Telangiectasia, Hereditary Hemorrhagic, Type 2
A number sign (#) is used with this entry because hereditary hemorrhagic telangiectasia type 2 (HHT2) is caused by mutation in the ACVRL1 gene (601284) on chromosome 12q13.
For a general phenotypic description and a discussion of genetic heterogeneity of this disorder, see HHT1 (187300).
Clinical FeaturesMcDonald et al. (2000) reported clinical features of a large kindred in which 38 members had HHT2 confirmed by genetic analysis (see 601284.0004 and Berg et al., 1997). Visceral findings of HHT2 included pulmonary arteriovenous malformations (PAVMs) (6%), cerebral AVM (7%), spinal AVM (3%), hepatic AVM (17%), gastrointestinal bleeding due to AVMs (11%), and cirrhosis (3%). Seventy-two percent of patients had onset of nosebleeds by age 15 years; however, there was overlap in frequency of epistaxis between mutation-negative and mutation-positive individuals. The findings illustrated the extreme phenotypic variability of HHT2 even in those with the same mutation.
Berg et al. (2003) performed a questionnaire-based study to delineate phenotypic differences between HHT1 and HHT2. The questionnaires were completed by 83 patients with known mutations (49 had HHT1 and 34 had HHT2). Patients with HHT1 reported an earlier onset of epistaxis and telangiectasis than those with HHT2. PAVMs were reported only in the group of HHT1 patients.
Abdalla et al. (2003) reported clinical data on 10 HHT2 families with known mutations in the ALK1 gene. They also summarized published data on patients and/or families with a known HHT2 genotype. Visceral manifestations were detected in 24 (26%) of 93 HHT2 patients from 9 of the families and included gastrointestinal bleeding (14%), intrahepatic shunts (6%), and arteriovenous malformations (AVMs) in the lung (4%) and brain (3%). Gastrointestinal bleeding, the most frequent visceral manifestation, was reported in 6 of the 10 families, mostly in patients over the age of 50. Identification of ALK1 mutations in subjects with a suspected diagnosis but without clinical signs of HHT argued in favor of molecular diagnosis. Visceral manifestations occurred in 27 of 44 reported families with HHT2, and affected 29% of HHT2 patients. This was considered an underestimate given incomplete and variable screening for lung, brain, and/or liver involvement in different clinical centers.
In affected members of a family with HHT2, Abdalla et al. (2003) identified a 1-bp insertion (1113insG) in the ACVRL1 gene (601284.0014). In 17 of 160 unrelated patients with HHT2, Lesca et al. (2004) identified the 1113insG mutation, which they referred to as a 1-bp duplication (1112dupG). The 17 patients shared a common haplotype and all originated from the Rhone-Alpes region of France, strongly suggesting a founder effect. Lesca et al. (2004) stated that the family reported by Abdalla et al. (2003) originated from the same region.
Rinaldi et al. (2011) described the ocular abnormalities in 8 affected members of a family segregating HHT2. Five patients (62.5%) had conjunctival telangiectases and 3 (37.5%) had retinal abnormalities, consisting mainly of choriocapillaris atrophy. Rinaldi et al. (2011) stated that this appeared to be the first report of the occurrence of choriocapillaris atrophy in HHT patients belonging to the same pedigree.
Canzonieri et al. (2014) examined the gastrointestinal tract of consecutive HHT patients to assess distribution, number, size, and type of telangiectases in relation to genotype. Twenty-two patients (13 men; mean age 59 +/- 9 years) were analyzed, 7 with HHT1 (187300), 13 with HHT2, and 2 undefined. Gastrointestinal telangiectases were identified in 86% of HHT1 patients and in 77% of HHT2 patients.
Wooderchak-Donahue et al. (2018) reported a 4-generation family in which 9 members had HHT2. All had epistaxis and characteristic telangiectases, and 6 of the 9 had PAVMs, 5 requiring treatment by transcatheter embolization.
