Acute Intermittent Porphyria
Summary
Clinical characteristics.
Acute intermittent porphyria (AIP), an autosomal dominant disorder, occurs in heterozygotes for an HMBS pathogenic variant that causes reduced activity of the enzyme porphobilinogen deaminase. AIP is considered "overt" in a heterozygote who was previously or is currently symptomatic; AIP is considered "latent" in a heterozygote who has never had symptoms, and typically has been identified during molecular genetic testing of at-risk family members. Note that GeneReviews does not use the term "carrier" for an individual who is heterozygous for an autosomal dominant pathogenic variant; GeneReviews reserves the term "carrier" for an individual who is heterozygous for an autosomal recessive disorder and thus is not expected to ever develop manifestations of the disorder.
- Overt AIP is characterized clinically by life-threatening acute neurovisceral attacks of severe abdominal pain without peritoneal signs, often accompanied by nausea, vomiting, tachycardia, and hypertension. Attacks may be complicated by neurologic findings (mental changes, convulsions, and peripheral neuropathy that may progress to respiratory paralysis), and hyponatremia. Acute attacks, which may be provoked by certain drugs, alcoholic beverages, endocrine factors, calorie restriction, stress, and infections, usually resolve within two weeks. Most individuals with AIP have one or a few attacks; about 3%-8% (mainly women) have recurrent attacks (defined as >3 attacks/year) that may persist for years. Other long-term complications are chronic renal failure, hepatocellular carcinoma (HCC), and hypertension. Attacks, which are very rare before puberty, are more common in women than men.
- Latent AIP. While all individuals heterozygous for an HMBS pathogenic variant that predisposes to AIP are at risk of developing overt AIP, most have latent AIP and never have symptoms.
Diagnosis/testing.
The diagnosis of overt AIP in a symptomatic proband is based on detection of increased concentration of porphobilinogen (PBG) in urine on biochemical testing. Molecular genetic testing is not a first-line diagnostic test for probands; detection of a heterozygous HMBS pathogenic variant is mainly used in difficult diagnostic situations – for example, when the proband is not available for testing.
Management.
Treatment of manifestations: Acute neurovisceral attacks.
- Stop medications that can exacerbate AIP; provide adequate caloric intake by intravenous infusion if required (hypotonic dextrose water solutions should be avoided).
- Treat any intercurrent infections or disease using drugs known to be safe in acute porphyria.
- Treat pain with opiate analgesia (often in large amounts); support from a pain team may be required.
- Treat agitation, vomiting, hypertension, and tachycardia using non-porphyrinogenic drugs (those that will not act as triggers for acute porphyria; also known as "safe" drugs).
- Monitor fluid balance and correct electrolyte disturbances, especially hyponatremia; treat severe hyponatremia with saline infusions, not fluid restriction.
- Monitor neurologic status carefully and provide respiratory support as needed.
- Prompt administration of human hemin (panhematin or heme arginate) is the specific treatment of choice to curtail acute neurovisceral attacks and avoid paresis. Patients treated regularly with heme arginate require monitoring of iron status to detect iron overload.
Mild attacks. Manage by symptomatic treatment, increased calorie intake, and fluid replacement.
Recurrent acute attacks. Manage together with a porphyria specialist; treatment options include ovulation suppression with gonadorelin analogs, regular hematin infusions, or (as a last resort) liver transplantation.
Evaluation of relatives at risk: If the HMBS pathogenic variant is known in a family, at-risk relatives can benefit from molecular genetic testing to clarify their genetic status, so that those at increased risk of developing acute attacks of AIP can be identified early and counseled about preventive measures to reduce the risk of acute attacks.
Prevention of primary manifestations: All individuals with latent AIP, the parents of affected individuals, and patients with overt AIP who are in remission should be advised about measures that diminish the risk of acute attacks:
- Avoid precipitating factors (unsafe prescribed and illicit drugs, excessive alcohol consumption, smoking, and severe calorie restriction).
- Adopt safe practices (maintenance of a regular, balanced diet; prompt treatment of infections; and reduction of stress).
