Hemolytic Anemia Due To Red Cell Pyruvate Kinase Deficiency
A rare, genetic metabolic disorder due to pyruvate kinase deficiency characterized by a variable degree of chronic nonspherocytic hemolytic anemia resulting in a variable clinical manifestations ranging from fatal anemia at birth to a to a fully compensated hemolysis without apparent anemia.
Epidemiology
Pyruvate kinase (PK) deficiency is the most frequent cause of congenital nonspherocytic hemolytic anemia with a prevalence estimated at 1/20,000 in the general white population.
Clinical description
Clinically, PK-deficient patients suffer from a highly variable degree of chronic hemolysis, ranging from severe neonatal jaundice and fatal anemia at birth, severe transfusion-dependent chronic hemolysis, moderate hemolysis with exacerbation during infection, to a fully compensated hemolysis without apparent anemia. Symptoms are usually present at birth but, due to the variable severity, may not be recognized or acknowledged until later. Chronic icterus, gallstones, iron overload and splenomegaly are common findings.
Etiology
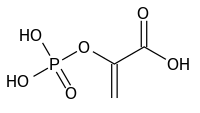
Erythrocyte PK deficiency is caused by mutations in the PKLR gene (1q22). To date, more than 290 mutations in PKLR have been reported. PK is a key regulatory enzyme of glycolysis and two major metabolic abnormalities result from PK deficiency: ATP depletion and increased 2,3-diphosphoglycerate (2,3-DPG) content. The precise mechanisms that cause extravascular hemolysis are as yet unknown, but an important feature involves the selective sequestration of PK-deficient young red blood cells, in particular reticulocytes, by the spleen. The increased 2,3-DPG levels ameliorate the anemia by lowering the oxygen-affinity of hemoglobin.
Diagnostic methods
Diagnosis may be considered on the basis of the clinical features and laboratory findings: a variable degree of anemia, reticulocytosis, increased non-conjugated bilirubin, and decreased levels of haptoglobin. Red blood cell morphology is essentially normal. PK deficiency is diagnosed by measuring PK enzymatic activity. Importantly, due to the fact that the enzymatic activity is red cell age-dependent, a deficiency of PK may be masked by reticulocytosis. Simultaneous measurement of another red cell age-specific enzyme, e.g. hexokinase, may therefore be helpful. Confirmation of the diagnosis requires genetic testing.
Differential diagnosis
Secondary PK deficiency has also been reported, occurring in the context of hematological diseases (acute/chronic leukemia, myelodysplastic syndromes and sideroblastic anemia). In case of persistent normocytic hemolytic anemia in which hemoglobin abnormalities and antiglobulin reactions have been excluded, spherocytes are absent, and osmotic fragility is normal, the diagnosis of hereditary nonspherocytic hemolytic anemia should be considered.
Genetic counseling
Erythrocyte PK deficiency is an autosomal recessive disease and genetic counseling should be offered to affected families. Where both parents are unaffected carriers, there is a 25% risk of disease transmission to offspring.
Management and treatment
The mainstay of treatment is blood transfusion and, in severe cases, splenectomy. The latter should be based on the patient's ability to tolerate the anemia. As a result of splenectomy, transfusion needs are reduced in many patients. Splenectomy is often accompanied by a considerable increase in reticulocyte counts. Bone marrow transplantation can cure PK deficiency but is rarely performed. Small molecule activator therapy is currently in clinical trials.
Prognosis
Prognosis is variable depending on the severity of the anemia, but as in other chronic hemolytic disorders, gallstones and iron overload may develop, requiring appropriate treatment.