Spanish Flu

The Spanish flu, also known as the 1918 flu pandemic, was an unusually deadly influenza pandemic caused by the H1N1 influenza A virus. Lasting from February 1918 to April 1920, it infected 500 million people – about a third of the world's population at the time – in four successive waves. The death toll is typically estimated to have been somewhere between 20 million and 50 million, although estimates range from a conservative 17 million to a possible high of 100 million, making it one of the deadliest pandemics in human history.
The first observations of illness and mortality were documented in the United States (in Kansas) in March 1918 and then in April in France, Germany and the United Kingdom. To maintain morale, World War I censors minimized these early reports. Newspapers were free to report the epidemic's effects in neutral Spain, such as the grave illness of King Alfonso XIII, and these stories created a false impression of Spain as especially hard hit. This gave rise to the name "Spanish" flu. Historical and epidemiological data are inadequate to identify with certainty the pandemic's geographic origin, with varying views as to its location.
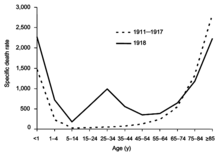
Most influenza outbreaks disproportionately kill the very young and the very old, with a higher survival rate for those in between, but the Spanish flu pandemic resulted in a higher-than-expected mortality rate for young adults. Scientists offer several possible explanations for the high mortality rate of the 1918 influenza pandemic, including a severe 6-year climate anomaly that affected the migration of disease vectors and increased the likelihood of the spread of the disease through bodies of water. Some analyses have shown the virus to be particularly deadly because it triggers a cytokine storm, which ravages the stronger immune system of young adults. In contrast, a 2007 analysis of medical journals from the period of the pandemic found that the viral infection was no more aggressive than previous influenza strains. Instead, malnourishment, overcrowded medical camps and hospitals, and poor hygiene, all exacerbated by the recent war, promoted bacterial superinfection. This superinfection killed most of the victims, typically after a somewhat prolonged death bed.
The 1918 Spanish flu was the first of two pandemics caused by H1N1 influenza A virus; the second was the 2009 swine flu pandemic.
Etymology
Although its geographic origin is unknown, the disease was called Spanish flu as early as the first wave of the pandemic. Spain was not involved in the war, having remained neutral, and had not imposed wartime censorship. Newspapers were therefore free to report the epidemic's effects, such as the grave illness of King Alfonso XIII, and these widely-spread stories created a false impression of Spain as especially hard hit.
Alternative names were also used at the time of the pandemic. Similar to the name of Spanish flu, many of these also alluded to the purported origins of the disease. In Senegal it was named 'the Brazilian flu', and in Brazil 'the German flu', while in Poland it was known as 'the Bolshevik disease'. In Spain itself, the nickname for the flu, the "Naples Soldier", was adopted from a 1916 operetta, The Song of Forgetting (La canción del olvido) after one of the librettists quipped that the play's most popular musical number, Naples Soldier, was as catchy as the flu. Today, however, 'Spanish flu' (Gripe Española) is the most widely used name for the pandemic in Spain.
Other terms for this virus include the "1918 influenza pandemic," the "1918 flu pandemic", or variations of these.
History
Timeline
First wave of early 1918
The pandemic is conventionally marked as having begun on 4 March 1918 with the recording of the case of Albert Gitchell, an army cook at Camp Funston in Kansas, United States, despite there likely having been cases before him. The disease had been observed in Haskell County in January 1918, prompting local doctor Loring Miner to warn the US Public Health Service's academic journal. Within days, 522 men at the camp had reported sick. By 11 March 1918, the virus had reached Queens, New York. Failure to take preventive measures in March/April was later criticized.
As the US had entered World War I, the disease quickly spread from Camp Funston, a major training ground for troops of the American Expeditionary Forces, to other US Army camps and Europe, becoming an epidemic in the Midwest, East Coast, and French ports by April 1918, and reaching the Western Front by the middle of the month. It then quickly spread to the rest of France, Great Britain, Italy, and Spain and in May reached Breslau and Odessa. After the signing of the Treaty of Brest-Litovsk (March 1918), Germany started releasing Russian prisoners of war, who then brought the disease to their country. It reached North Africa, India, and Japan in May, and soon after had likely gone around the world as there had been recorded cases in Southeast Asia in April. In June an outbreak was reported in China. After reaching Australia in July, the wave started to recede.