HHT-Related Pulmonary Arterial Hypertension
Pulmonary hypertension that is clinically and histologically indistinguishable from primary pulmonary hypertension (see 178600) has been reported in a subset of patients with hereditary hemorrhagic telangiectasia (Trell et al., 1972).
Among 5 kindreds plus 1 individual patient with hereditary hemorrhagic telangiectasia, Trembath et al. (2001) identified 10 cases of pulmonary hypertension, including 5 patients with isolated clinical PPH and 5 with clinical evidence of both PPH and HHT. Only 2 of the 10 patients were found to have PAVMs. In affected members of 4 kindreds and in the individual patient, mutations were identified in the ALK1 gene. Two patients from 1 family had isolated PPH with mutation in the in the BMPR2 gene (600799). Trembath et al. (2001) noted that the pathophysiologic features of PPH and HHT seem to be distinct: in HHT, PAVMs lead to decreased pulmonary vascular resistance and increased cardiac output, with normal to low arterial pressures, whereas in PPH, obliteration of small pulmonary arteries leads to increased pulmonary artery pressures and decreased cardiac output. However, the histologic features of 4 patients with HHT and PPH showed pulmonary arterial lesions, including medial hypertrophy, intimal cellular proliferation, and plexiform lesions similar to those found in PPH1 patients with mutations in the BMPR2 gene. Trembath et al. (2001) postulated that the pulmonary abnormalities found in the 2 disorders are related to the TGF-beta signaling pathway in the pulmonary vascular endothelium.
MappingLinkage studies by Shovlin et al. (1994), Porteous et al. (1994), McAllister et al. (1994), and Heutink et al. (1994) indicated that in some families hereditary hemorrhagic telangiectasia is not linked to markers on 9q34. Furthermore, affected members of these families tended to escape pulmonary arteriovenous malformations, which tend to be a conspicuous feature of the 9q-linked form of HHT.
In 2 families with HHT unlinked to chromosome 9q, Vincent et al. (1995) found linkage to a series of genetic markers in the centromeric region of chromosome 12q. Using 2-point linkage analysis, a maximum lod score of 7.86 at theta = 0.05 was observed with the D12S85 microsatellite marker. In these 2 families, pulmonary arteriovenous malformations were absent.
Johnson et al. (1995) reported 4 families in which HHT was linked to markers mapping to the pericentromeric region of chromosome 12. Markers D12S85 and D12S339 showed the highest maximum combined lod scores of 9.06 (theta = 0.0) and 10.77 (theta = 0.04), respectively. By haplotype analysis, they identified an 11-cM candidate region bordered by D12S345 and D12S339. The experience in these families continued to support the previously reported observation of a significantly reduced incidence of pulmonary arteriovenous malformations in non-HHT1 families.
McAllister et al. (1994) observed 1 HHT family with suggestion of linkage to markers in the 3p22 region where the tumor growth factor-beta (TGFB type II) receptor (190182) is located. However, Johnson et al. (1995) stated that in the one family studied by McAllister et al. (1994), the 2-point lod score was 1.43 with marker D3S1211; stronger statistical support for linkage to the disease locus in this family was obtained for chromosome 12 (lod score = 2.64 at theta = 0.0 for marker D12S85), suggesting this as the actual location.
Johnson et al. (1996) reported a 4-cM interval for ORW2 on chromosome 12 and a 1.38-Mb YAC contig that spanned the entire interval. The contig included ACVRLK1, also symbolized ALK1, a member of the serine-threonine kinase receptor family expressed in endothelium.
Molecular GeneticsIn 3 families with HHT2, Johnson et al. (1996) identified mutations in the ALK1 gene (601284.0001-601284.0003). The finding suggested a critical role for ALK1 in the control of blood vessel development or repair.
