Achilles Tendon Rupture
Overview
Achilles (uh-KILL-eez) tendon rupture is an injury that affects the back of your lower leg. It mainly occurs in people playing recreational sports, but it can happen to anyone.
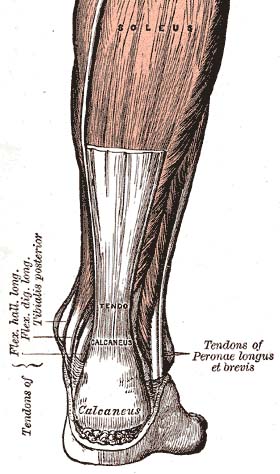
The Achilles tendon is a strong fibrous cord that connects the muscles in the back of your calf to your heel bone. If you overstretch your Achilles tendon, it can tear (rupture) completely or just partially.
If your Achilles tendon ruptures, you might hear a pop, followed by an immediate sharp pain in the back of your ankle and lower leg that is likely to affect your ability to walk properly. Surgery is often performed to repair the rupture. For many people, however, nonsurgical treatment works just as well.
Symptoms
Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people have:
- The feeling of having been kicked in the calf
- Pain, possibly severe, and swelling near the heel
- An inability to bend the foot downward or "push off" the injured leg when walking
- An inability to stand on the toes on the injured leg
- A popping or snapping sound when the injury occurs
When to see your doctor
Seek medical advice immediately if you hear a pop in your heel, especially if you can't walk properly afterward.
Causes
Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you walk and move your foot.
Rupture usually occurs in the section of the tendon situated within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section might be prone to rupture because blood flow is poor, which also can impair its ability to heal.
Ruptures often are caused by a sudden increase in the stress on your Achilles tendon. Common examples include:
- Increasing the intensity of sports participation, especially in sports that involve jumping
- Falling from a height
- Stepping into a hole
Risk factors
Factors that may increase your risk of Achilles tendon rupture include:
- Age. The peak age for Achilles tendon rupture is 30 to 40.
- Sex. Achilles tendon rupture is up to five times more likely to occur in men than in women.
- Recreational sports. Achilles tendon injuries occur more often during sports that involve running, jumping, and sudden starts and stops — such as soccer, basketball and tennis.
- Steroid injections. Doctors sometimes inject steroids into an ankle joint to reduce pain and inflammation. However, this medication can weaken nearby tendons and has been associated with Achilles tendon ruptures.
- Certain antibiotics. Fluoroquinolone antibiotics, such as ciprofloxacin (Cipro) or levofloxacin (Levaquin), increase the risk of Achilles tendon rupture.
- Obesity. Excess weight puts more strain on the tendon.
Prevention
To reduce your chance of developing Achilles tendon problems, follow these tips:
- Stretch and strengthen calf muscles. Stretch your calf until you feel a noticeable pull but not pain. Don't bounce during a stretch. Calf-strengthening exercises can also help the muscle and tendon absorb more force and prevent injury.
- Vary your exercises. Alternate high-impact sports, such as running, with low-impact sports, such as walking, biking or swimming. Avoid activities that place excessive stress on your Achilles tendons, such as hill running and jumping activities.
- Choose running surfaces carefully. Avoid or limit running on hard or slippery surfaces. Dress properly for cold-weather training, and wear well-fitting athletic shoes with proper cushioning in the heels.
- Increase training intensity slowly. Achilles tendon injuries commonly occur after an abrupt increase in training intensity. Increase the distance, duration and frequency of your training by no more than 10 percent weekly.
Diagnosis
During the physical exam, your doctor will inspect your lower leg for tenderness and swelling. Your doctor might be able to feel a gap in your tendon if it has ruptured completely.
The doctor might ask you to kneel on a chair or lie on your stomach with your feet hanging over the end of the exam table. He or she might then squeeze your calf muscle to see if your foot will automatically flex. If it doesn't, you probably have ruptured your Achilles tendon.
If there's a question about the extent of your Achilles tendon injury — whether it's completely or only partially ruptured — your doctor might order an ultrasound or MRI scan. These painless procedures create images of the tissues of your body.
Treatment
Treatment for a ruptured Achilles tendon often depends on your age, activity level and the severity of your injury. In general, younger and more active people, particularly athletes, tend to choose surgery to repair a completely ruptured Achilles tendon, while older people are more likely to opt for nonsurgical treatment.
Recent studies, however, have shown fairly equal effectiveness of both surgical and nonsurgical management.
Nonsurgical treatment
This approach typically involves:
- Resting the tendon by using crutches
- Applying ice to the area
- Taking over-the-counter pain relievers
- Keeping the ankle from moving for the first few weeks, usually with a walking boot with heel wedges or a cast, with the foot flexed down
Nonoperative treatment avoids the risks associated with surgery, such as infection.
However, a nonsurgical approach might increase your chances of re-rupture and recovery can take longer, although recent studies indicate favorable outcomes in people treated nonsurgically if they start rehabilitation with weight bearing early.
Surgery
The procedure generally involves making an incision in the back of your lower leg and stitching the torn tendon together. Depending on the condition of the torn tissue, the repair might be reinforced with other tendons.
Complications can include infection and nerve damage. Minimally invasive procedures reduce infection rates over those of open procedures.
Rehabilitation
After either treatment, you'll have physical therapy exercises to strengthen your leg muscles and Achilles tendon. Most people return to their former level of activity within four to six months. It's important to continue strength and stability training after that because some problems can persist for up to a year.
A type of rehabilitation known as functional rehabilitation also focuses on coordination of body parts and how you move. The purpose is to return you to your highest level of performance, as an athlete or in your everyday life.
One review study concluded that if you have access to functional rehabilitation, you might do just as well with nonsurgical treatment as with surgery. More study is needed.
Rehabilitation after either surgical or nonsurgical management is also trending toward moving earlier and progressing faster. Studies are ongoing in this area also.
Preparing for your appointment
People with an Achilles tendon rupture commonly seek immediate treatment at a hospital's emergency department. You might also need to consult with doctors specializing in sports medicine or orthopedic surgery.
What you can do
Write a list that includes:
- Detailed descriptions of the symptoms and how and when the injury occurred
- Information about past medical problems
- All the medications and dietary supplements you take, including doses
- Questions to ask the doctor
What to expect from your doctor
The doctor may ask you some of the following questions:
- How did this injury occur?
- Did you feel or hear a popping or snapping sound when it happened?
- Can you stand on tiptoe on that foot?