Surveillance: Individuals who have experienced acute attacks require monitoring of renal function; in some countries annual hepatic imaging to detect HCC is also offered to all individuals with an HMBS pathogenic variant after age 50 years (whether or not they have experienced acute attacks).
Therapies Under Investigation: Givosiran (ALN-AS1), an interference RNA that represses ALAS1, has completed Phase I and III clinical trials that showed reduction of 5-aminolevulinic acid and PBG excretion to near normal levels and a reduction in the rate of porphyria attacks when compared to a placebo.
Genetic counseling.
AIP is inherited in an autosomal dominant manner. Sibs and offspring of individuals with an HMBS pathogenic variant are at 50% risk of inheriting the HMBS pathogenic variant; however, because penetrance is low, the likelihood of an individual with an inherited HMBS pathogenic variant having an acute attack is small. Once an HMBS variant has been identified in an affected family member, prenatal testing for a pregnancy at increased risk and preimplantation genetic testing are possible. However, because clinical penetrance is low, the finding of an HMBS pathogenic variant on prenatal testing cannot be used to predict whether an individual will become symptomatic – or if they do become symptomatic, the age of onset, severity, or type of symptoms.
Diagnosis
Acute intermittent porphyria (AIP) is caused by a heterozygous HMBS pathogenic variant. AIP is considered overt in a heterozygote who was previously or is currently symptomatic and latent in a heterozygote who has never had symptoms, and typically has been diagnosed through cascade screening (i.e., molecular genetic testing for the familial HMBS pathogenic variant to identify family members who are heterozygous and, therefore, at increased risk for an acute attack). Individuals with latent AIP may be referred to as "carriers" in the medical literature (see Nomenclature).
Suggestive Findings in Probands with Overt AIP
Overt AIP should be suspected in individuals with the following clinical findings and family history.
Clinical findings of overt AIP
- Otherwise unexplained severe, acute abdominal pain without physical signs. The pain, which occasionally may be more severe in the back or thighs, usually requires opiate analgesia. Abdominal pain is present in the vast majority (92%) of acute attacks; atypical presentations are rare [Puy et al 2010, Gouya et al 2019]. Note: Clinically indistinguishable acute attacks occur in other acute porphyrias. See Differential Diagnosis.
- Nausea, vomiting, constipation, tachycardia, and hypertension are common.
- Muscle weakness, convulsions, mental changes, and hyponatremia are all features that may be present alone or in combination and that heighten the probability of acute porphyria [Puy et al 2010].
- The urine may be reddish-brown or red; however, this is not a constant finding, especially if the sample is fresh. The color is enhanced by exposure to air and light and reflects increased urinary concentrations of porphyrins and porphobilins formed from the porphyrin precursor porphobilinogen (PBG).
Family history. Consistent with autosomal dominant inheritance of an acute porphyria. Family history often reveals no other affected family members due to the low penetrance of clinical manifestations of AIP that result in a significant proportion of heterozygotes remaining asymptomatic (see Penetrance).
Establishing the Diagnosis
The diagnosis of overt AIP in a symptomatic proband is based on detection of increased concentration of PBG in urine on biochemical testing. Molecular genetic testing is not a first-line diagnostic test for probands; detection of a heterozygous HMBS pathogenic variant on molecular genetic testing is mainly used in difficult diagnostic situations – for example, where the proband is not available for testing.
Biochemical Testing
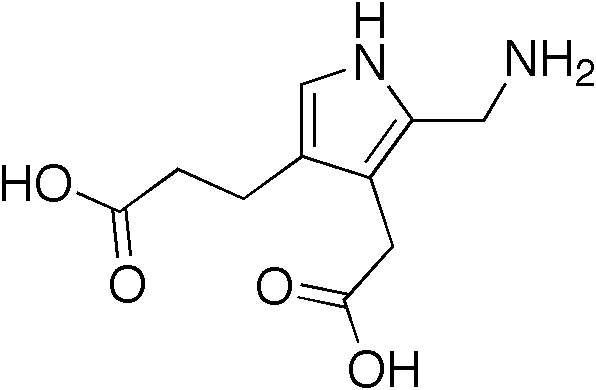
Urinary PBG. Evidence of an increased concentration of PBG in urine, using a specific quantitative assay, is essential to establish an unequivocal diagnosis of acute porphyria in a symptomatic individual. The concentration of PBG in urine is invariably increased in individuals with symptoms of AIP: during an acute attack, PBG concentration is often more than 10-20 times the upper reference limit [Elder et al 2013].