Kjeldsen et al. (2001) used denaturing gradient gel electrophoresis (DGGE) to identify mutations in the ALK1 gene in 2 families with hereditary hemorrhagic telangiectasia. In a family with an ile398-to-asn mutation (I398N; 601284.0006) there was a high prevalence of pulmonary arteriovenous malformations and severe gastrointestinal bleeding, whereas in a family with an arg374-to-thr mutation (R374T; 601284.0007), no individuals had pulmonary arteriovenous malformations and only 1 patient had a history of severe gastrointestinal bleeding.
Wehner et al. (2006) identified mutations in 32 (62.7%) of 51 unrelated German patients with HHT. Thirteen mutations were in the ENG gene, consistent with HHT1, and 17 mutations were in the ACVRL1 gene, consistent with HHT2. Analysis of genotype/phenotype correlations was consistent with a more common frequency of PAVMs in patients with HHT1.
Olivieri et al. (2007) identified 50 different mutations in the ACVRL1 gene in 72 of 101 Italian patients with HHT. Twenty-six different ENG mutations were identified in 29 of the 101 patients. The findings were consistent with a higher frequency of ACVRL1 mutations compared to ENG mutations in HHT patients of Mediterranean ancestry.
In 4 of 45 probands with clinical HHT and negative results on direct sequencing, Shoukier et al. (2008) identified 4 different large heterozygous deletions involving the ACVRL1 gene using quantitative real-time polymerase chain reaction (qRT-PCR). The results were confirmed by multiplex ligation-dependent probe amplification (MLPA). Affected members of 2 families had deletion of the entire ACVRL1 gene. One of these deletions spanned at least 216 kb and included 5 neighboring genes, including ACVR1B (601300), GRASP (612027), and NR4A1 (139139). The proband who carried this large deletion had no additional symptoms besides HHT, indicating that heterozygous loss of these genes has no obvious phenotypic effect.
Using whole-genome sequencing of 35 patients with HHT among 13 families and next-generation sequencing of a custom panel of genes that had been associated with HHT among 87 unrelated patients with suspected HHT, Wooderchak-Donahue et al. (2018) identified 8 patients with novel noncoding heterozygous ACVRL1 gene variants that disrupt splicing. In 1 family (family 2), an affected mother and son had an ACVRL1 intron 9:chromosome 3 translocation, t(12,3)(q13,p21), the first reported translocation to cause HHT. In the other 7 families, the variants were located within an approximately 300-bp CT-rich hotspot region of intron 9 (see, e.g., 601284.0016) that disrupted splicing. The authors suggested that adding this region to HHT molecular diagnostic testing algorithms would improve clinical sensitivity.
HHT-Related Pulmonary Arterial Hypertension
In affected patients from 4 kindreds with HHT, PPH, or both, and in 1 patient with PPH and pulmonary AVMs, Trembath et al. (2001) identified mutations in the ALK1 gene (see, e.g., 601284.0008-601284.0010). No mutations in ALK1 were identified in 35 patients with isolated PPH.
In 8 unrelated probands with HHT2 and HHT-related pulmonary arterial hypertension, Harrison et al. (2003) identified 7 mutations, including 3 novel mutations, in the ALK1 gene (see, e.g., 601284.0011-601284.0013).
Genotype/Phenotype CorrelationsAmong 14 kindreds with HHT1 and 12 with HHT2 confirmed by genetic analysis, Bayrak-Toydemir et al. (2006) found that HHT2 was associated with later onset and more hepatic involvement than HHT1.
Among 18 German adults with HHT, Brakensiek et al. (2008) identified 9 mutations in the ACVRL1 gene and 7 in the ENG gene. Eight of the mutations were novel. Five of the 18 patients had liver involvement, including hepatomegaly, nodular hyperplasia, and massive arteriovenous shunts detected by imaging. All 5 of the patients with liver involvement had an ACVRL1 mutation, yielding a statistically significant difference in the distribution of ACVRL1 and ENG mutations among HHT patients with and without liver involvement (p = 0.0016). The positive predictive value for ACVRL1-positive patients to develop liver disease until the age of 52 years was estimated to be 68.4%. Brakensiek et al. (2008) concluded that molecular genetic testing of HHT patients is important for prognosis with respect to liver disease.