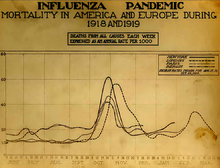
The first wave of the flu lasted from the first quarter of 1918 and was relatively mild. Mortality rates were not appreciably above normal; in the United States ~75,000 flu-related deaths were reported in the first six months of 1918, compared to ~63,000 deaths during the same time period in 1915. In Madrid, Spain, fewer than 1,000 people died from influenza between May and June 1918. There were no reported quarantines during the first quarter of 1918. However, the first wave caused a significant disruption in the military operations of World War I, with three-quarters of French troops, half the British forces, and over 900,000 German soldiers sick.

Deadly second wave of late 1918
The second wave began in the second half of August, probably spreading to Boston and Freetown, Sierra Leone, by ships from Brest, where it had likely arrived with American troops or French recruits for naval training. From the Boston Navy Yard and Camp Devens (later renamed Fort Devens), about 30 miles west of Boston, other U.S. military sites were soon afflicted, as were troops being transported to Europe. Helped by troop movements, it spread over the next two months to all of North America, and then to Central and South America, also reaching Brazil and the Caribbean on ships. In July 1918, the Ottoman Empire saw its first cases in some soldiers. From Freetown, the pandemic continued to spread through West Africa along the coast, rivers, and the colonial railways, and from railheads to more remote communities, while South Africa received it in September on ships bringing back members of the South African Native Labour Corps returning from France. From there it spread around southern Africa and beyond the Zambezi, reaching Ethiopia in November. On September 15, New York City saw its first fatality from influenza. The Philadelphia Liberty Loans Parade, held in Philadelphia, Pennsylvania, on 28 September 1918 to promote government bonds for World War I, resulted in 12,000 deaths after a major outbreak of the illness spread among people who had attended the parade.
From Europe, the second wave swept through Russia in a southwest–northeast diagonal front, as well as being brought to Arkhangelsk by the North Russia intervention, and then spread throughout Asia following the Russian Civil War and the Trans-Siberian railway, reaching Iran (where it spread through the holy city of Mashhad), and then later India in September, as well as China and Japan in October. The celebrations of the Armistice of 11 November 1918 also caused outbreaks in Lima and Nairobi, but by December the wave was mostly over.

The second wave of the 1918 pandemic was much more deadly than the first. The first wave had resembled typical flu epidemics; those most at risk were the sick and elderly, while younger, healthier people recovered easily. October 1918 was the month with the highest fatality rate of the whole pandemic. In the United States, ~292,000 deaths were reported between September–December 1918, compared to ~26,000 during the same time period in 1915. The Netherlands reported 40,000+ deaths from influenza and acute respiratory disease. Bombay reported ~15,000 deaths in a population of 1.1 million. The 1918 flu pandemic in India was especially deadly, with an estimated 12.5–20 million deaths in the last quarter of 1918 alone.
Third wave of 1919
In January 1919, a third wave of the Spanish Flu hit Australia, where it killed 12,000 following the lifting of a maritime quarantine, and then spread quickly through Europe and the United States, where it lingered through the Spring and until June 1919. It primarily affected Spain, Serbia, Mexico and Great Britain, resulting in hundreds of thousands of deaths. It was less severe than the second wave but still much more deadly than the initial first wave. In the United States, isolated outbreaks occurred in some cities including Los Angeles, New York City, Memphis, Nashville, San Francisco and St. Louis. Overall American mortality rates were in the tens of thousands during the first six months of 1919.
Fourth wave of 1920
In spring 1920, a fourth wave occurred in isolated areas including New York City, Switzerland, Scandinavia, and some South American islands. New York City alone reported 6,374 deaths between December 1919 and April 1920, almost twice the number of the first wave in spring 1918. Other US cities including Detroit, Milwaukee, Kansas City, Minneapolis and St. Louis were hit particularly hard, with death rates higher than all of 1918. Peru experienced a late wave in early 1920, and Japan had one from late 1919 to 1920, with the last cases in March. In Europe, five countries (Spain, Denmark, Finland, Germany and Switzerland) recorded a late peak between January–April 1920.

Potential origins
Despite its name, historical and epidemiological data cannot identify the geographic origin of the Spanish flu. However, several theories have been proposed.
