Chronic Granulomatous Disease
Summary
Clinical characteristics.
Chronic granulomatous disease (CGD) is a primary immunodeficiency disorder of phagocytes (neutrophils, monocytes, macrophages, and eosinophils) resulting from impaired killing of bacteria and fungi. CGD is characterized by severe recurrent bacterial and fungal infections and dysregulated inflammatory response resulting in granuloma formation and other inflammatory disorders such as colitis. Infections typically involve the lung (pneumonia), lymph nodes (lymphadenitis), liver (abscess), bone (osteomyelitis), and skin (abscesses or cellulitis); granulomas typically involve the genitourinary system (bladder) and gastrointestinal tract (often the pylorus initially, and later the esophagus, jejunum, ileum, cecum, rectum, and perirectal area). Some males with X-linked CGD have McLeod neuroacanthocytosis syndrome as the result of a contiguous gene deletion. CGD may present anytime from infancy to late adulthood; however, the vast majority of affected individuals are diagnosed before age five years. Use of antimicrobial prophylaxis and therapy has greatly improved overall survival.
Diagnosis/testing.
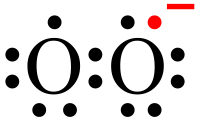
CGD is diagnosed by tests that measure neutrophil superoxide production via the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex: the dihydrorhodamine (DHR) test has largely replaced the nitroblue tetrazolium (NBT) test, the oldest and most recognized diagnostic test for CGD. CGD is caused by pathogenic variants in one of five genes that encode the subunits of phagocyte NADPH oxidase: biallelic pathogenic variants in CYBA, NCF1, NCF2, and NCF4 cause autosomal recessive CGD (AR-CGD); mutation of CYBB causes X-linked CGD.
Management.
Treatment of manifestations: A definitive microbiologic diagnosis is essential to proper treatment of infections. Newer azole drugs (voriconazole, posaconazole, isovuconazole) have expanded therapeutic options for fungal infections. Long courses of antimicrobials are often needed for adequate treatment. Abscesses may require percutaneous drainage or excisional surgery. Simultaneous administration of antimicrobials and corticosteroids can help resolve the associated heightened inflammatory response, including colitis.
Prevention of primary manifestations: Allogeneic hematopoietic stem cell transplantation (HSCT) is the only known cure for CGD; however, indications for and timing of HSCT are yet to be resolved. Antibacterial and antifungal prophylaxis is the cornerstone of prevention; immunomodulatory therapy with interferon gamma (IFN-gamma) is part of the prophylactic regimen in many centers.
Surveillance: Regular follow-up visits can aid in early detection and treatment of asymptomatic or minimally symptomatic infections and noninfectious complications such as colitis, pulmonary granulomas, and pulmonary fibrosis.
Agents/circumstances to avoid: (1) Decayed organic matter (e.g., mulching, gardening, leaf raking, house demolition) as inhalation of fungal spores can result in fulminant pneumonitis; (2) bacille Calmette-Guérin (BCG) vaccination; (3) persons with CGD and McLeod neuroacanthocytosis syndrome: blood transfusions that are Kell antigen positive.
Evaluation of relatives at risk: Early diagnosis of relatives at risk allows for prompt initiation of antimicrobial prophylaxis and other treatment.
Pregnancy management: The major concern during the pregnancy of a woman known to have CGD is use of prophylactic antimicrobials: trimethoprim, a folic acid antagonist, is discontinued during pregnancy because of the high risk for birth defects. Although sulfamethoxazole is not known to increase the risk of birth defects in humans, it is typically administered in conjunction with trimethoprim. Data regarding teratogenicity of itraconazole are limited.
Genetic counseling.
CGD associated with a pathogenic variant in CYBB is inherited in an X-linked manner. CGD associated with biallelic pathogenic variants in CYBA, NCF1, NCF2, or NCF4 is inherited in an autosomal recessive manner.
- X-linked CGD. If the mother of an affected male is heterozygous for a CYBB pathogenic variant, the chance of transmitting it in each pregnancy is 50%. Males who inherit the pathogenic variant will be affected; females who inherit the pathogenic variant will be heterozygous and will usually not be affected with typical CGD but may have other manifestations including discoid lupus erythematosus and aphthous ulcers.
- AR-CGD. At conception, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier.
Molecular genetic carrier testing and prenatal testing for pregnancies at increased risk is possible if the pathogenic variant(s) in a family are known. (Other carrier and prenatal testing options may be available if the pathogenic variant[s] in the family are not known.)
Diagnosis
Suggestive Findings
Chronic granulomatous disease (CGD) should be suspected in individuals (usually children) with the following clinical features and laboratory testing:
Clinical features
- Growth retardation in childhood
- Infections of lung (pneumonia), lymph nodes (lymphadenitis), liver (abscess), bone (osteomyelitis), and skin (abscesses or cellulitis), especially spontaneously occurring severe or recurrent bacterial infections. Microbiologic confirmation of the cause of infection helps confirm the likelihood of CGD, since the spectrum of infection in CGD is distinct and narrow (see Table 2).
- Granuloma formation, especially genitourinary (bladder) and gastrointestinal (often pyloric initially, and later esophageal, jejunal, ileal, cecal, rectal, and perirectal)
- Colitis, manifesting as frequent stooling and fistulae or fissures. This may be the sole finding in some individuals.
- Abnormal wound healing caused by excessive granulation, which may cause the wound to dehisce and gape, leading to healing by secondary intention
Laboratory testing
Clinical tests that rely on direct measurement of neutrophil superoxide production via the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex to establish the diagnosis of CGD include the following:
Dihydrorhodamine (DHR) test uses flow cytometry to measure the oxidation of dihydrorhodamine 123 to rhodamine 123 in phorbol myrisate acetate (PMA)-stimulated neutrophils, a marker for cellular NADPH oxidase activity [Vowells et al 1996]. In this test the generation of hydrogen peroxide oxidizes the dye, leading to the emission of fluorescence. Mean fluorescence intensity of the activated cells correlates directly with (and thus serves as a reliable surrogate for) superoxide production [Kuhns et al 2010].
The DHR test can distinguish the following forms of CGD:
- Complete forms (i.e., those with absent to greatly diminished production of superoxide) commonly observed in males with X-linked CGD
- Hypomorphic (variant) forms of CGD characterized by reduced protein expression/function and residual superoxide production (observed in autosomal recessive CGD and protein-positive X-linked CGD)
- Mosaic forms (i.e., those with two discrete populations of phagocytes: some oxidase-positive and some oxidase-negative) commonly observed in female carriers of X-linked CGDNote: Although the pattern of oxidase-positive and oxidase-negative phagocytes can suggest X-linked inheritance of CGD or autosomal recessive inheritance of CGD, the results are not definitive in establishing the mode of inheritance.
Although the DHR is superior to other tests for CGD, it is not always clinically available to ordering clinicians, and the nitroblue tetrazolium (NBT) test is ordered in its place.
