Lymphangioleiomyomatosis
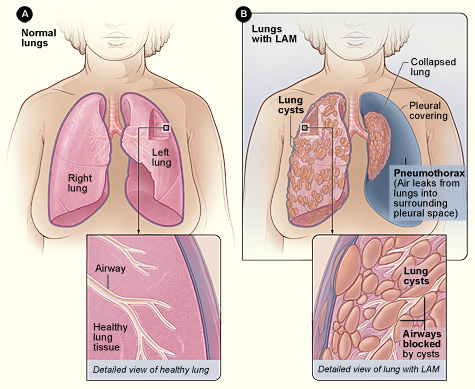
Lymphangioleiomyomatosis (LAM) is a multiple cystic lung disease characterized by progressive cystic destruction of the lung and lymphatic abnormalities, frequently associated with renal angiomyolipomas (AMLs). LAM occurs either sporadically or as a manifestation of tuberous sclerosis complex (TSC).
Epidemiology
Sporadic LAM affects around 1/500,000-1/125,000 adult women in Europe. TSC is present in 1 in 6,000 births. Pulmonary LAM is present in up to 30-40% of adult TSC cases. LAM affects almost exclusively females.
Clinical description
Defining manifestations of the disease are respiratory and include progressive dyspnea, pneumothorax and chylothorax. LAM may lead to chronic respiratory failure. A common extra-pulmonary manifestation is a high incidence of AMLs, mostly localized to the kidneys and usually asymptomatic (hemorrhage is rare). Chylous ascites, abdominal and thoracic lymphadenopathy and lymphangioleiomyomas can be observed. Symptoms may worsen during pregnancy. In TSC-LAM the symptoms of TSC are present.
Etiology
Sporadic LAM is due to somatic mutations in the tuberous sclerosis genes TSC1 and TSC2, that encode the major signaling proteins hamartin and tuberin. Mutations result in excessive proliferation of LAM cells. In TSC, germline mutations are found.
Diagnostic methods
Diagnosis of LAM can be definite, probable or possible. For a definite LAM diagnosis, a high resolution computed tomography (HRCT) scan shows more than 10 lung cysts with diffuse distribution together with a lung biopsy showing cysts and abnormal immature smooth muscle-like cells (LAM cells) or a HRCT scan shows typical lung cysts and one of the following: AMLs in the kidney, thoracic or abdominal chylous effusion, lymphangioleiomyoma and definite or probable TSC. Lung cysts are present together with a clinical history of pneumothorax or with an HRCT showing AMLs or thoracic or abdominal chylous effusion in probable LAM. Elevation of serum level of vascular endothelial growth factor D (VEGF-D) greater than 800 mg/L is LAM specific and confirms diagnosis. Possible LAM is diagnosed when only characteristic lung cysts are present. If TSC is also present then TSC-LAM is diagnosed.
Differential diagnosis
The two main differential diagnoses are adult pulmonary Langerhans cell histiocytosis and emphysema. Less frequent differential diagnoses include hypersensitivity pneumonitis, light chain-deposition disease, Birt-Hogg-Dubé syndrome and Sjögren syndrome.
Genetic counseling
Sporadic LAM is not inherited. In TSC-LAM genetic counseling is difficult due to the great variability in clinical presentation.
Management and treatment
Management of air flow obstruction is essential and 1/4 of patients respond to inhaled bronchodilators. Chemical pleurodesis may be performed at first pneumothorax to prevent increased risk of recurrent pneumothorax. Surgical pleurodesis is often necessary for a recurrent pneumo or chylothorax. Single/bilateral lung transplantation is performed when other options have proven unsuccessful. The mTOR inhibitor sirolimus may be used in expert centres to stabilize or improve pulmonary function in severe cases. Asymptomatic AMLs <4cm in diameter do not usually need to be treated but should be monitored. AMLs >4 cm, with microaneurysms >0.5 cm or bleeding should be treated by selective arterial embolisation, sirolimus therapy, or nephron sparing surgery. LAM patients who develop respiratory symptoms should have periodic pulmonary function testing. Estrogen therapy should be avoided.
Prognosis
Disease progression rate and severity is highly variable. The main predictor of prognosis is the rate of decline in pulmonary function with sporadic LAM generally more severe than TSC-LAM.