Sarcosinemia
A number sign (#) is used with this entry because of evidence that sarcosinemia (SARCOS) is caused by homozygous or compound heterozygous mutation in the SARDH gene (604455) on chromosome 9q34.
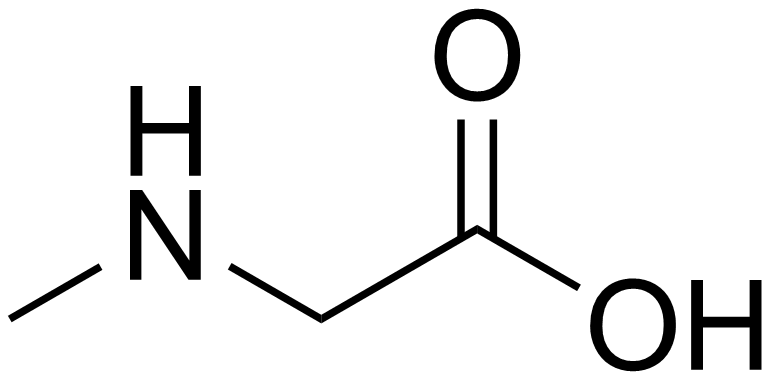
DescriptionSarcosinemia is characterized by an increased concentration of sarcosine in plasma and an increased excretion of sarcosine in urine. Sarcosine (N-methylglycine) is enzymatically formed from dimethylglycine by dimethylglycine dehydrogenase (EC 1.5.99.2) and converted to glycine by sarcosine dehydrogenase (SARDH; 604455; EC 1.5.99.1). Some reports have associated sarcosinemia with mental retardation and neurologic problems, but the disorder is most likely benign and unrelated to significant clinical problems (summary by Scott, 2001).
Clinical FeaturesGerritsen and Waisman (1966) found hypersarcosinemia and sarcosinuria in brother and sister with mild mental retardation and few other abnormalities. Abnormal increases in blood and urine sarcosine occurred in 2 other sibs, the mother, a maternal aunt, and the maternal grandmother (but not in the father) when sarcosine or its precursor dimethylglycine were administered.
Scott et al. (1970) reported a patient with sarcosinemia who had motor and mental retardation. They found, by loading tests, a decreased capacity to convert sarcosine to glycine, suggesting a deficiency of sarcosine dehydrogenase activity. They concluded that sarcosinemia is a benign metabolic state with no clinical manifestations. They viewed earlier impressions to the contrary as the result of bias of ascertainment, i.e., the discovery of sarcosinemia in children being investigated for abnormalities.
Levy et al. (1984) reported 4 patients with sarcosinemia who were detected by routine neonatal screening. All of the patients were mentally normal with no dysmorphic or other abnormal features.
Sewell et al. (1986) stated that 16 cases of sarcosinemia had been reported. They reported sarcosinemia in a retarded, amaurotic child of Turkish ancestry.
Meissner and Mayatepek (1997) reported the case of a 22-year-old woman who at the age of 5 years developed the first symptoms of sarcosinemia in the form of progressive loss of speech ability. One year later, she developed neurologic symptoms, including muscular hypotonia, pyramidal tract signs with unaffected sensation, paresis of the peroneal nerve, and subsequently ataxia. At that time, gross elevations of the concentration of sarcosine in plasma and urine were detected. By the age of 7 years she was no longer able to walk, finally resulting in complete tetraparesis at 15 years of age. At that time, she lost her speech totally, and bilateral optic atrophy became prominent. At the age of 18 years, she developed tonic-clonic seizures. MRI showed general cerebral atrophy. At the age of 20 years, echocardiography revealed biventricular hypertrophic cardiomyopathy with functional infundibular pulmonic stenosis and reduced pulmonary outflow. The severe symptoms had not been reported previously in association with sarcosinemia. The possibility of a second disorder was raised since generally sarcosinemia is a completely benign condition. Meissner and Mayatepek (1997) commented that, since more than a single enzyme defect may be responsible for sarcosinemia, different clinical phenotypes may exist, including at least some patients with neurologic and other severe clinical symptoms.
Sarcosinemia and sarcosinuria also occur in some patients with type II glutaric aciduria (see 231675 and 231680) and with severe deficiency of folic acid (Scott, 2001).
Population GeneticsLevy et al. (1984) found that the incidence of sarcosinemia identified by newborn screening in Massachusetts was 1/350,000.
In the Saguenay-Lac-Saint-Jean region of Quebec province, De Braekeleer (1991) estimated the prevalence at birth of sarcosinemia to be 1 in 3,414, giving a carrier frequency of 1 in 29.
Molecular GeneticsIn 4 individuals from 3 consanguineous Israeli Arab families and 3 individuals from 3 French families who had elevated levels of sarcosine in blood and urine, Bar-joseph et al. (2012) sequenced the SARDH gene and identified homozygous or compound heterozygous mutations in 3 families (604455.0001-604455.0004). In 1 French family, they found a uniparental disomy in the region of the SARDH gene. No mutation in the SARDH gene was found in 2 of the Israeli Arab families, suggesting genetic heterogeneity.
Animal ModelBy screening the progeny of ethylnitrosourea-mutagenized mice for amino acidurias, Harding et al. (1992) identified a mouse mutant with sarcosinemia. Urinary sarcosine levels were in the upper range of those observed in humans with this disorder. Sarcosine dehydrogenase activity was deficient. The sarcosinuria phenotype in these mice was inherited as an autosomal recessive. In the mouse as in the human, homozygous sarcosine dehydrogenase deficiency is apparently benign.