Nitroblue tetrazolium (NBT) test, the oldest and most recognized diagnostic test for CGD, relies on light microscopy to provide a mostly qualitative determination of phagocyte NADPH oxidase activity. When stimulated in vitro, normal phagocytes produce superoxide that reduces yellow NBT to blue/black formazan, forming a precipitate in cells [Baehner & Nathan 1967]. The NBT test is typically performed on a microscope slide, which is read manually to distinguish reducing (blue-black) from non-reducing (unstained) cells:
- Neutrophils in unaffected non-carriers. More than 95% of cells produce superoxide that reduces NBT to formazan.
- Neutrophils in individuals with CGD. Production of superoxide is absent or greatly diminished.
- Female carriers of X-linked CGD (who have two populations of leukocytes). Superoxide is typically produced in 20%-80% of cells [Elloumi & Holland 2014] (range: 0.001%-97%).Note: Because the NBT test is semi-quantitative and evaluates only a limited number of cells, it may be falsely interpreted as normal in: (1) female carriers of X-linked CGD, especially those with skewed (non-random) X-chromosome inactivation (see Carriers of X-Linked CGD); and (2) persons with hypomorphic (variant) forms of CGD characterized by partial protein expression/function and residual superoxide production (observed in autosomal recessive CGD and protein-positive X-linked CGD).
Click here for information about research testing.
Establishing the Diagnosis
The diagnosis of CGD is established in a proband with identification of pathogenic variant(s) in one of five genes that encode the subunits of phagocyte NADPH oxidase (see Table 1).
- CYBA, NCF1, NCF2, and NCF4 are the genes in which biallelic pathogenic variants cause autosomal recessive chronic granulomatous disease (AR-CGD).
- CYBB is the gene in which a hemizygous pathogenic variant causes X-linked chronic granulomatous disease (X-linked CGD).
Molecular testing approaches can include serial single-gene testing, use of a multigene panel, and more comprehensive genomic testing.
- Serial single-gene testing. Sequence analysis of the gene of interest is performed first, followed by gene-targeted deletion/duplication analysis if only one or no pathogenic variant is found. Of note:
- Early-onset, more severe infections and male gender suggest X-linked CGD, and CYBB testing may be considered first.
- Later-onset, milder course, female gender, and consanguinity suggest autosomal recessive CGD.
- The c.75_76delGT deletion is a common pathogenic variant in NCF1 (see Table 1); however, NCF1-related CDG is not clinically distinguishable from other autosomal recessive forms.
- A multigene panel that includes CYBA, NCF1, NCF2, NCF4, CYBB, and other genes of interest (see Differential Diagnosis) may also be considered. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview; thus, clinicians need to determine which multigene panel is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
- More comprehensive genomic testing (when available) including exome sequencing, genome sequencing, and mitochondrial sequencing may be considered if serial single-gene testing (and/or use of a multigene panel) fails to confirm a diagnosis in an individual with features of CGD.For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Special Consideration in a Male with Suspected CGD and Other Medical Issues
Large deletions in Xp21.1 have been reported in some with X-CGD. Other genes that lie in close proximity to CYBB at Xp21.1 include the following [Peng et al 2007] (see Note):
- XK, encoding the Kx blood group (telomeric) associated with McLeod neuroacanthocytosis syndrome (deletion of XK). This is a multisystem disorder with central nervous system (CNS), neuromuscular, and hematologic manifestations in males. CNS manifestations are a neurodegenerative basal ganglia disease including (1) movement disorder, (2) cognitive impairment, and (3) psychiatric symptoms. Neuromuscular manifestations include a (mostly subclinical) sensorimotor axonopathy and clinically relevant muscle weakness or atrophy. The hematologic manifestations are red blood cell acanthocytosis, compensated hemolysis, and the McLeod blood group phenotype resulting from absent expression of the Kx erythrocyte antigen and reduced expression of the Kell blood group antigens. The Kell blood group system can cause strong reactions to transfusions of incompatible blood and severe anemia in newborns of Kell-negative mothers. Heterozygous females have mosaicism for the Kell system blood group antigens and RBC acanthocytosis but lack CNS and neuromuscular manifestations.
- RPGR, encoding retinitis pigmentosa GTPase regulator (telomeric) associated with RPGR-related retinitis pigmentosa
- DMD, encoding the protein dystrophin (telomeric) associated with Duchenne muscular dystrophy
- OTC, encoding ornithine transcarbamylase (centromeric) associated with ornithine transcarbamylase deficiency (OTC) leading to urea cycle defects
- Note: Concurrent deletion of XK with CYBB is the most common; deletion of all five genes is exceedingly rare.
Therefore:
- Patients with suspected X-CGD and clinical manifestations of McLeod syndrome, retinitis pigmentosa, Duchenne muscular dystrophy, and/or ornithine transcarbamylase deficiency should have a chromosome microarray analysis (CMA).
- If a large deletion is found within CYBB, a CMA may be indicated.
Table 1.
Molecular Genetic Testing Used in Chronic Granulomatous Disease
| Gene 1 / Protein | Mode of Inheritance | Proportion of CGD Attributed to Pathogenic Variants in This Gene 2 | Proportion of Pathogenic Variants 3 Detected by Test Method | |
|---|---|---|---|---|
| Sequence analysis 4 | Gene-targeted deletion/duplication analysis 5 | |||
| CYBA / p22phox | AR | 6% 6 | ~85% | ~15% |
| NCF1 / p47phox | AR | 20% 6 | ~99%7 | ~1% 8 |
| NCF2 / p67pho | AR | 6% 6 | ~85% | ~15% 9 |
| NCF4 / p40phox | AR | One individual 10 | 2/2 alleles | |
| CYBB / gp91phox | XL | ~67% 11 | ~85% 12, 13 | ~15% 13, 14 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
These rates apply to North America and certain western European populations.
- 3.
See Molecular Genetics for information on allelic variants detected in this gene.
- 4.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 5.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 6.
Roos et al [2010a]
- 7.
By far the most common pathogenic variant in NCF1 is GT deletion c.75_76delGT [Kuhns et al 2010, Roos et al 2010a]. Molecular testing for c.75_76delGT can be complicated by nearby pseudogenes (see Molecular Genetics).
- 8.
Several large, intragene deletions in NCF1 have been reported [Roos et al 2010a, Roos et al 2010b, Raptaki et al 2013].
- 9.
Leusen et al [1996], Gentsch et al [2010], Roos et al [2010a], Teimourian et al [2010], Badalzadeh et al [2012]
- 10.
Inactivating pathogenic variants in both NCF4 alleles were reported in one individual [Matute et al 2009]
- 11.
Roos et al [2010b]
- 12.
Roos et al [1996], Roos et al [2010b]
- 13.
Lack of amplification by PCR prior to sequence analysis can suggest a putative (multi)exon or whole-gene deletion on the X chromosome in affected males; confirmation requires additional testing by gene-targeted deletion/duplication analysis.