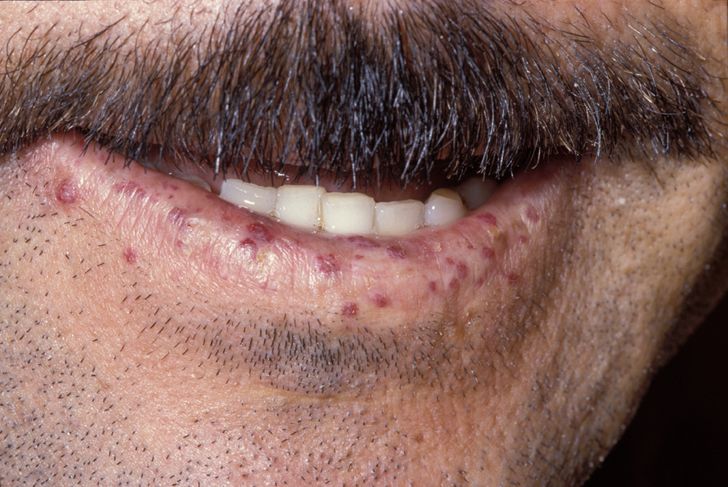
In a study of 268 Dutch patients with HHT1 and 130 Dutch patients with HHT2, Letteboer et al. (2008) found that oral and nasal mucosal telangiectases were present earlier in life in patients with HHT1 compared to patients with HHT2, whereas dermal lesions were more frequent and appeared earlier in life in patients with HHT2. In both groups, telangiectases of the nasal mucosa were present at a higher prevalence and started to appear earlier in life than those of the oral mucosa or dermal sites. The number of sites affected increased with age in both groups. In patients with HHT1, more women than men had skin telangiectases, particularly on the face. These results confirmed that the frequency of AVMs differ between patients with HHT1 and HHT2, and that these differences can be detected on physical examination.
Population GeneticsIn a large-scale French epidemiologic study, Bideau et al. (1989) found an average prevalence of HHT to be 1 in 8,345, which was more than 10 times higher than expected at that time. The distribution of the disease varied greatly from 1 area to another. Three French administrative areas had a far higher prevalence: Ain (1 in 3,345), Jura (1 in 5,062) and Deux-Sevres (1 in 4,287). Lesca et al. (2008) found that the 1112dupG mutation (601284.0014) was responsible for the very high frequency of the disease observed in the Ain and Jura administrative areas. The mutation was likely to have occurred in a common ancestor living in a valley of the Haut-Jura mountains more than 3 centuries ago and to have spread over the generations, mainly in the Rhone-Alpes region but also outside.
Animal ModelSrinivasan et al. (2003) created mice heterozygous for a loss-of-function mutation in Acvrl1 (601284). The mice developed age-dependent vascular lesions in the skin, extremities, oral cavity, and internal organs (lung, liver, intestine, spleen, and brain), as well as occult gastrointestinal bleeding. Major histopathologic features of the lesions included thin-walled dilated vessels in close proximity to each other, hemorrhage, and fibrosis. An Acvrl1 +/- mouse with profound liver involvement also displayed a secondary cardiac phenotype, similar to that observed in human patients.
Using a novel Acvrl1 null mutant mouse line in which a beta-galactosidase (see 230500) reporter gene (lacZ) was inserted into the Acvrl1 locus, Seki et al. (2003) showed that Acvrl1 was predominantly expressed in developing arterial, but not venous, endothelium. They concluded that, contrary to the view of HHT as a venous disease, their findings suggested that arterioles rather than venules are the primary vessels affected by the loss of an ACVRL1 allele.