Glioblastoma
Glioblastomas are malignant astrocytic tumors (grade IV according to the WHO classification).
Epidemiology
Glioblastomas represent the most frequent brain tumors in adults, with an annual incidence of around 1/33,330. Prevalence is estimated at 1/100,000.
Clinical description
They may occur at any age, but 70% of cases are seen in patients between 45 and 70 years of age. The tumors are usually located in the brain hemispheres, but can be found anywhere in the central nervous system. The disease often progresses rapidly (over 2 to 3 months), except when the glioblastoma develops within a pre-existing low grade astrocytoma (secondary glioblastoma). Neurological signs are nonspecific as they result from intracranial hypertension and include headaches and vomiting, often associated with behavioral changes or focal neurological deficits. Histological variants (gliosarcoma and giant cell glioblastoma) have been described for which the treatment protocols and prognosis are similar to those of glioblastoma.
Etiology
The cause of the disease is unknown, except when it occurs after therapeutic irradiation of the brain for another disease. The genetic abnormalities detected (amplification of the EGFR gene (7p12), mutations in the TP53 gene (17p13.1), loss of chromosome 10) vary depending on the nature of the tumor: primary glioblastoma (de novo) or a secondary glioblastoma (developing from a benign astrocytic tumor).
Diagnostic methods
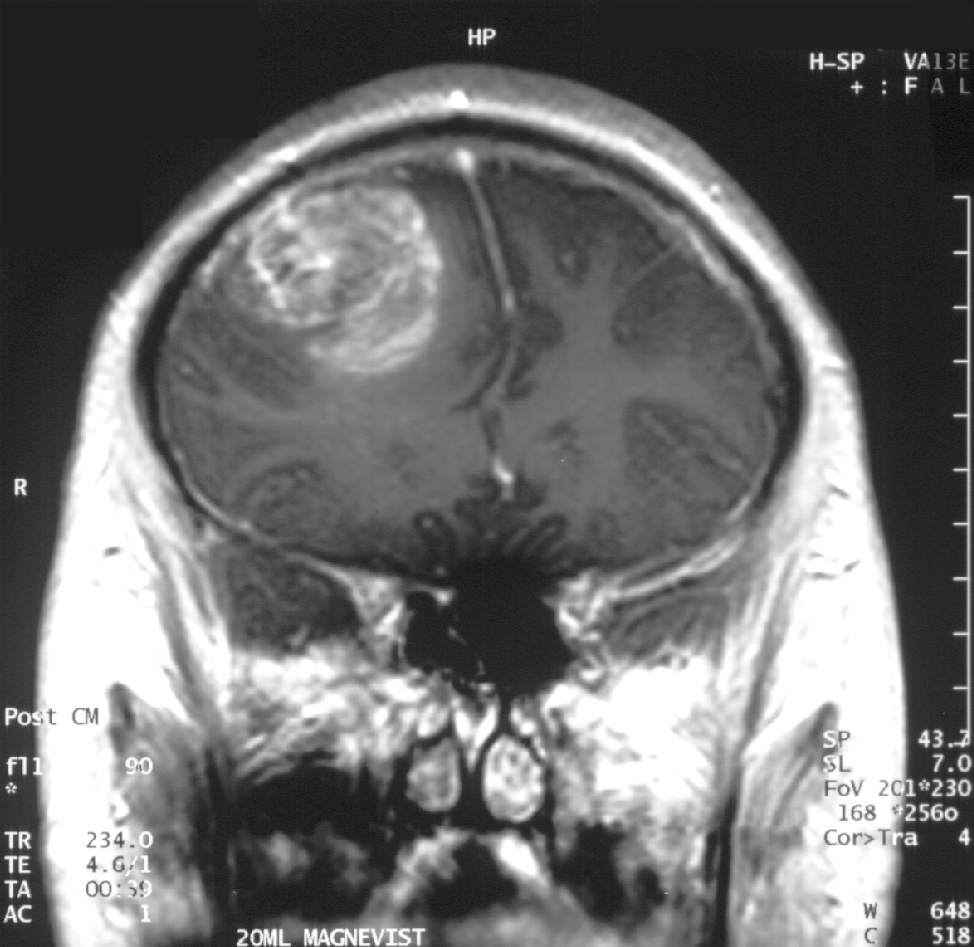
Radiologic studies, computerized tomography (CT) and magnetic resonance imaging (MRI) demonstrate characteristic features such as an infiltrating tumor associated with heterogeneous contrast enhancement and areas of necrosis.
Differential diagnosis
The differential diagnosis should include infectious and parasitic diseases with central nervous system involvement. Familial forms of glioblastoma are very rare but the tumor may occur as part of a syndrome such as Turcot syndrome, neurofibromatosis type 1 or Li-Fraumeni syndrome (see these terms).
Management and treatment
The first-line treatment is usually surgery, either to confirm the diagnosis with a biopsy or to remove as much of the tumor as possible. Complete resection is rarely feasible, since tumor cells usually infiltrate the surrounding brain. Treatment is then completed with radiotherapy targeted at the tumor bed, combined with chemotherapy (nitrosoureas and temozolomide). In terms of survival, the benefits from adjuvant treatments after surgery are significant, although they remain modest. In case of relapse, second-line chemotherapy or reoperation may be performed. Due to the relative rarity of this tumor, management of glioblastoma patients should be carried out by multidisciplinary teams with expertise in neuro-oncology within prospective studies aiming to improve patient survival and quality of life.
Prognosis
Prognosis is poor, especially in the absence of gross total resection, in older patients and in case of severe neurological deficits.