Johanson-Blizzard Syndrome
Johanson-Blizzard syndrome (JBS) is a multiple congenital anomaly characterized by exocrine pancreatic insufficiency, hypoplasia/aplasia of the nasal alae, hypodontia, sensorineural hearing loss, growth retardation, anal and urogenital malformations, and variable intellectual disability.
Epidemiology
The prevalence of JBS in Europe has been estimated to be around 1/250,000 live births.
Clinical description
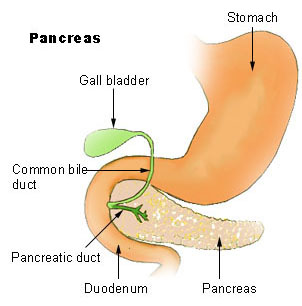
Onset of symptoms is usually during infancy with hallmark features being aplasia/hyposia of nasal alae and pancreatic exocrine insufficiency (presenting in the newborn or young infant with failure to thrive, oily stools and fat-soluble vitamin malabsorption). Additional features include dental anomalies (oligodontia/hypodontia (see these terms) of permanent teeth; >90%), sensorineural hearing loss (~75%), scalp defects (aplasia cutis congenital; ~65%), short stature (~60%), hypothyroidism (~40%), microcephaly (~35%), intrauterine growth restriction (~30%), genitourinary malformations (~30%; cryptorchidism, micropenis, hypospadias, clitoral hypertrophy/clitoromegaly, uterovaginal anomalies, hydronephrosis), congenital heart defects (25%; atrial and ventricular septal defects, patent arterial duct, tetralogy of Fallot, hypertrophic cardiomyopathy; see these terms), and imperforate anus (~20%). A presumably high risk for diabetes mellitus development during adolescence or adulthood has been reported. Developmental and intellectual delays of variable degree are present in ~60% of cases. Other frequent minor signs include abnormal frontal hair pattern (upsweep), lacrimal duct anomalies, severe facial clefting (cleft lip/palate) and lower eyelid coloboma. Less common features are natal teeth, tethered spinal cord, poly-/syndactyly of the feet, prostate aplasia, gastroesophageal reflux, cholestatic liver disease, café au-lait spots, growth hormone deficiency, hypopituitarism, brain malformations (e.g. arhinencephaly), situs inversus, and osseous malformations (left hip dislocation).
Etiology
Most cases of JBS are caused by mutations of UBR1 gene (15q13) which encodes a protein highly expressed in pancreatic acinar cells. UBR1 deficiency may contribute to gradual destruction of previously formed acinar cells starting prenatally, thereby leading to pancreatic enzymes deficiency.
Diagnostic methods
Diagnosis is based on identification of the pathognomonic combination of congenital or infantile exocrine pancreatic insufficiency (fecal fat quantification; fecal elastase; C-triglyceride breath test) with other characteristic anomalies such as aplasia/hyposia alae nasi. Diagnosis is confirmed by genetic screening of UBR1.
Differential diagnosis
Differential diagnosis includes cystic fibrosis, Shwachman-Diamond syndrome, Pearson Marrow-Pancreas syndrome, partial pancreatic agenesis (for congenital exocrine pancreatic insufficiency), oculodentodigital dysplasia (for hypoplasia of the alae nasi) and Adams-Oliver syndrome (for aplasia cutis congenita) (see these terms).
Antenatal diagnosis
Prenatal diagnosis is suspected by a beak-like nose (due to aplasia/hypoplasia of nasal alae) and a dilated sigmoid colon suggestive of imperforate anus at 21 weeks of gestation. Molecular testing of UBR1 confirms the diagnosis.
Genetic counseling
Transmission is autosomal recessive. Inter- rather than intrafamilial variability have been described.
Management and treatment
Treatment includes oral administration of exogenous pancreatic enzymes and nutritional support (high-calorie diet with 30-40% calories from fat, lipase, fat-soluble vitamins and mineral supplementation) for pancreatic insufficiency; thyroid hormone substitution; surgery for anorectal and genitourinary malformations; hearing aids for deafness; insulin for diabetes mellitus; early intervention programs and specific education for patients with intellectual disabilities; and dental implantation during the teenage years. Facial malformations may be corrected by plastic surgery.
Prognosis
Pancreatic insufficiency and complications of severe malnutrition (e.g. severe hypoproteinemia, vitamin deficiency, immunodeficiency) may lead to death in infancy or early childhood. For patients managed appropriately, survival into adulthood is the rule.