Axenfeld-Rieger Syndrome
Axenfeld-Rieger syndrome (ARS) is a generic term used to designate overlapping genetic disorders, in which the major physical condition is anterior segment dysgenesis of the eye. Patients with ARS may also present with multiple variable congenital anomalies.
Epidemiology
The syndrome has an estimated prevalence of 1/200,000.
Clinical description
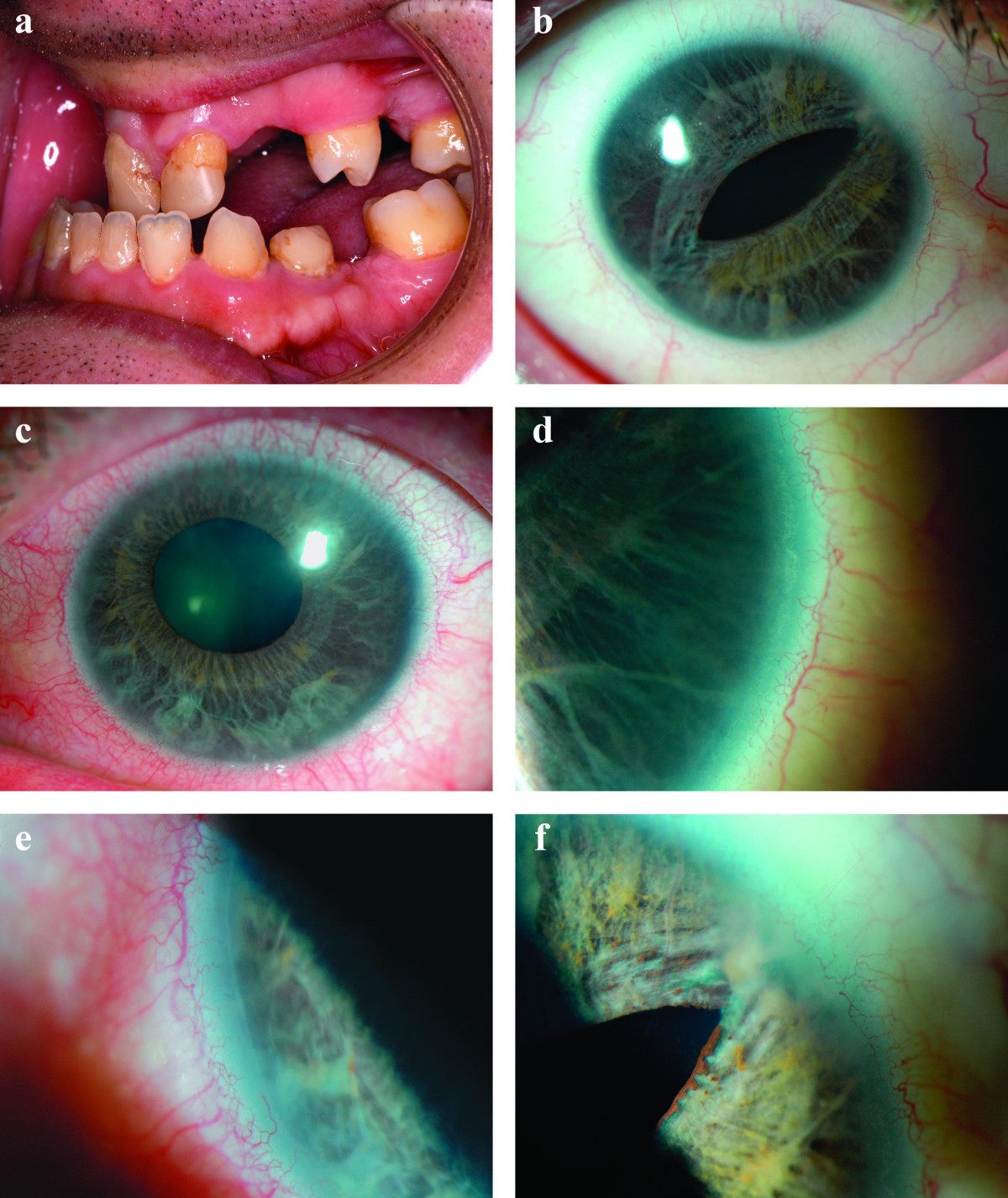
The clinical manifestations of ARS are highly variable. Features can be divided into ocular and non-ocular findings. Ocular abnormalities mainly affect the iris: hypoplasia, corectopia or hole formation in the iris mimicking polycoria; cornea: prominent and anteriorly displaced Schwalbe's line (posterior embryotoxon); and the chamber angle: iris strands bridging the iridocorneal angle to the trabecular meshwork. Eye dysgenesis in ARS may cause increased ocular pressure (IOP) leading to glaucoma. Glaucoma can develop in infancy, but usually occurs in adolescence or early adulthood, occasionally after middle age. The most characteristic non-ocular findings are mild craniofacial dysmorphism, dental anomalies and redundant periumblical skin. Mid-face abnormalities include hypertelorism, telecanthus, maxillary hypoplasia with flattening of the mid-face, prominent forehead, and broad, flat nasal bridge. Dental abnormalities may include microdontia or hypodontia. Hypospadias in males, anal stenosis, pituitary abnormalities and growth retardation may also be observed.
Etiology
Patients with ARS have been found to have mutations in the transcription factor genes PITX2 (4q25) and FOXC1 (6p25). A large number of different mutations have been identified but there is no clear genotype-phenotype relationship. However, PITX2 mutations are mainly detected in ARS patients with non-ocular changes. The underlying genetic defect is unknown in 60% of cases, and at least two more loci have been associated with ARS.
Diagnostic methods
ARS is diagnosed by ophthalmologic and clinical examination. Associated systemic findings are supportive of diagnosis. Genetic testing can be used to confirm the diagnosis.
Differential diagnosis
Differential diagnoses include iris hypoplasia (IH), primary congenital glaucoma (PCG) and Peters anomaly (see these terms). Absence of other corneal abnormalities, such as megalocornea, sclerocornea and corneal opacity are useful in distinguishing ARS from other anterior segment disorders.
Antenatal diagnosis
If the disease-causing mutation has been identified in a family, prenatal testing for at-risk pregnancies is possible.
Genetic counseling
The disorders that comprise the ARS spectrum are inherited in an autosomal dominant manner with high penetrance. Genetic counseling can be offered to patients and their families.
Management and treatment
An annual slit lamp examination should be performed, along with gonioscopy, IOP measurements and funduscopy to assess the retinal nerve fiber layer and optic nerve head involvement due to possible glaucoma. Autoperimetry (automated measurements of the visual fields) is necessary whenever glaucoma is suspected. Should glaucoma develop, drug therapy is recommended before surgery. In case of glaucoma, the goal of treatment is to reach low IOP. Surgery is performed if eye drops are not sufficient in lowering IOP. Medications that decrease aqueous output (beta-blockers, alpha-agonists and carbonic anhydrase inhibitors) are more beneficial than those affecting outflow. However, alpha-agonists should be used with caution in young children because of possible CNS depression. If surgery is necessary, the procedure of choice is trabeculectomy with the adjunctive use of antimetabolites. If photophobia is present in patients with corectopia and polycoria, contact lenses may be used to cover the holes in the iris.
Prognosis
Prognosis is good, particularly in the absence of glaucoma.