Mucoepithelial Dysplasia, Hereditary
Description
Hereditary mucoepithelial dysplasia (HMD) is a rare autosomal dominant genodermatosis characterized by onset in infancy of a panepithelial defect involving the oral, nasal, conjunctival, vaginal, cervical, perineal, urethral, and bladder mucosa. Patients develop cataracts, blindness, nonscarring alopecia, perineal psoriasiform lesions, and follicular keratoses (Witkop et al., 1982). Although 1 family was reported to have progressive severe interstitial lung disease (Witkop et al., 1979), this feature has not been reported in other families and is not considered a criterion for diagnosis (review by Boralevi et al., 2005).
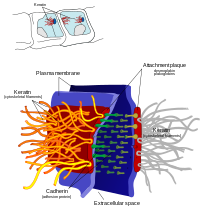
Clinical FeaturesWitkop et al. (1979) described a 4-generation kindred with a disorder termed hereditary mucoepithelial dysplasia, characterized by flat red lesions affecting the periorificial mucosa and by follicular keratosis of the skin. Affected individuals had severe photophobia and nystagmus in infancy followed by keratitis, pannus, and cataracts in childhood. Nonscarring alopecia was also a feature. Vaginal, oral, and urinary PAP smears showed large immature cells containing vacuoles and strand-shaped inclusions. Histologic studies of the mucosa showed dyshesion, dyskeratosis, and lack of cornification. Ultrastructural studies of epithelial cells showed lack of keratohyalin, reduced numbers of desmosomes, and intracytoplasmic accumulation of standard material resembling desmosomes and gap junctions. In addition, patients had repeated pneumonia in childhood followed by fibrocystic lung disease and cor pulmonale in adulthood. Witkop et al. (1979) concluded that there was a defect in desmosome and gap junction formation.
Witkop et al. (1979) concluded that the family reported by Okamoto et al. (1977) as 'chronic mucocutaneous candidiasis' in fact had hereditary mucoepithelial dysplasia. Two (possibly 3) generations of the family were affected with early-onset, mild mucocutaneous candidiasis, increased susceptibility to bacterial infection, hyperkeratosis follicularis, alopecia universalis, keratoconjunctivitis, diarrhea in infancy, T- and B-cell abnormalities, and possibly hypoadrenocorticism. A mother and her 2 daughters were studied in detail. The mother became legally blind by her teens. She had cataracts as well as a densely hazy and vascularized cornea. She wore a wig from age 6 years. Candidiasis affected the corners of her mouth, and she had candida vulvovaginitis that was occasionally complicated by bacterial infection. Chronic monilial nail infection began in her late teens. The 2 daughters were experiencing a similar evolution of disease. One of them had slit-lamp signs of keratoconjunctivitis with mild vascularization of the cornea at the age of 18 months. Watery diarrhea occurred episodically in both girls. The maternal grandfather of these girls was probably affected. He had progressive blindness in his 20s and his skin was rough and dry and appeared tanned (as did his daughters') even in winter. He died unexpectedly at age 36 years while recovering from bacterial pneumonia. At autopsy, the adrenal cortices were questionably thin. Noteworthy is the fact that when the patient was born, his father was 52 years old. Witkop et al. (1979) reported that vaginal Pap smear in the mother showed cytoplasmic inclusions. They concluded that the evidence for an immune or endocrinologic defect was 'tenuous.' Misinterpretation of abnormal results from cervical Pap smears may lead to hysterectomy being performed unnecessarily in these patients (Scheman et al., 1989).
Witkop et al. (1982) provided a detailed report of the ocular features in 2 affected members of the family reported by Witkop et al. (1979). At age 6 months, the first had severe photophobia, tearing, nystagmus, pannus formation, and corneal vascularization. By age 3.5 years, she had corneal scar tissue, more pannus formation, opacified corneal epithelium, subcapsular cataract, and visual impairment. The second patient had photophobia, tearing, and esotropia in the neonatal period. He had keratoconjunctivitis with vascular opacified corneas at age 2.5 years and cataracts at age 6. Radiation and graft treatment failed, and he became blind. Pathologic findings of ocular tissue (conjunctiva, cornea) showed lack of desmosomes, basal cells with numerous cytoplasmic vacuoles, pleomorphic nuclei, dyskeratotic cells, and variation in epithelial thickness.
Urban et al. (1991) described a 5-generation kindred in which affected persons had the characteristic histologic findings of this disorder, including dyskeratosis on light microscopy and a paucity of gap junctions and desmosomes on electron microscopy, but a somewhat different clinical spectrum and a more benign course, most notably lack of pulmonary involvement. A fiery red coloration of the gingiva and adjacent hard palate was illustrated.
Rogers et al. (1994) reported a 20-year-old Australian man with sporadic progressive HMD. He had blepharitis, conjunctivitis, corneal opacities, and superficial corneal vascularization with severely reduced visual acuity. He also had sparse hair and eyebrows, psoriasiform plaques over the joint surfaces, keratitis pilaris, bright red tongue, and a dry hyperkeratotic perianal rash. Although plasma zinc levels were normal, he showed some response to oral zinc therapy. Skin biopsies showed psoriasis with hyperkeratosis and reduced numbers of desmosomes. There were also cytoplasmic vacuoles, some of which contained lamellar or fragmented material.
Boralevi et al. (2005) reported a family in which 5 patients had hereditary mucoepithelial dysplasia. All had classic ocular and mucosal features of the disorder, but none had pulmonary involvement or diarrhea. Skin biopsies showed a psoriasiform pattern, dyskeratosis, and cytoplasmic vacuoles. Immunohistochemical studies of skin biopsies did not show abnormalities of keratins, connexins (which form gap junctions), or several other desmosomal proteins. Three sporadic patients were also described. Boralevi et al. (2005) postulated a defect in expression of cytoskeletal elements or a modification of mechanisms regulating junction-cytoskeletal assembly.
InheritanceWitkop et al. (1979) observed the disorder in 4 generations of a family consistent with autosomal dominant inheritance.
DiagnosisDifferential Diagnosis
Urban et al. (1991) suggested that this disorder should be considered in the differential diagnosis of childhood alopecia, follicular hyperkeratosis, keratoconjunctivitis, juvenile cataracts, gingival hyperemia, restrictive lung disease, and esophageal stenosis or webs.
Rothe and Lucky (1995) commented on the similarities between HMD and ichthyosis follicularis (IFAP; 308205), including keratosis pilaris, nonscarring alopecia, photophobia, psoriasiform plaques, and nail dystrophy.