- 14.
If a contiguous gene deletion involving multiple genes at Xp21.1 is suspected based on clinical findings, a chromosome microarray analysis (CMA) to detect a microdeletion may be warranted.
Clinical Characteristics
Clinical Description
Chronic granulomatous disease (CGD) is characterized by severe recurrent bacterial and fungal infections and dysregulated inflammatory response resulting in granuloma formation and other inflammatory disorders such as colitis.
CGD may present anytime from infancy to late adulthood; however, the vast majority of affected individuals are diagnosed before age five years. The median age of diagnosis was 2.5 to three years in several series [Jones et al 2008, Martire et al 2008]. More recently, increased numbers of affected individuals have been diagnosed in adolescence or adulthood. This delay in diagnosis may be attributed to the following:
- Effective treatment of CGD-related infections with antimicrobials not available in the past
- Recognition of milder cases of autosomal recessive (AR) CGD that may have gone undiagnosed without currently available tests and/or awareness of milder disease manifestations
- Overall improvement in food handling and sanitation
Infections and granulomatous lesions are usually the first manifestations of CGD, with the most frequent sites being the lung, lymph nodes, liver, and skin. The types of infection seen most often include pneumonia, abscess, adenitis, osteomyelitis, and cellulitis. Other pulmonary complications include empyema and hilar adenopathy. The most common sites for abscesses are the perianal and perirectal areas as well as the liver.
Although the frequency of infections in persons with CGD has decreased with the routine administration of antibacterial and antifungal prophylaxis, infections still occur at a frequency of 0.3/year.
In North America, the majority of infections in CGD are caused by Staphylococcus aureus, Burkholderia cepacia complex, Serratia marcescens, Nocardia species, and Aspergillus species [Marciano et al 2015] (Table 2). In other parts of the world, important causes of infection are Salmonella, bacille Calmette-Guérin (BCG), and tuberculosis [Winkelstein et al 2000, van den Berg et al 2009].
Table 2.
Infections in CGD: Common Pathogens and Sites of Involvement
| Pathogen | Presentation | |
|---|---|---|
| Bacterial infections | Staphylococcus aureus | Soft tissue infections Lymphadenitis Liver abscess Osteomyelitis Pneumonia Sepsis |
Burkholderia species 1
| Pneumonia Sepsis | |
| Serratia marcescens 3 | More common:
| |
Nocardia species 4, 5
| Pneumonia Osteomyelitis Brain abscess | |
| Necrotizing lymphadenitis Sepsis Meningitis | |
| Sepsis | |
| Sepsis | |
| Fungal infections 9 | Aspergillus species
| Pneumonia Osteomyelitis Brain abscess Lymphadenitis |
Paecilomyces species
| Pneumonia Soft tissue infections Osteomyelitis | |
Other molds
| Pneumonia Soft tissue infection | |
| Yeast infections | Candida
| Sepsis Soft tissue infection Liver abscess |
Trichosporon
| Pneumonia Soft tissue infection | |
- 1.
Greenberg et al [2009]
- 2.
B cepacia is also a cause of pneumonia in cystic fibrosis.
- 3.
Galluzzo et al [2008], Friend et al [2009]
- 4.
Dorman et al [2002]
- 5.
Outside of CGD Nocardia infections occur predominantly in the setting of high-dose corticosteroids.
- 6.
Greenberg et al [2006]
- 7.
Sirinavin et al [2005]
- 8.
Mailman & Schmidt [2005]
- 9.
Beauté et al [2011], Blumental et al [2011]
- 10.
De Ravin et al [2011]
- 11.
De Ravin et al [2014], Ramesh et al [2014], Shigemura et al [2015]
Bacterial Infections
Widespread prophylaxis has limited staphylococcal infections primarily to the skin, lymph nodes, liver, and (rarely) lung [Marciano et al 2015].
Burkholderia cepacia complex infection is common in patients with CGD and can occasionally cause sepsis.
Outside of CGD, Nocardia infections occur predominantly in the setting of high-dose corticosteroids.
Mycobacterial diseases in CGD are mostly limited to regional and disseminated BCG infections and tuberculosis. Persons with CGD are less susceptible to nontuberculous infections than persons with defects in T cell or interferon gamma/IL-12 pathways: in persons with CGD, BCG infection may cause severe localized disease such as draining skin lesions at sites of BCG vaccination [Lee et al 2008], whereas in persons with severe combined immunodeficiency or defects in the IFN-gamma receptor pathway, BCG infection typically causes disseminated disease.
Uncommon bacterial infections that are virtually pathognomonic for CGD include:
- Granulibacter bethesdensis, which causes necrotizing lymphadenitis, sepsis, and meningitis [Greenberg et al 2006];
- Chromobacterium violaceum, which is found in brackish waters such as the Gulf of Mexico and causes sepsis [Sirinavin et al 2005];
- Francisella philomiragia, which is also found in brackish waters such as the Chesapeake Bay and is a cause of sepsis [Mailman & Schmidt 2005].
Bacteremia is relatively uncommon except with certain gram-negative organisms.
Fungal Infections
Invasive fungal infections, which have the highest prevalence in CGD among all primary immunodeficiencies, remain the leading cause of mortality in CGD. They occur most commonly in the first two decades of life and can be a first presentation of disease [Marciano et al 2015]; about 30% of individuals with CGD will develop fungal infections [Beauté et al 2011, Marciano et al 2015].
Fungal infections are typically acquired through inhalation of spores or hyphae resulting in pneumonia that can spread locally to the ribs and spine or metastatically to the brain. Presentation may be insidious with symptoms that are absent or manifest as failure to thrive and malaise. Other common presenting signs and symptoms include cough, fever, and chest pain.
Aspergillus species are the most common cause of invasive fungal infections, typically in the lung.
- Aspergillus fumigatus is the most common of the Aspergillus species to cause infection in CGD. Although angioinvasion is common in neutropenic settings, it does not occur in CGD.
- Aspergillus nidulans infection is almost exclusive to CGD and causes more severe and refractory disease with local and distant spread [Segal et al 1998, Beauté et al 2011].
Paecilomyces lilacinus and Paecilomyces variotti cause pneumonia and osteomyelitis in CGD almost exclusively.
Mucormycosis has been reported in CGD but appears to occur only in the setting of significant immunosuppression [Vinh et al 2009].
The overall frequency and mortality of invasive fungal infections have been significantly reduced with the use of itraconazole as antifungal prophylaxis and the use of other azoles (voriconazole and posaconazole) as therapy. However, when they occur, fungal infections develop at an older age and may require longer duration of therapy. Fungal infections cause more mortality than other infections in CGD [Marciano et al 2015]. An increased frequency of infection with Aspergillus nidulans and other opportunistic fungi may be associated with itraconazole prophylaxis [Blumental et al 2011].
Yeast infections are not nearly as common as bacterial and fungal infections in persons with CGD; mucocutaneous candidiasis is not encountered.