United States
The first confirmed cases originated in the United States. Historian Alfred W. Crosby stated in 2003 that the flu originated in Kansas, and popular author John M. Barry described a January 1918 outbreak in Haskell County, Kansas, as the point of origin in his 2004 article.
A 2018 study of tissue slides and medical reports led by evolutionary biology professor Michael Worobey found evidence against the disease originating from Kansas, as those cases were milder and had fewer deaths compared to the infections in New York City in the same period. The study did find evidence through phylogenetic analyses that the virus likely had a North American origin, though it was not conclusive. In addition, the haemagglutinin glycoproteins of the virus suggest that it originated long before 1918, and other studies suggest that the reassortment of the H1N1 virus likely occurred in or around 1915.
Europe
The major UK troop staging and hospital camp in Étaples in France has been theorized by virologist John Oxford as being at the center of the Spanish flu. His study found that in late 1916 the Étaples camp was hit by the onset of a new disease with high mortality that caused symptoms similar to the flu. According to Oxford, a similar outbreak occurred in March 1917 at army barracks in Aldershot, and military pathologists later recognized these early outbreaks as the same disease as the Spanish flu. The overcrowded camp and hospital was an ideal environment for the spread of a respiratory virus. The hospital treated thousands of victims of poison gas attacks, and other casualties of war, and 100,000 soldiers passed through the camp every day. It also was home to a piggery, and poultry was regularly brought in from surrounding villages to feed the camp. Oxford and his team postulated that a precursor virus, harbored in birds, mutated and then migrated to pigs kept near the front.
A report published in 2016 in the Journal of the Chinese Medical Association found evidence that the 1918 virus had been circulating in the European armies for months and possibly years before the 1918 pandemic. Political scientist Andrew Price-Smith published data from the Austrian archives suggesting the influenza began in Austria in early 1917.
A 2009 study in Influenza and Other Respiratory Viruses found that Spanish flu mortality simultaneously peaked within the two-month period of October and November 1918 in all fourteen European countries analyzed, which is inconsistent with the pattern that researchers would expect if the virus had originated somewhere in Europe and then spread outwards.
China
In 1993, Claude Hannoun, the leading expert on the Spanish flu at the Pasteur Institute, asserted the precursor virus was likely to have come from China and then mutated in the United States near Boston and from there spread to Brest, France, Europe's battlefields, the rest of Europe, and the rest of the world, with Allied soldiers and sailors as the main disseminators. Hannoun considered several alternative hypotheses of origin, such as Spain, Kansas, and Brest, as being possible, but not likely. In 2014, historian Mark Humphries argued that the mobilization of 96,000 Chinese laborers to work behind the British and French lines might have been the source of the pandemic. Humphries, of the Memorial University of Newfoundland in St. John's, based his conclusions on newly unearthed records. He found archival evidence that a respiratory illness that struck northern China (where the laborers came from) in November 1917 was identified a year later by Chinese health officials as identical to the Spanish flu. However, no tissue samples have survived for modern comparison. Nevertheless, there were some reports of respiratory illness on parts of the path the laborers took to get to Europe, which also passed through North America.
One of the few regions of the world seemingly less affected by the Spanish flu pandemic was China, where several studies have documented a comparatively mild flu season in 1918. (Although this is disputed due to lack of data during the Warlord Period, see Around the globe.) This has led to speculation that the Spanish flu pandemic originated in China, as the lower rates of flu mortality may be explained by the Chinese population's previously acquired immunity to the flu virus.
A report published in 2016 in the Journal of the Chinese Medical Association found no evidence that the 1918 virus was imported to Europe via Chinese and Southeast Asian soldiers and workers and instead found evidence of its circulation in Europe before the pandemic. The 2016 study suggested that the low flu mortality rate (an estimated one in a thousand) found among the Chinese and Southeast Asian workers in Europe meant that the deadly 1918 influenza pandemic could not have originated from those workers. Further evidence against the disease being spread by Chinese workers was that workers entered Europe through other routes that did not result in a detectable spread, making them unlikely to have been the original hosts.
