali et al., 1998).
Wolf et al. (1959) reported cases of fructose intolerance in a father and son, but the mother was likely heterozygous.
Since aldolase B is normally present in kidney and intestinal mucosa as well as in liver, Cox et al. (1982) were able to detect heterozygotes by intestinal biopsy. In a Jewish family, they demonstrated that apparent dominant inheritance was the result of a homozygote-heterozygote mating.
DiagnosisIn aldolase B-deficient tissues, cytoplasmic accumulation of fructose-1-phosphate leads to sequestration of inorganic phosphate with resulting activation of AMP deaminase that catalyzes the irreversible deamination of AMP to IMP (inosine monophosphate), a precursor of uric acid. In the cytoplasm, AMP, ADP, and ATP are maintained in a state approaching equilibrium. Depletion of tissue ATP occurs through massive degradation to uric acid and impairment of regeneration by oxidative phosphorylation in the mitochondria because of inorganic phosphate depletion. In the cell, ATP exists largely as a 1:1 complex with magnesium. Depletion of ATP in tissues leads to depletion also of magnesium concentration. Oberhaensli et al. (1987) used (31)P magnetic resonance spectroscopy to study the effect of fructose on liver metabolism in patients with this disorder. In heterozygotes, the method could be used to diagnose fructose intolerance and to monitor patient compliance with a restricted diet. Ingestion of small amounts of fructose was followed by an increase in sugar phosphates and decrease in inorganic phosphate in the liver. In heterozygotes, fructose led to accumulation of sugar phosphates and depletion of inorganic phosphate in the liver. Fructose also induced a larger increase in plasma urate in heterozygotes than in control subjects. Heterozygosity for this disorder may predispose to hyperuricemia.
Edstrom (1990) emphasized hereditary fructose intolerance as the basis of vomiting in infants. Oral administration of a fructose solution resulted in a characteristic decrease in serum glucose and phosphorus within 1 hour.
Paolella et al. (1987) described a RFLP within the ALDOB gene useful in the study of hereditary fructose intolerance.
Clinical ManagementGitzelmann et al. (1974) demonstrated that antiserum against crystallized fructosediphosphate aldolase B from human liver activated the mutant enzyme in liver extracts from 3 patients with hereditary fructose intolerance, but not in 2 others. Both genetic heterogeneity and potential for therapy were suggested.
Mock et al. (1983) described 2 unrelated boys with hereditary fructose intolerance and growth retardation which occurred even though acute symptomatic fructose intoxication was prevented by restriction of dietary fructose. Stringent limitation of fructose intake resulted in accelerated growth. Experimental challenge with fructose caused sustained hyperuricemia and hyperuricosuria and increased plasma and urine levels of magnesium, without symptoms, hypoglycemia, or evidence of hepatic or renal dysfunction.
Marks et al. (1989) described the obstetrical management of a woman with fructose intolerance. Her first child had failure to thrive and died at 6 months; autopsy showed cirrhosis and pulmonary edema, with a clinical diagnosis of E. coli sepsis. Her second child also had fructose intolerance and died at age 5 years from acquired immunodeficiency syndrome contracted from a neonatal blood transfusion. On a strict fructose-free diet, her third pregnancy proceeded well; the child, who was also found to have fructose intolerance, did well on a fructose-free diet. Diagnosis of fructose intolerance was said to have been verified in the mother by biopsy of the liver. Presumably the father of these children was at least heterozygous for the fructose intolerance gene.
Molecular GeneticsIn affected individuals from several unrelated families with fructose intolerance, Cross et al. (1988) identified homozygosity for a mutation in the ALDOB gene (A149P; 612724.0001). The findings indicated that this mutation may be a common cause of the disorder.
Cross and Cox (1990) identified deletions in the aldolase B gene in patients with fructose intolerance. Two were large deletions of 1.65 kb and 1.4 kb, respectively, whereas the third was a small 4-bp deletion (612724.0004).
Tolan (1995) reviewed 21 ALDOB mutations that had been reported to that time; 15 were single-base substitutions, resulting in 9 amino acid replacements, 4 nonsense codons, and 2 putative splicing defects, and the other 6 were deletions. Recurrent mutations were observed in exons 5 and 9.
Among 162 patients from 92 families with hereditary fructose intolerance, Davit-Spraul et al. (2008) identified 16 different mutations in the ALDOB gene, including 8 novel mutations. Most of the patients were French. The most common mutations were A149P (64%), A174D (612724.0002) (16%), and N335K (612724.0013) (5%). Screening for these 3 mutations alone confirmed the diagnosis in 69 (75%) of 92 probands. There were no apparent genotype/phenotype correlations.
In 6 unrelated Italian patients with hereditary fructose intolerance, Esposito et al. (2010) identified a 6.5-kb deletion in the ALDOB gene (612724.0013). The authors could not rule out the possibility of a founder effect.
Population GeneticsThe incidence of hereditary fructose intolerance in the Caucasian population has been estimated at 1 in 20,000 births (Cross et al., 1990).
By haplotype analysis, Tolan (1995) demonstrated that the A149P (612724.0001) and A174D (612724.0002) ALDOB mutations originated from a single founder and had achieved a relatively high frequency through genetic drift.
In the United Kingdom, about 1.3% of neonates carry 1 copy of the A149P mutation (Ali et al., 1998).
Animal ModelOppelt et al. (2015) found that the phenotype of Aldo2-null mice is a phenocopy of hereditary fructose intolerance. The null mice showed failure to thrive and liver dysfunction that was exacerbated by fructose ingestion. Livers of Aldo2-null mice exhibited rapid onset of hepatic steatosis that could be reversed by removal of fructose from the diet.
NomenclatureBy analogy to galactosemia (230400), Levin et al. (1963) suggested the term 'fructosemia' to refer to hereditary fructose intolerance.