Note: The endemic dimorphic mold infections histoplasmosis, blastomycosis, and coccidioidomycosis do not occur in CGD [Holland 2010].
Inflammatory and Other Manifestations
Formation of granulomata and dysregulated inflammation in CGD contribute to morbidity and can cause multiple symptoms. The genitourinary and gastrointestinal tracts are most commonly affected.
- Genitourinary manifestations include bladder granulomata that are associated with ureteral obstruction and urinary tract infections. Other manifestations include pseudotumors of the bladder and eosinophilic cystitis.
- Gastrointestinal manifestations
- Pyloric edema leads to functional gastric outlet obstruction and can be an initial presentation of CGD.
- Esophageal, jejunal, ileal, cecal, rectal, and perirectal granulomata similar to those in Crohn disease have also been described. Symptomatic inflammatory bowel disease affects up to 50% of affected individuals and can be the presenting finding [Marciano et al 2004].
- Other gastrointestinal symptoms indicative of CGD colitis include abdominal pain, diarrhea, strictures, and fistulae. Significant colitis leading to bowel obstruction, fistulae, and strictures can be an important cause of growth retardation [Marciano et al 2004].
Liver involvement is a significant cause of morbidity in CGD, with abscesses occurring in up to 35% of affected individuals. Liver abscesses have been difficult to cure without surgery and carry a significant risk for recurrence, but not relapse [Hussain et al 2007].
Other common liver abnormalities include liver enzyme elevation, persistent elevations in alkaline phosphatase, and drug-induced hepatitis.
High rates of portal venopathy are associated with splenomegaly and nodular regenerative hyperplasia. Portal hypertension and thrombocytopenia are associated with intrahepatic disease and important risk factors for mortality [Hussain et al 2007, Feld et al 2008].
Hyperinflammation is seen, especially in response to infectious agents. The exact etiology of dysregulated inflammation in CGD is unclear. Heightened inflammatory response has been described in chronic colitis [Marciano et al 2004], granulomatous cystitis [Kontras et al 1971], pulmonary infections with Nocardia [Freeman et al 2011], and staphylococcal liver abscesses [Yamazaki-Nakashimada et al 2006, Leiding et al 2012].
Fungi elicit an exuberant inflammatory response regardless of whether the fungi are alive or dead [Morgenstern et al 1997] as in "mulch pneumonitis," a syndrome caused by inhalation of aerosolized decayed organic matter (e.g., hay, dead leaves) [Siddiqui et al 2007]. Acute fulminant pneumonitis (similar to that seen in hypersensitivity pneumonitis) ensues.
Prolonged and dysregulated inflammation in CGD can overlap clinically with the syndrome of hemophagocytic lymphohistiocytosis (HLH). HLH is caused by an ineffective and unrestrained inflammatory response by T lymphocytes, NK cells, and macrophages leading to fever, hepatosplenomegaly, cytopenias, and hemophagocytosis in the bone marrow and other tissues. Persons with CGD can develop prolonged fever and most of the clinical features of HLH.
Growth retardation is common in CGD and failure to thrive can be a common presenting finding [Marciano et al 2004]. Growth failure can be compounded by colitis. Growth may improve in late adolescence and many affected individuals may attain appropriate adult height and weight, albeit on the lower end of the spectrum.
Chronic respiratory disease can result from recurrent infection. Bronchiectasis, obliterative bronchiolitis, and chronic fibrosis may occur but are not as common as in some other primary immunodeficiencies.
Ophthalmic manifestations include chorioretinal lesions and granulomata with pigment clumping that are usually asymptomatic but often associated with recovery of bacterial DNA from retinal tissue samples [Wang et al 2013]. Inflammatory eye disease including keratitis and uveitis can occur as well.
Oral manifestations include gingivitis, stomatitis, aphthous ulceration, and gingival hypertrophy.
Noninfectious skin manifestations include photosensitivity, granulomatous lesions, vasculitis, and excessive inflammation at drainage and surgical wounds leading to dehiscence.
Autoimmune disorders are common. Autoimmune diseases reported in individuals with CGD include idiopathic thrombocytopenic purpura, juvenile idiopathic arthritis, autoimmune pulmonary disease, myasthenia gravis, IgA nephropathy, antiphospholipid syndrome, and recurrent pericardial effusion [Winkelstein et al 2000, De Ravin et al 2008].
Malignancies have been reported in CGD, and may be more common in autosomal recessive CGD than in X-linked CGD, raising the possibility that the increased incidence of malignancy is due to other cosegregating autosomal recessive traits [Aguilera et al 2009, Geramizadeh et al 2010, Lugo Reyes et al 2011].
The histopathologic patterns of malignancy have significant overlap with certain chronic inflammatory conditions. However, the largest series to date reported no malignancies [Winkelstein et al 2000, van den Berg et al 2009]. Smaller, more recent series corroborate a low overall incidence of malignancy [Köker et al 2013, Raptaki et al 2013, Baba et al 2014, Al-Zadjali et al 2015].
Survival in CGD has improved greatly, and is now approximately 90% at age ten years [Jones et al 2008, Martire et al 2008, Kuhns et al 2010, Marciano et al 2015]. Overall rates of survival are lower among those with X-linked CGD than those with autosomal recessive CGD.
Survival is influenced by several factors:
- Residual superoxide production, which correlates most directly with overall survival [Kuhns et al 2010] (see Genotype-Phenotype Correlations):
- Persons with NCF1 pathogenic variants have relatively good overall survival (>80% beyond age 40 years), which is similar to the survival rate in persons with CYBB pathogenic missense variants associated with residual superoxide production.
- Persons with CYBB pathogenic variants that result in no superoxide production have a survival of approximately 55% beyond age 40 years.
- Use of azoles for antifungal prophylaxis and therapy. Several series [Jones et al 2008, Kobayashi et al 2008, Martire et al 2008, Marciano et al 2015] report increased survival rates over the past 20 years:
- 88%-97% at age 10 years
- 73%-87% at age 20 years
- 46%-55% at age 30 yearsNote: Patients diagnosed and treated before the use of azoles usually did not survive past age 30-40 years.
- Access to care and expertise of caregivers
- Post-infectious complications such as hepatic nodular regenerative hyperplasia and portal venopathy associated with liver abscess, which contribute to overall morbidity and mortality [Marciano et al 2004, Hussain et al 2007, Feld et al 2008]
Note: Inflammatory bowel disease does not influence mortality: overall survival rates of persons with CGD with and without colitis are similar [Marciano et al 2004, Kuhns et al 2010, Marciano et al 2015].
Hypomorphic (variant) CGD is characterized by partial protein expression/function and residual superoxide production (observed in autosomal recessive CGD and protein-positive X-linked CGD). Affected individuals typically have a milder course and come to clinical attention later in life than those with absent protein expression [Bender et al 2009].