Epidemiology and pathology
Transmission and mutation

The basic reproduction number of the virus was between 2 and 3. The close quarters and massive troop movements of World War I hastened the pandemic, and probably both increased transmission and augmented mutation. The war may also have reduced people's resistance to the virus. Some speculate the soldiers' immune systems were weakened by malnourishment, as well as the stresses of combat and chemical attacks, increasing their susceptibility. A large factor in the worldwide occurrence of the flu was increased travel. Modern transportation systems made it easier for soldiers, sailors, and civilian travelers to spread the disease. Another was lies and denial by governments, leaving the population ill-prepared to handle the outbreaks.
The severity of the second wave has been attributed to the circumstances of the First World War. In civilian life, natural selection favors a mild strain. Those who get very ill stay home, and those mildly ill continue with their lives, preferentially spreading the mild strain. In the trenches, natural selection was reversed. Soldiers with a mild strain stayed where they were, while the severely ill were sent on crowded trains to crowded field hospitals, spreading the deadlier virus. The second wave began, and the flu quickly spread around the world again. Consequently, during modern pandemics, health officials look for deadlier strains of a virus when it reaches places with social upheaval. The fact that most of those who recovered from first-wave infections had become immune showed that it must have been the same strain of flu. This was most dramatically illustrated in Copenhagen, which escaped with a combined mortality rate of just 0.29% (0.02% in the first wave and 0.27% in the second wave) because of exposure to the less-lethal first wave. For the rest of the population, the second wave was far more deadly; the most vulnerable people were those like the soldiers in the trenches – adults who were young and fit.
After the lethal second wave struck in late 1918, new cases dropped abruptly. In Philadelphia, for example, 4,597 people died in the week ending 16 October, but by 11 November, influenza had almost disappeared from the city. One explanation for the rapid decline in the lethality of the disease is that doctors became more effective in the prevention and treatment of pneumonia that developed after the victims had contracted the virus. However, John Barry stated in his 2004 book The Great Influenza: The Epic Story of the Deadliest Plague In History that researchers have found no evidence to support this position. Another theory holds that the 1918 virus mutated extremely rapidly to a less lethal strain. Such evolution of influenza is a common occurrence: there is a tendency for pathogenic viruses to become less lethal with time, as the hosts of more dangerous strains tend to die out. Some fatal cases did continue into March 1919, killing one player in the 1919 Stanley Cup Finals.
Signs and symptoms
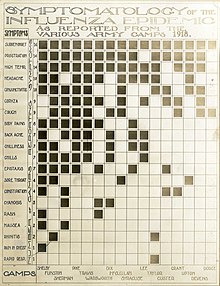
The majority of the infected experienced only the typical flu symptoms of sore throat, headache, and fever, especially during the first wave. However, during the second wave the disease was much more serious, often complicated by bacterial pneumonia, which was often the cause of death. This more serious type would cause heliotrope cyanosis to develop, whereby the skin would first develop two mahogany spots over the cheekbones which would then over a few hours spread to color the entire face blue, followed by black coloration first in the extremities and then further spreading to the limbs and the torso. After this, death would follow within hours or days due to the lungs being filled with fluids. Other signs and symptoms reported included spontaneous mouth and nosebleeds, miscarriages for pregnant women, a peculiar smell, teeth, and hair falling, delirium, dizziness, insomnia, loss of hearing or smell, blurred vision, and impaired color vision. One observer wrote, "One of the most striking of the complications was hemorrhage from mucous membranes, especially from the nose, stomach, and intestine. Bleeding from the ears and petechial hemorrhages in the skin also occurred". The severity of the symptoms was believed to be caused by cytokine storms.
The majority of deaths were from bacterial pneumonia, a common secondary infection associated with influenza. This pneumonia was itself caused by common upper respiratory-tract bacteria, which were able to get into the lungs via the damaged bronchial tubes of the victims. The virus also killed people directly by causing massive hemorrhages and edema in the lungs. Modern analysis has shown the virus to be particularly deadly because it triggers a cytokine storm (overreaction of the body's immune system). One group of researchers recovered the virus from the bodies of frozen victims and transfected animals with it. The animals suffered rapidly progressive respiratory failure and death through a cytokine storm. The strong immune reactions of young adults were postulated to have ravaged the body, whereas the weaker immune reactions of children and middle-aged adults resulted in fewer deaths among those groups.
Misdiagnosis
Because the virus that caused the disease was too small to be seen under a microscope at the time, there were problems with correctly diagnosing it. The bacterium Haemophilus influenzae was instead mistakenly thought to be the cause, as it was big enough to be seen and was present in many, though not all, patients. For this reason, a vaccine that was used against that bacillus did not make an infection rarer but did decrease the death rate.
