Pemphigoid Gestationis
A rare autoimmune bullous skin disease characterized by pruritus with or without polymorphic skin eruptions, affecting pregnant women typically during the second and third trimester. Skin eruptions may include erythematous papules and plaques, erythema multiforme-like or eczematous lesions, papulovesicles, and bullae, and typically affect the umbilicus, abdomen, and extremities.
Epidemiology
The estimated incidence ranges between 1/3,000-60,000 pregnancies.
Clinical description
Pemphigoid gestationis (PG) Pemphoid gestationis (PG) typically presents during the second or third trimesters, although onset during the first trimester and postpartum is possible. Pruritus can be the presenting symptom and may remain the only symptom. Clinical presentation typically includeEruptive skin lesions occur as urticarial papules and annular plaques, erythema multiform-like changes, eczematous lesions, or papulofollowed byvesicles that, and in some cases may develop into large tense blisters. Lesionsbullae. Skin lesions first erupt around the umbilicus and subsequently spread to the abdomen and the extremities. The mucous membranes and the face are typically spared. The clinical course is fairly benign andOccasionally, concomitant general symptoms, such as fatigue, subfebrile temperatures, shivers, and stress, occur. PG typically resolves with an average duration of 4-6weeks to months of onset. A flare may occur immediately after delivery but typically resolves within 4 weeks. Recurrence in subsequent pregnancies is common (35-50%), and is typically more severe with earlier onset. PG is associated with the autoimmune Graves' disease in the mother. There is an increased risk of small-for-gestational-age baby, premature birth, and development of mild, self-limiting skin lesions in the neonate (10-11%). PG can be associated with the autoimmune Graves' disease in the mother.
Etiology
PG is caused by production of anti-BP180 IgG antibodies that result from antigen presentation by MHC class II molecules aberrantly expressed on amniochorionic stromal cells and on the trophoblast. PG is strongly associated with maternal MHC class II antigens haplotypes HLA-DR3 and HLA-DR4.
Diagnostic methods
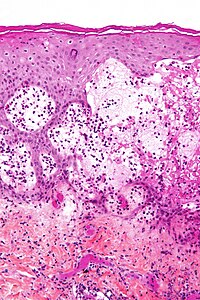
Clinical and histological features are not specific to PG; therefore, additional tests are required for diagnosis. Direct immunofluorescence demonstrates a linear deposition of C3 (complement 3) and IgG autoantibodies at the dermal-epidermaldermoepidermal junction as. C3 is reported in bullous pemphigoid100% of cases, while IgG is seen in 25%-50% of cases. Indirect immunofluroescence detects serum IgG autoantibodies targeting the basement membrane of the skin in 30%-100% of cases. ELISA (enzyme-linked immunosorbent assay) can reveal circulating IgG antibodies against BP180.
Differential diagnosis
Differential diagnosis includes atopic eruption of pregnancy, polymorphic eruption of pregnancy, and intrahepatic cholestasis of pregnancy, herpes virus infection, urticaria, drug hypersensitivity reactions, contact dermatitis and other eczemas, pityriasis rosea, pityriasis versicolor, yeast folliculitis as well as other types of folliculitis, miliaria, and scabies.
Management and treatment
Most patients are controlledMild cases can be treated with potentclass III or super-potentIV topical corticosteroids in combination with H1-receptor antagonists such as cetirizin. In more severe cases, oral corticosteroids are necessary. Preferred corticosteroids are prednisone and prednisolone. Minimum effective doses should be used to reduce the risk of side effects, and gradually tapered to a lower maintenance dose. If exacerbation in the peripartum period occurs, the maintenance dose can be increased. Ultraviolet light therapy is relatively contraindicated. In unresponsive cases, patients may benefit from systemic immunoadsorption, or intravenous immunoglobulin. In cases of persisting (postnatal) symptoms, systemic immunosuppressants might be beneficial.
Prognosis
The disease is typically self-limiting; however, onset in the first or second trimester and presence of blisters is associated with adverse pregnancy outcomes. Recurrence in subsequent pregnancies is common (35-50%), and is typically more severe with earlier onset. The disease can persist and converts to bullous pemphigoid (in less than 5% of patients).