Carriers of X-Linked CGD
Female carriers of a CYBB pathogenic variant are typically unaffected, as the amount of gp91phox produced by their normal CYBB allele allows adequate superoxide production. However, some women are affected because they express primarily the CYBB disease-causing allele as the result of skewed (non-random) X-chromosome inactivation. These women may develop clinical evidence of CGD [Johnston 1985, Anderson-Cohen et al 2003]:
- The most common findings are cutaneous lesions resembling discoid lupus and recurrent aphthous stomatitis [Hafner et al 1992].
- In a prospective study of 19 women known to carry a CYBB pathogenic variant, Cale et al [2007] found a history of photosensitive skin rashes (58%), mouth ulcers (42%), and joint pain (37%). Most of these women had negative lupus serology.
- Chorioretinal lesions and granulomata with pigment clumping that are usually asymptomatic have been detected in females who are carriers of a CYBB pathogenic variant [Wang et al 2013].
- Lewis et al [2008] reported a female age 16 years with X-linked CGD in whom methylation analysis demonstrated skewed X-chromosome inactivation resulting in expression of the CYBB pathogenic variant inherited from her mother.
- Gono et al [2008] reported a woman age 28 years with CGD resulting from a de novo CYBB pathogenic variant on her paternally inherited X chromosome and skewed X-chromosome inactivation of her maternally inherited X chromosome.
- Wolach et al [2005] reported somatic mosaicism for a CYBB pathogenic variant in a woman with findings consistent with X-linked CGD at age 66 years. They suggested that the pathogenic variant probably originated in her bone marrow.
Genotype-Phenotype Correlations
Historically, it has been recognized that pathogenic variants in CYBB (the cause of X-linked CGD) give rise to a more serious phenotype than pathogenic variants causing autosomal recessive (AR) forms of CGD. Compared to persons with AR-CGD, males with X-linked CGD are typically diagnosed earlier and have a significantly higher incidence of perirectal abscess, suppurative adenitis, gastric outlet obstruction, urinary obstruction, and higher mortality at a young age.
Genotype-phenotype correlations in the X-linked gene CYBB (encoding gp91phox) include the following:
- All nonsense variants or deletions of CYBB in males are highly deleterious and associated with poorer outcomes.
- Pathogenic missense variants that occur in the CYBB region encoding amino acids 1-309 are associated with residual superoxide production at a level sufficient for good overall survival. Exceptions are pathogenic variants in the nucleotides encoding histidine at residue 222, which do not support production of residual superoxide and, therefore, are more deleterious.
- CYBB regions encoding amino acid residues 310 and beyond affect the FAD- and NADPH-binding domains that are essential for superoxide function. Even when pathogenic variants in this region allow protein expression, the proteins are nonfunctional and associated with poorer overall outcomes in affected males. Therefore, protein expression is neither reliable nor useful as a predictor of residual superoxide production [Kuhns et al 2010].
- The phenotype caused by pathogenic variants in CYBB associated with residual superoxide production is characterized by better survival than with CYBB variants that cause no residual superoxide production.
- Of note, the occurrence of inflammatory bowel disease in CGD is not correlated with superoxide production or mortality [Bender et al 2009, Kuhns et al 2010].
- Kuhns et al [2010] detemined that the level of residual neutrophil superoxide production influences morbidity and survival rates in persons with CGD. The production of reactive oxygen intermediates (ROI) was measured using the cytochrome c reduction assay (see Research testing) and the DHR test (see Diagnosis, Laboratory testing). Protein expression was determined using the immunoblot test for the NADPH complex proteins (see Research testing). Persons with modest ROI production have less severe illness and higher long-term survival than those with little ROI production.
- ROI production may be predicted by the specific pathogenic variant type and gene:
- Lower ROI production is associated with decreased survival and was observed in persons with deletions and nonsense, frameshift, and some splice variants.
- Higher ROI production and increased survival were observed in persons with CYBB pathogenic missense variants between amino acids 1 and 309 (with the exception of histidine 222) or pathogenic variants in NCF1 [Kuhns et al 2010].
Complete CYBA pathogenic variants lead to absent protein expression and thereby disable the formation of the cytochrome complex. These variants therefore behave like the most deleterious of the CYBB pathogenic variants.
Nomenclature
When first characterized, chronic granulomatous disease was called "fatal granulomatous disease of childhood" [Bridges et al 1959].
Prevalence
The retrospectively and voluntarily reported prevalence of CGD is approximately 1:200,000 live births in the United States [Winkelstein et al 2000].
Prevalence rates in other countries vary somewhat based on social, religious, and cultural factors that influence birth rates and frequency of consanguinity [Wolach et al 2008, Fattahi et al 2011].
- Sweden: 1:450,000 [Ahlin et al 1995]
- Japan: 1:300,000 [Hasui & Japa 1999]
- United Kingdom: 1:133,000 [Jones et al 2008]
- Israel [Wolach et al 2008]
- Arabs: 1:111,000
- Jews: 1:218,000
- Italy: 1:1,000,000 [Martire et al 2008]
- Greece: 2.2:100,000 [Raptaki et al 2013]
Importantly, in regions with high rates of consanguineous marriages, the prevalence of recessive forms of CGD exceeds that of X-linked CGD.
Differential Diagnosis
The differential diagnosis of chronic granulomatous disease (CGD) mainly involves disorders with recurrent or unusual infections or disorders associated with granuloma formation and hyperinflammation. The following disorders should be considered.
Cystic fibrosis. Individuals with cystic fibrosis may develop pulmonary infections with Burkholderia cepacia complex. Unlike in CGD, these infections are typically isolated to the lung and occur concurrently with significant bronchiectasis. Individuals with CGD are prone to recurrent infection with different strains of Burkholderia cepacia complex, whereas those with cystic fibrosis are often persistently infected with the same strain [Greenberg et al 2009].
Hyper IgE syndrome. Staphylococcal and Aspergillus infections are common in individuals with autosomal dominant STAT3-deficient hyper IgE syndrome (AD-HIES). However, those with AD-HIES also have characteristic facies, skeletal abnormalities, and markedly elevated IgE levels [Freeman & Holland 2009].
Allergic bronchopulmonary aspergillosis (ABPA). ABPA is a pulmonary hypersensitivity reaction to Aspergillus fumigatus and other molds and is most commonly seen in asthmatics and persons with cystic fibrosis. The diagnosis is based on history, elevated serum concentration of IgE, blood eosinophilia, immediate skin reactivity to Aspergillus fumigatus antigens, presence of precipitating serum antibodies to Aspergillus fumigatus, and specific imaging results, none of which are characteristic of CGD [Greenberger 2002].
Glucose 6-phosphate dehydrogenase (G6PD) deficiency (OMIM 300908) and glutathione synthetase (GS) deficiency (OMIM 266130). Deficiencies in G6PD and GS affect the neutrophil respiratory burst and can increase host susceptibility to infections. Both disorders are associated with hemolytic anemia; GS deficiency is associated with 5-oxoprolinuria and intellectual disability, features not seen in CGD [Whitin & Cohen 1988, Ristoff et al 2001].