During the deadly second wave there were also fears that it was in fact plague, dengue fever, or cholera. Another common misdiagnosis was typhus, which was common in circumstances of social upheaval, and was therefore also affecting Russia in the aftermath of the October Revolution. In Chile, the view of the country's elite was that the nation was in severe decline, and therefore the assumption of doctors was that the disease was typhus caused by poor hygiene, and not an infectious one, causing a mismanaged response which did not ban mass gatherings.
The role of climate conditions
Studies have shown that the immune system of Spanish flu victims was weakened by adverse climate conditions which were particularly unseasonably cold and wet for extended periods of time during the duration of the pandemic. This affected especially WWI troops exposed to incessant rains and lower-than-average temperatures for the duration of the conflict, and especially during the second wave of the pandemic. Ultra-high-resolution climate data combined with highly detailed mortality records analyzed at Harvard University and the Climate Change Institute at the University of Maine identified a severe climate anomaly that impacted Europe from 1914 to 1919, with several environmental indicators directly influencing the severity and spread of the Spanish flu pandemic. Specifically, a significant increase in precipitation affected all of Europe during the second wave of the pandemic, from September to December 1918. Mortality figures follow closely the concurrent increase in precipitation and decrease in temperatures. Several explanations have been proposed for this, including the fact that lower temperatures and increased precipitation provided ideal conditions for virus replication and transmission, while also negatively affecting the immune systems of soldiers and other people exposed to the inclement weather, a factor proven to increase likelihood of infection by both viruses and pneumococcal co-morbid infections documented to have affected a large percentage of pandemic victims (one fifth of them, with a 36% mortality rate). A six-year climate anomaly (1914–1919) brought cold, marine air to Europe, drastically changing its weather, as documented by eyewitness accounts and instrumental records, reaching as far as the Gallipoli campaign, in Turkey, where ANZAC troops suffered extremely cold temperatures despite the normally Mediterranean climate of the region. The climate anomaly likely influenced the migration of H1N1 avian vectors which contaminate bodies of water with their droppings, reaching 60% infection rates in autumn. The climate anomaly has been associated with an anthropogenic increase in atmospheric dust, due to the incessant bombardment; increased nucleation due to dust particles (cloud condensation nuclei) contributed to increased precipitation.
Responses
Public health management
While systems for alerting public health authorities of infectious spread did exist in 1918, they did not generally include influenza, leading to a delayed response. Nevertheless, actions were taken. Maritime quarantines were declared on islands such as Iceland, Australia, and American Samoa, saving many lives. Social distancing measures were introduced, for example closing schools, theatres, and places of worship, limiting public transportation, and banning mass gatherings. Wearing face masks became common in some places, such as Japan, though there were debates over their efficacy. There was also some resistance to their use, as exemplified by the Anti-Mask League of San Francisco. Vaccines were also developed, but as these were based on bacteria and not the actual virus, they could only help with secondary infections. The actual enforcement of various restrictions varied. To a large extent, the New York City health commissioner ordered businesses to open and close on staggered shifts to avoid overcrowding on the subways.
A later study found that measures such as banning mass gatherings and requiring the wearing of face masks could cut the death rate up to 50 percent, but this was dependent on them being imposed early in the outbreak and not being lifted prematurely.
Medical treatment
As there were no antiviral drugs to treat the virus, and no antibiotics to treat the secondary bacterial infections, doctors would rely on a random assortment of medicines with varying degrees of effectiveness, such as aspirin, quinine, arsenics, digitalis, strychnine, epsom salts, castor oil, and iodine. Treatments of traditional medicine, such as bloodletting, ayurveda, and kampo were also applied.
Information dissemination
Due to World War I, many countries engaged in wartime censorship, and suppressed reporting of the pandemic. For example, the Italian newspaper Corriere della Sera was prohibited from reporting daily death tolls. The newspapers of the time were also generally paternalistic and worried about mass panic. Misinformation would also spread along with the disease. In Ireland there was a belief that noxious gases were rising from the mass graves of Flanders Fields and being "blown all over the world by winds". There were also beliefs that the Germans were behind it, for example by poisoning the aspirin manufactured by Bayer, or by releasing poison gas from U-boats.