PBG is best analyzed in a fresh random 10-mL urine sample collected without preservative, and protected from prolonged exposure to bright light [Woolf et al 2017]. Urgent testing in new patients will typically require specific arrangements to be made with the biochemistry laboratory but results should be available within 24 hours of sample receipt.
Note that positive results on qualitative or semi-quantitative urine PBG tests must be confirmed by a specific quantitative measurement to avoid reporting of false positive test results.
Biochemical confirmation that the increased urinary PBG is caused by AIP requires evidence that:
- Total fecal porphyrin concentration or coproporphyrin isomer ratio is normal;
- Plasma porphyrin fluorescence emission scan either shows a peak around 620 nm or is normal.
Molecular Genetic Testing
Single-gene testing. Molecular genetic testing is not a first-line test for AIP because the relatively high prevalence of HMBS pathogenic variants in the general population (1:1299) and low penetrance (0.5%-1%) can lead to misdiagnosis and inappropriate treatment of individuals with nonspecific symptoms of abdominal pain [Chen et al 2019].
Following biochemical confirmation of increased urinary PBG, sequence analysis of HMBS is performed first to detect small intragenic deletions/insertions and missense, nonsense, and splice site variants. Note: Depending on the method used, exon or whole-gene deletions/duplications may not be detected. If no variant is detected by a sequencing method that is not able to detect exon or whole-gene deletions/duplications, the next step is to perform gene-targeted deletion/duplication analysis to detect intragenic deletions or duplications.
Table 1.
Molecular Genetic Testing Used in Acute Intermittent Porphyria
| Gene 1 | Method | Proportion of Probands with a Pathogenic Variant 2 Detectable by Method |
|---|---|---|
| HMBS | Sequence analysis 3 | 96%-98% 4 |
| Gene-targeted deletion/duplication analysis 5 | ~2% 4 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on allelic variants detected in this gene.
- 3.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 4.
In individuals with a proven biochemical diagnosis of AIP, Whatley et al [2009] reported that of 265 individuals, 255 had a variant detected by sequence analysis, five had a variant detected by gene-targeted deletion/duplication analysis, and five no variant was detected. Cerbino et al [2015] in a similar study reported that of 107 families, 105 had a variant detected by sequence analysis and two had a variant detected by gene-targeted deletion/duplication analysis.
- 5.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
Clinical Characteristics
Clinical Description
Acute intermittent porphyria (AIP), caused by a heterozygous HMBS pathogenic variant, is considered overt when a heterozygote was previously or is currently symptomatic and latent when a heterozygote has never had symptoms, and typically has been diagnosed through cascade screening (i.e., molecular genetic testing for the familial HMBS pathogenic variant to identify family members who are heterozygous and therefore at increased risk for an acute attack).
Overt AIP
Symptoms of AIP are more common in women than men and very rare before puberty. Onset typically occurs in the third or fourth decade [Elder et al 2013, Bonkovsky et al 2014].
The visceral, peripheral, autonomic, and/or central nervous systems may be affected, leading to a range of findings that are usually intermittent and sometimes life threatening. The course of acute attacks is highly variable within and between individuals.
Affected individuals may recover from acute AIP attacks within days, but recovery from severe attacks that are not promptly recognized and treated may take weeks or months. Although attacks in most individuals are typically caused by exposure to certain endogenous or exogenous factors, it is not uncommon for individuals to have acute attacks in which no precipitating factor can be identified.
Acute attack. Severe abdominal pain, which may be generalized or localized and not accompanied by muscle guarding, is the most common symptom and is often the initial sign of an acute attack. Back, buttock, or limb pain may be a feature. Gastrointestinal features including nausea, vomiting, constipation or diarrhea, abdominal distention, and ileus are also common. Tachycardia and hypertension are frequent, while fever, sweating, restlessness, and tremor are seen less frequently. Urinary retention, incontinence, and dysuria may be present.