Crohn disease. Significant colitis leading to bowel obstruction, fistulae, and strictures can occur in patients with CGD and can be an important cause of growth retardation [Marciano et al 2004]. Persons with Crohn disease also can present with weight loss, abdominal pain, diarrhea, and colitis.
Other. Spontaneously occurring severe or recurrent bacterial infections should always prompt consideration of immune deficiency. Persons with recurrent soft tissue infections or staphylococcal lymphadenitis should be evaluated for CGD. Presence of liver abscess or other deep tissue abscesses is concerning for CGD as well as other immunodeficiencies.
Other conditions that may affect the ability of the neutrophil to generate the respiratory burst that is detected in the DHR assay include myeloperoxidase deficiency (OMIM 254600) [Mauch et al 2007] and SAPHO (the syndrome of synovitis, acne, pustulosis, hyperostosis, and osteitis) (OMIM 612852) [Ferguson et al 2008]. In these two conditions the DHR results are abnormal, but superoxide production levels and NBT staining are normal. In addition, neither of these syndromes has overlapping infection profiles with CGD.
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs of an individual diagnosed with chronic granulomatous disease (CGD), evaluation should include the following:
- Consultation with a clinical geneticist and/or genetic counselor
- Tests looking for evidence of infection, such as C reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which are sensitive but nonspecific markers of inflammation
- Complete blood count (CBC). Anemia is common either due to anemia of chronic disease or iron deficiency anemia. Poor iron absorption is common in CGD-related colitis.
- Albumin. Hypoalbuminemia is found in 70% of persons with GI involvement and in 25% of persons without GI manifestations [Marciano et al 2004].
- Endoscopy and colonoscopy if signs and symptoms of colitis are present
- Imaging as it pertains to specific symptoms for diagnosis and management of infection. Because CGD can affect almost every organ system, different imaging modalities can be used depending on the site affected. Because of its relative ease and sensitivity, CT scan is often used; however, ultrasound and MRI can be used instead in many instances. Positron emission tomography (PET) using fluorine-18-fluoro-2-deoxy-D-glucose (FDG) uptake can help discriminate active from resolved infection. High FDG uptake is consistent with active inflammation [Güngör et al 2001].
Affected Organs / Manifestations of CGD on Imaging
Lungs / pneumonia [Godoy et al 2008]
- Chest x-ray. Consolidation, reticular nodular opacities, scarring
- CT
- Consolidation, ground-glass opacity, tree-in-bud opacity, centrilobular or random nodules, septal thickening, air trapping, scarring
- Empyema or abscess
- Mediastinal or hilar adenopathy, honeycomb lung, pleural thickening in chronic cases
- Contiguous spread to chest wall, associated osteomyelitis of ribs and vertebral bodies
Lymph nodes / suppurative adenitis [Towbin & Chaves 2010]
- CT. Enhancing lymph node with central area of hypodensity and enhancing septations
- US
- Swirling debris, thickened septa, and increased color Doppler flow
- Calcifications if granuloma present
Liver / abscess [Garcia-Eulate et al 2006]
- Single to multiple small or large abscesses, sharply defined; variable enhancement but usually with small central area with poor enhancement
- Calcifications
Musculoskeletal / osteomyelitis [Galluzzo et al 2008]
- Multifocal, occurring in ribs, vertebral bodies, small bones of hands and feet
Genitourinary / cystitis [Walther et al 1992]
- Inflammatory pseudotumors of the bladder; on US appear as focal wall thickening
Gastrointestinal / obstruction and colitis [Marciano et al 2004, Laskey et al 2009]
- Obstruction
- Esophagus: strictures, diverticula, dysmotility
- Thickening of bowel wall, fistulae
- Upper GI: gastric outlet obstruction with gastric dilation, delayed gastric emptying, circumferential antral narrowing, thickened gastric folds
- Gastric wall thickening on US, CT, or MRI
- Colitis: Bowel wall thickening, skip lesions, luminal narrowing, fistulae, cobblestone mucosal pattern
Head and neck / sinusitis [Towbin & Chaves 2010]
- MRI. Fungal sinusitis hypointense on T1- and T2-weighted images, associated with bony destruction
- CT. Fungal sinusitis hyperdense
Central nervous system / abscess [Towbin & Chaves 2010]
- Abscesses with typical appearance on MRI with ring-enhancing lesions
Treatment of Manifestations
Serious infections may occur at any time in persons with CGD. Infections that are asymptomatic or minimally symptomatic may be identified at initial presentation. Significant rises in CRP or ESR should prompt evaluation for infection. Imaging is important in detecting and understanding the severity of infections. CT or MRI should be followed closely until resolution of infections.
A definitive microbiologic diagnosis is essential to proper treatment of infections. Biopsies to identify the pathogen should be pursued prior to initiation of antimicrobial therapy unless infections are life threatening. Often obtaining an appropriate sample for diagnosis requires fine needle aspiration or percutaneous drainage of an abscess.
Initially antibiotics and antifungals are often used empirically, with more selective use after the pathogen is identified. Newer azole drugs (voriconazole, posaconazole, isovuconazole) have expanded therapeutic options for fungal infections in CGD. Long courses of antimicrobials are often needed for adequate treatment. For example, those who do develop fungal infections on itraconazole prophylaxis develop them at an older age and may require longer duration of therapy.
The primary prophylaxis used to prevent bacterial and fungal infections also has good activity against yeasts. However, if invasive yeast infections occur, organism-specific antimicrobials are warranted.
Percutaneous drainage itself can be therapeutic, especially for liver or other intra-abdominal abscesses. Lymphadenitis and liver abscesses often require excisional surgery [Feld et al 2008]. Staphylococcal liver abscesses can be effectively treated without surgery using a combination of drainage of liquid pus (if present), intravenous antimicrobials, and moderate dose corticosteroids (1 mg/kg/day tapered over 1-2 months) [Leiding et al 2012].
Colitis. Treatment of colitis in CGD can be difficult.
Corticosteroids are usually effective but have long-term complications including growth retardation, osteoporosis, and increased risk of infection. The authors' current practice is to initiate therapy for proven colitis with prednisone 1 mg/kg/day for one to two weeks followed by a slow taper to 0.1-0.25 mg/kg/day over one to two months [Holland 2010].
Metronidazole to reduce bowel flora, salicylic acid derivatives, 6-mercaptopurine, and mesalamine are also useful in treatment of CGD colitis.
In CGD, the use of TNF-alpha inhibitors, specifically infliximab, a chimeric (mouse/human) monoclonal antibody to TNF alpha, is successful in closing fistulae but leads to increased frequency of severe infections with typical CGD pathogens or death. A report of infliximab in five persons with CGD found severe infections in all five and death in two. Of note, none of the five developed mycobacterial infections, as has been reported with use of infliximab in other conditions [Uzel et al 2010].