Mortality
Around the globe

The Spanish flu infected around 500 million people, about one-third of the world's population. Estimates as to how many infected people died vary greatly, but the flu is regardless considered to be one of the deadliest pandemics in history. An early estimate from 1927 put global mortality at 21.6 million. An estimate from 1991 states that the virus killed between 25 and 39 million people. A 2005 estimate put the death toll at 50 million (about 3% of the global population), and possibly as high as 100 million (more than 5%). However, a 2018 reassessment in the American Journal of Epidemiology estimated the total to be about 17 million, though this has been contested. With a world population of 1.8 to 1.9 billion, these estimates correspond to between 1 and 6 percent of the population.
A 2009 study in Influenza and Other Respiratory Viruses based on data from fourteen European countries estimated a total of 2.64 million excess deaths in Europe attributable to the Spanish flu during the major 1918–1919 phase of the pandemic, in line with the three prior studies from 1991, 2002, and 2006 that calculated a European death toll of between 2 million and 2.3 million. This represents a mortality rate of about 1.1% of the European population (c. 250 million in 1918), considerably higher than the mortality rate in the US, which the authors hypothesize is likely due to the severe effects of the war in Europe. The excess mortality rate in the U.K. has been estimated at 0.28%-0.4%, far below this European average.
Some 12–17 million people died in India, about 5% of the population. The death toll in India's British-ruled districts was 13.88 million. Another estimate gives at least 12 million dead. The decade between 1911 and 1921 was the only census period in which India's population fell, mostly due to devastation of the Spanish flu pandemic. While India is generally described as the country most severely affected by the Spanish flu, at least one study argues that other factors may partially account for the very high excess mortality rates observed in 1918, citing unusually high 1917 mortality and wide regional variation (ranging from 0.47% to 6.66%). A 2006 study in The Lancet also noted that Indian provinces had excess mortality rates ranging from 2.1% to 7.8%, stating: "Commentators at the time attributed this huge variation to differences in nutritional status and diurnal fluctuations in temperature."
In Finland, 20,000 died out of 210,000 infected. In Sweden, 34,000 died.
In Japan, 23 million people were affected, with at least 390,000 reported deaths. In the Dutch East Indies (now Indonesia), 1.5 million were assumed to have died among 30 million inhabitants. In Tahiti, 13% of the population died during one month. Similarly, in Western Samoa 22% of the population of 38,000 died within two months.
In Istanbul, capital of the Ottoman Empire, 6,403 to 10,000 died, giving the city a mortality rate of at least 0,56%.
In New Zealand, the flu killed an estimated 6,400 Pakeha and 2,500 indigenous Maori in six weeks, with Māori dying at eight times the rate of Pakeha.
In the US, about 28% of the population of 105 million became infected, and 500,000 to 850,000 died (0.48 to 0.81 percent of the population). Native American tribes were particularly hard hit. In the Four Corners area, there were 3,293 registered deaths among Native Americans. Entire Inuit and Alaskan Native village communities died in Alaska. In Canada, 50,000 died.
In Brazil, 300,000 died, including president Rodrigues Alves.
In Britain, as many as 250,000 died; in France, more than 400,000.
In Ghana, the influenza epidemic killed at least 100,000 people. Tafari Makonnen (the future Haile Selassie, Emperor of Ethiopia) was one of the first Ethiopians who contracted influenza but survived. Many of his subjects did not; estimates for fatalities in the capital city, Addis Ababa, range from 5,000 to 10,000, or higher.
The death toll in Russia has been estimated at 450,000, though the epidemiologists who suggested this number called it a "shot in the dark". If it is correct, Russia lost roughly 0.4% of its population, meaning it suffered the lowest influenza-related mortality in Europe. Another study considers this number unlikely, given that the country was in the grip of a civil war, and the infrastructure of daily life had broken down; the study suggests that Russia's death toll was closer to 2%, or 2.7 million people.
Devastated communities
Even in areas where mortality was low, so many adults were incapacitated that much of everyday life was hampered. Some communities closed all stores or required customers to leave orders outside. There were reports that healthcare workers could not tend the sick nor the gravediggers bury the dead because they too were ill. Mass graves were dug by steam shovel and bodies buried without coffins in many places.
Bristol Bay, a region of Alaska populated by indigenous people, suffered a death rate of 40 percent of the total population, with some villages entirely disappearing.