Peripheral neuropathy is predominantly motor and is less common now than in the past. Muscle weakness often begins proximally in the legs but may involve the arms or legs distally and can progress to include respiratory muscles resulting in complete paralysis with respiratory failure. Bilateral axonal motor neuropathy may also involve the distal radial nerves. Motor neuropathy may also affect the cranial nerves or lead to bulbar paralysis.
Patchy sensory neuropathy may also occur
Mental changes are present in up to 30% of symptomatic individuals but are very rarely the dominant feature of AIP [Puy et al 2010]. Changes include insomnia, anxiety, depression, hallucinations, confusion, paranoia, amnesia, and/or altered consciousness ranging from somnolence to coma. These manifestations resolve after the attack, though anxiety may persist.
Seizures may occur in acute attacks, especially in individuals with hyponatremia, which may be worsened by vomiting and/or inappropriate fluid therapy. The cause of hyponatremia is not clear; both SIADH (syndrome of inappropriate antidiuretic hormone release) and renal salt wasting have been proposed as mechanisms.
Seizures may also be a manifestation of central nervous system involvement of the acute attack.
MRI findings. MRI changes were observed in two out of seven individuals with signs of CNS involvement. The main finding is posterior reversible encephalopathy syndrome [Pischik & Kauppinen 2009]. Twenty-two individuals with AIP presenting with posterior reversible encephalopathy syndrome were investigated with MRI imaging [Zheng et al 2018]; 95% of these presented with seizures that may be related to hyponatremia.
Cutaneous manifestations of porphyria do not occur in AIP.
Precipitating factors. Attacks of acute porphyria may be precipitated by endogenous or exogenous factors [Wang et al 2018]. These include:
- Prescribed and illicit drugs that are detoxified in the liver by cytochrome P450 and/or result in induction of 5-aminolevulinic acid (ALA) synthase and heme biosynthesis. Prescription drugs that can precipitate an attack include, for example, barbiturates, sulfa-containing antibiotics, some antiepileptic drugs, progestagens, and synthetic estrogens (see Agents/Circumstances to Avoid).
- Endocrine factors. Reproductive hormones play an important role in the clinical expression of AIP. In women, acute neurovisceral attacks related to the menstrual cycle, usually the luteal phase, are common [Wang et al 2018]. However, the majority of women with AIP fare well during pregnancy, despite substantial increases in the serum concentration of various steroid hormones [Marsden & Rees 2010].
- Fasting. A recognized precipitating factor is inadequate caloric intake [Wang et al 2018] in connection with, for example, dieting or heavy exercise schedules.
- Stress. Psychosocial and other stresses, including intercurrent illnesses, infections, alcoholic excess, and surgery, can precipitate an attack.
Chronic complications
- Hepatocellular carcinoma (HCC). Individuals with AIP, whether clinically manifest or latent, appear to be at increased risk of developing primary HCC [Innala & Andersson 2011], usually after age 54 years. The highest risk has been reported from Sweden; at present, it is unclear why the risk appears to be lower in other populations [Deybach & Puy 2011, Elder et al 2013]. The increased incidence of HCC appears to justify radiologic surveillance in individuals with AIP over age 50 years in order to allow early detection and improve outcomes [Peoc'h et al 2018].
- Renal involvement. Approximately 70% of individuals with recurrent attacks will develop progressive renal dysfunction as shown by declining estimated glomerular filtration rate (eGFR) (<90 mL/min/1.73m2). This may be a result of chronic renal exposure to high concentrations of ALA and porphobilinogen (PBG), influenced by genetic variation in the ALA transporter PEP2 [Tchernitchko et al 2017].
- Recurrent acute attacks. Approximately 3%-8% of individuals with AIP, mainly women, experience repeat attacks (defined as >3/yr in the EXPLORE study) for a prolonged period, often many years [Gouya et al 2019].
Mortality. Mortality directly related to acute attacks is now very rare in most countries as a result of improved treatment (use of human hemin; see Management, Treatment of Manifestations) and identification and counseling of presymptomatic relatives (see Management, Evaluation of Relatives at Risk). Deaths may occur as a complication of HCC or liver transplantation.