Successful bone marrow transplantation appears to cure CGD and the related colitis [Kang et al 2011].
Corticosteroid treatment of heightened inflammatory response. Simultaneous administration of antimicrobials and corticosteroids can help resolve the infections and extensive areas of inflammation that can occur with chronic colitis [Marciano et al 2004], granulomatous cystitis [Kontras et al 1971], pulmonary infections with Nocardia [Freeman et al 2011], and staphylococcal liver abscesses [Leiding et al 2012].
Successful treatment of mulch pneumonitis, the exuberant inflammatory response following inhalation of mulch or other organic matter, requires the simultaneous administration of antifungals and corticosteroids [Siddiqui et al 2007].
Aggressive treatment of the syndrome of secondary hemophagocytic lymphohistiocytosis (HLH) in CGD with antimicrobials, IVIg, and steroids can lead to clinical improvement and remission [Parekh et al 2011]. Because the HLH-like syndrome in CGD represents a reaction to bacterial or fungal infection, these infections must be aggressively treated if patients receive immunosuppression for HLH. Although the merit of immunosuppression in the setting of infection-triggered HLH in CGD is unclear, treatment of the infection is essential.
Granulocyte infusions. The value of granulocyte infusions has not been evaluated in prospective controlled trials; however, multiple case reports suggest its utility in treating serious bacterial and fungal infections [von Planta et al 1997, Ozsahin et al 1998, Bielorai et al 2000, Ikincioğullari et al 2005]. The principle is that a small number of normal phagocytes complement the oxidative defect in CGD phagocytes by supplying diffusible hydrogen peroxide. Transfused granulocytes have been recovered from sites of infection and appear to have normal respiratory burst activity and to traffic normally.
Granulocyte infusions are generally well tolerated; however, adverse effects include fever, development of leukoagglutinins, and rarely, pulmonary leukostasis. Alloimmunization is a major concern, as many patients with histories of severe infections may also be considered for hematopoietic stem cell transplantation (HSCT) [Heim et al 2011]. The possibility of CMV transmission is also a cause for caution.
Males with X-Linked CGD
For males with X-linked CGD and McLeod neuroacanthocytosis syndrome, early consideration should be given to autologous blood banking (see also Establishing the Diagnosis, Special Consideration in a Male with Suspected CGD and Other Medical Issues). Persons with McLeod neuroacanthocytosis syndrome do not express the erythrocyte blood group Kell antigen (i.e., they are Kell negative). Should they require transfusion of blood products, Kell-positive blood products must be avoided in order to prevent a transfusion reaction. Kell-negative blood products are rarely available.
Prevention of Primary Manifestations
Antibacterial prophylaxis. No randomized prospective clinical trials of antibacterial prophylaxis in persons with CGD have been performed; however, several retrospective studies suggest that trimethoprim-sulfamethoxazole (TMP-SMX) is effective in preventing bacterial infections. Lifelong daily antibacterial prophylaxis with oral TMP-SMX is recommended at 5 mg/kg up to 320 mg administered in two divided doses. Note: In liquid TMP-SMX the concentration of TMP is 40 mg / 5 mL and sulfamethoxazole 200 mg / 5 mL; the therapeutic dose of TMP-SMX is determined by the TMP component.
Alternatives to TMP-SMX for patients allergic to sulfonamides include trimethoprim as a single agent, dicloxacillin, cephalosporins, and fluroquinolones.
Antifungal prophylaxis. The use of azole antifungal drugs has markedly reduced the frequency and severity of fungal infections in CGD. Lifelong antifungal prophylaxis with itraconazole 5 mg/kg oral solution to a maximum of 200 mg once daily is recommended [Gallin et al 2003].
In a randomized trial, 39 patients were assigned to receive either placebo or itraconazole (100 mg/day in patients age 5-12 years; 200 mg/day in those age >13 years and weight >50 kg); only one person receiving itraconazole had a serious fungal infection compared to seven in the placebo group [Gallin et al 2003].
For those unable to tolerate itraconazole, posaconazole has been studied in the oncology setting and is likely to be effective in CGD as well [Segal et al 2005].
Of note, the primary prophylaxis used to prevent bacterial and fungal infections also has good activity against yeasts.
Immunomodulatory therapy. Interferon gamma (IFN-gamma) has become part of the prophylactic regimen in most centers in the United States; however, opinions differ on its use as primary prophylaxis and in the treatment of acute infections. The exact mechanism of IFN-gamma in CGD is not known, adding to the debate over its utility.
An international multicenter randomized prospective placebo-controlled trial showed a decrease in the rate of serious infections in the group receiving IFN-gamma (22%) versus placebo (46%) after a follow-up period of 8.9 months. This improvement was independent of age, CGD genotype, or concomitant use of other prophylactic antibiotics. Three prospective Phase IV trials showed decreased rates of infections ranging from 0.13 to 0.4 per patient year. However, one prospective study comparing treatment with TMP-SMX and itraconazole alone versus addition of IFN-gamma showed no difference in the rates of infection [Martire et al 2008].
Some practitioners use IFN-gamma only in the setting of acute infection, rather than as primary prophylaxis. The data for this are anecdotal and unimpressive. The authors typically discontinue IFN-gamma during acute infection, as its utility is unclear and the exacerbation of malaise and fever can confuse the clinical picture and alter decision-making [Holland 2010].
Administration by injection, cost, and lack of familiarity with cytokine therapy all affect the use of IFN-gamma in CGD. The authors use IFN-gamma in addition to antimicrobials as prophylaxis [Holland 2010]. Dosing is based on body surface area (BSA). For BSA >0.5/m2 the dose is 50 μg/m2 subcutaneously 3x/week; for BSA ≤0.5/m2 the dose is 1.5 μg/kg subcutaneously 3x/week. Fever, myalgias, and malaise are the most common side effects but can be alleviated with concurrent administration of acetaminophen.
Hematopoietic stem cell transplantation (HSCT). Allogeneic HSCT is the only known cure for CGD. Historically, HSCT has been associated with high morbidity and mortality and thus reluctantly offered. However, the use of non-myeloablative conditioning regimens has greatly decreased the risk of regimen-related toxicity as well as allowing for transplantation in the setting of active infection; recent reports place transplant survival at greater than 90% [Güngör et al 2014] with roughly equal survival among patients with matched related, matched unrelated, and umbilical cord blood donors.
The issue of which individuals with CGD should undergo HSCT remains complex. While transplant-related mortality rates have fallen dramatically and successful cure has risen, issues of long-term risk, sterility, graft-versus-host disease, donor matching, expense, center experience, availability, and insurance coverage all strongly influence family and physician choices regarding transplantation. Levels of residual superoxide production have correlated well with overall survival [Kuhns et al 2010]; that is, individuals with very low superoxide production had worse long-term survival than those with higher levels of residual superoxide production, suggesting that this latter group could benefit more from transplantation. However, even within this group some patients do relatively well for long periods.