Several Pacific island territories were hit particularly hard. The pandemic reached them from New Zealand, which was too slow to implement measures to prevent ships, such as Talune, carrying the flu from leaving its ports. From New Zealand, the flu reached Tonga (killing 8% of the population), Nauru (16%), and Fiji (5%, 9,000 people). Worst affected was Western Samoa, formerly German Samoa, which had been occupied by New Zealand in 1914. 90% of the population was infected; 30% of adult men, 22% of adult women, and 10% of children died. By contrast, Governor John Martin Poyer prevented the flu from reaching neighboring American Samoa by imposing a blockade. The disease spread fastest through the higher social classes among the indigenous peoples, because of the custom of gathering oral tradition from chiefs on their deathbeds; many community elders were infected through this process.
In Iran, the mortality was very high: according to an estimate, between 902,400 and 2,431,000, or 8% to 22% of the total population died. The country was going through the Persian famine of 1917–1919 concurrently.
In Ireland, during the worst 12 months, the Spanish flu accounted for one-third of all deaths.
In South Africa it is estimated that about 300,000 people amounting to 6% of the population died within six weeks. Government actions in the early stages of the virus' arrival in the country in September 1918 are believed to have unintentionally accelerated its spread throughout the country. Almost a quarter of the working population of Kimberley, consisting of workers in the diamond mines, died. In British Somaliland, one official estimated that 7% of the native population died. This huge death toll resulted from an extremely high infection rate of up to 50% and the extreme severity of the symptoms, suspected to be caused by cytokine storms.
Less-affected areas
In the Pacific, American Samoa and the French colony of New Caledonia also succeeded in preventing even a single death from influenza through effective quarantines. Australia also managed to avoid the first two waves with a quarantine. Iceland protected a third of its population from exposure by blocking the main road of the island. By the end of the pandemic, the isolated island of Marajó, in Brazil's Amazon River Delta had not reported an outbreak. Saint Helena also reported no deaths.

Estimates for the death toll in China have varied widely, a range which reflects the lack of centralized collection of health data at the time due to the Warlord period. China may have experienced a relatively mild flu season in 1918 compared to other areas of the world. However, some reports from its interior suggest that mortality rates from influenza were perhaps higher in at least a few locations in China in 1918. At the very least, there is little evidence that China as a whole was seriously affected by the flu compared to other countries in the world.
The first estimate of the Chinese death toll was made in 1991 by Patterson and Pyle, which estimated a toll of between 5 and 9 million. However, this 1991 study was criticized by later studies due to flawed methodology, and newer studies have published estimates of a far lower mortality rate in China. For instance, Iijima in 1998 estimates the death toll in China to be between 1 and 1.28 million based on data available from Chinese port cities. The lower estimates of the Chinese death toll are based on the low mortality rates that were found in Chinese port cities (for example, Hong Kong) and on the assumption that poor communications prevented the flu from penetrating the interior of China. However, some contemporary newspaper and post office reports, as well as reports from missionary doctors, suggest that the flu did penetrate the Chinese interior and that influenza was severe in at least some locations in the countryside of China.
Although medical records from China's interior are lacking, extensive medical data was recorded in Chinese port cities, such as then British-controlled Hong Kong, Canton, Peking, Harbin and Shanghai. These data were collected by the Chinese Maritime Customs Service, which was largely staffed by non-Chinese foreigners, such as the British, French, and other European colonial officials in China. As a whole, accurate data from China's port cities show astonishingly low mortality rates compared to other cities in Asia. For example, the British authorities at Hong Kong and Canton reported a mortality rate from influenza at a rate of 0.25% and 0.32%, much lower than the reported mortality rate of other cities in Asia, such as Calcutta or Bombay, where influenza was much more devastating. Similarly, in the city of Shanghai – which had a population of over 2 million in 1918 – there were only 266 recorded deaths from influenza among the Chinese population in 1918. If extrapolated from the extensive data recorded from Chinese cities, the suggested mortality rate from influenza in China as a whole in 1918 was likely lower than 1% – much lower than the world average (which was around 3–5%). In contrast, Japan and Taiwan had reported a mortality rate from influenza around 0.45% and 0.69% respectively, higher than the mortality rate collected from data in Chinese port cities, such as Hong Kong (0.25%), Canton (0.32%), and Shanghai.