Patients with CGD may experience behavioral, emotional, and learning difficulties as a consequence of chronic disease, recurrent hospitalization, and limitations of activity. Older children and adolescents are especially likely to be noncompliant with respect to prophylaxis and risk avoidance, increasing their risk for CGD-related complications. The inflammatory bowel disease present in up to 50% of persons with X-linked CGD may result in discomfort and growth impairment, and may require colostomy or colectomy. Overall quality of life is reduced in children with CGD, whereas patients with CGD who have undergone transplant report quality of life comparable to healthy children [Cole et al 2013]. Thus, with improved outcomes HSCT presents an increasingly reasonable alternative and the possibility of a normal life.
As HSCT becomes safer, more reliable, and more available it will likely be an early and initial choice for the management of CGD. Currently, many centers offer HSCT after the first life-threatening infection, but with advances in the technique, the availability of donors, especially for minority populations, and the availability of experienced centers, that equation and timing may change. Even without HSCT the majority of persons with CGD will live into adulthood. There is currently very little difference in overall survival over the first decades of life between medical and transplant management. However, the significant mortality in medical management begins to accrue after age 20 [Kuhns et al 2010]. Aggressive prophylaxis and infection management increase the likelihood of doing well.
The European Bone Marrow Transplantation (EBMT) Working Group 2011 statement [EBMT Working Group 2011] recommends allogeneic bone marrow transplantation for CGD in the case of unavailability of reliable specialist medical care, noncompliance with long-term antibiotic/antifungal prophylaxis, one or more life-threatening infections, severe granulomatous disease with progressive organ dysfunction (e.g., lung restriction), steroid-dependent granulomatous disease (e.g., colitis), or ongoing therapy-refractory infection (e.g., aspergillosis).
Surveillance
Regular follow-up visits can aid in early detection and treatment of asymptomatic or minimally symptomatic infections and noninfectious complications such as colitis, pulmonary granulomas, and pulmonary fibrosis [Roesler et al 2005].
- Laboratory examinations include CBC, chemistries, CRP, and ESR.
- Significant rises in CRP or ESR should prompt evaluation for infection.
- Presence of microcytic anemia and hypoalbuminemia may indicate development of colitis.
- Monitor liver chemistries for transaminase and alkaline phosphatase elevation, especially drug-related hepatotoxicity.
- Although imaging is also important in detection of infectious and noninfectious manifestations, no specific guidelines address the intervals at which imaging should be used. CT or MRI should be followed closely to monitor progression of disease or until resolution of infections.
Frequent follow-up visits also provide the treating clinician opportunities to encourage compliance with prophylaxis and educate the patient and family about the disease.
Agents/Circumstances to Avoid
Exposures. Activities that expose the affected person to decayed organic matter (e.g., mulching, gardening, leaf raking, house demolition) are to be avoided as inhalation of fungal spores can result in fulminant pneumonitis leading to hypoxia and respiratory failure [Siddiqui et al 2007]. Therefore, the following should be avoided:
- Exposure to mulch
- Potting of plants or gardening
- Raking leaves or mowing lawns
- Swimming in stagnant water, brackish water, or ponds
BCG vaccination should be avoided (live viral vaccines are likely safe).
Transfusion considerations. Persons with CGD and McLeod neuroacanthocytosis syndrome lack red blood cell Kell antigens and thus should not receive blood transfusions that are Kell antigen positive.
Evaluation of Relatives at Risk
It is appropriate to evaluate apparently asymptomatic at-risk relatives in order to identify as early as possible those who would benefit from initiation of treatment and preventive measures.
Evaluations can include the following:
- Molecular genetic testing if the pathogenic variant(s) in the family are known
- Routine DHR testing of peripheral blood, which will detect the CGD disease state (except for p40phox deficiency), if the pathogenic variant(s) in the family are not known
See Genetic Counseling for issues related to testing of at-risk relatives for genetic counseling purposes.
Pregnancy Management
The major concern during the pregnancy of a woman known to have CGD is continued use of prophylactic antimicrobials.
- Trimethoprim, a folic acid antagonist, is usually avoided in pregnancy
- Sulfamethoxazole is not known to increase the risk of birth defects in humans; however, it is typically administered in conjunction with trimethoprim for prophylaxis in affected non-pregnant women.
- Data regarding teratogenicity of itraconazole are limited. Although case reports of birth defects in infants born to women taking itraconazole during pregnancy have been published, this observation is not supported by larger case series. Given the lack of adequate data on the use of itraconazole during pregnancy, some practitioners suggest that it should be avoided during pregnancy until such data become available.
The authors' practice for women with CGD who are or are planning to become pregnant is to use antibacterial prophylaxis (e.g., penicillin- or cephalosporin-based therapies) for which more data on safety during pregnancy exist [Author, personal communication]. Although no antifungal prophylactic medications known to be completely safe during pregnancy are currently available, the risks and benefits of antifungal treatment must be weighed case by case. Interferon gamma is held during pregnancy and restarted after breastfeeding has ceased.
Therapies Under Investigation
Gene therapy. CGD is an attractive target for gene therapy: the disorder results from a single gene defect, neutrophil superoxide production can be reconstituted in vitro, and correction of neutrophil superoxide production need not be complete to provide complete protection, as exemplified by X-linked carriers. Although initially unsuccessful, more recent gene therapy efforts have been encouraging.
Early trials using retrovirus-based therapy were complicated by loss of engraftment. Most forms of CGD gene therapy seek to introduce a retroviral vector containing normal CYBB into mobilized CD34 stem cells. Ott et al [2006] reported successful early levels of gene-corrected oxidase-producing circulating neutrophils in two adults with X-linked CGD. While there was initial clinical benefit to both patients, over time gene silencing with loss of oxidase activity and myelodysplasia developed. Kang et al [2010] reported three individuals with X-linked CGD who underwent gene therapy: two had low-level correction of neutrophil superoxide production. One had resolution of infection with 1.1% of neutrophils regaining gp91phox expression. The lack of an intrinsic survival advantage for gene-corrected CGD cells further complicated low rates of correction. All three individuals lost corrected gene expression over the course of several months.
Hematopoietic gene therapy in general and in CGD in particular has been complicated by the development of hematologic malignancies [Ott et al 2006, Stein et al 2010]. Two adults who were treated with retrovirus-based therapy developed monosomy 7 secondary to retroviral insertional activation of transcription of the oncogene MECOM (MDS and EVI1 complex locus).
Promising results with the use of lentiviral vectors in a murine X-linked CGD model have been obtained [Chiriaco et al 2014]. Recently an international study using a lentiviral vector encoding a chimeric myeloid promoter in patients with X-linked CGD has opened. As is true for many forms of hematopoietic stem cell gene therapy, the treatment of CGD will require some chemotherapeutic bone marrow conditioning to facilitate long-term corrected cell engraftment and persistence.
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for information on clinical studies for a wide range of diseases and conditions.