Latent AIP
Symptoms are present in only a minority of those heterozygous for an HMBS pathogenic variant that predisposes to AIP, and it may be difficult to be certain whether or not these are porphyria-related. The risk that an individual with latent AIP will later develop symptoms depends on age, sex, exposure to provoking agents, and other factors; however, the majority will remain asymptomatic throughout their lives.
Up to 50% of adults with latent AIP may have increased urinary PBG excretion.
Genotype-Phenotype Correlations
Genotype-phenotype correlations are not evident in AIP.
Penetrance
Families from the French reference center for porphyria were evaluated for penetrance of AIP. The cohort consisted of 496 symptomatic individuals and 1672 asymptomatic relatives with an HMBS pathogenic variant. The estimated penetrance of AIP in affected families was 22.9% and 12.7% in the relatives of AIP index cases.
Using Exome Variant Server data, a minimal prevalence of HMBS pathogenic variants in the general population was calculated as 1:1299. In France the prevalence of pathogenic variants in the general population was estimated at between 50-100,000 individuals and the prevalence 0.5%-1%. The authors propose that penetrance is a consequence of both environmental and genetic factors [Lenglet et al 2018].
Nomenclature
Individuals with latent AIP are often referred to as "carriers" in the medical literature. GeneReviews does not use the term "carrier" for an individual who is heterozygous for an autosomal dominant pathogenic variant – reserving the term "carriers" for those who are heterozygous for an autosomal recessive disorder, and thus are not expected to ever develop manifestations of the disorder.
Overt AIP may also be referred to as "manifest AIP."
Prevalence
In most countries, AIP is the most common of the acute hepatic porphyrias [Wang et al 2018].
- The prevalence of overt AIP in France is 1:132 000 inhabitants [Lenglet et al 2018]. This is similar to the incidence of newly diagnosed individuals in Europe, excluding Sweden, with overt AIP reported as 0.13:1,000,000 per year, with a calculated prevalence of 5.9:1,000,000 [Elder et al 2013].
- In Sweden the incidence and prevalence of AIP are about four times higher than in Europe due to a founder effect originating in Lappland [Floderus et al 2002] (see Table 3. Notable HMBS Pathogenic Variants).
Differential Diagnosis
Acute neurovisceral attacks. Clinically indistinguishable acute neurovisceral attacks occur in acute intermittent porphyria (AIP) and the three other acute porphyrias, and may complicate hereditary tyrosinemia type 1 (see Table 2) [Puy et al 2010].
Table 2.
Genes of Interest in the Differential Diagnosis of Clinically Manifest Acute Intermittent Porphyria (AIP)
| Gene | Disorder | MOI | Clinical Features | Biochemical Characteristics 1 | |||
|---|---|---|---|---|---|---|---|
| Urine | Stool | Plasma | Erythrocytes | ||||
| CPOX | Hereditary coproporphyria (HCP) | AD | Acute attack ± skin lesions 2 | ↑ PBG, ALA 3, porphyrins 4 | ↑ copro- porphyrin III | ↑ plasma porphyrins; fluorescence emission peak ~620 nm 5 | |
| PPOX | Variegate porphyria (VP) | AD | Acute attack ± skin lesions 2 | ↑ PBG, ALA 3, porphyrins 4 | ↑ proto- porphyrin 6 | ↑ plasma porphyrins; fluorescence emission peak ~626 nm 7 | |
| ALAD | ALAD deficiency porphyria (OMIM 612740) | AR | Acute attack | ↑ ALA, copropor- phyrin III, normal PBG | ↑ zinc-protoporphyrin; ↓ ALAD activity | ||
| FAH | Tyrosinemia type 1 | AR | Acute attack | ↑ ALA | ↓ ALAD activity | ||
AD = autosomal dominant; ALA = 5-aminolevulinic acid; ALAD = 5-aminolevulinate dehydratase; AR = autosomal recessive; MOI = mode of inheritance
- 1.
See Table 1 for biochemical characteristics of clinically manifest AIP.
- 2.
Acute neurovisceral attacks are accompanied by porphyric skin lesions (bullae, fragile skin) in about 15% of persons with HCP and about 60% of persons with VP.
- 3.
PBG increased more than ALA; both may decrease rapidly as symptoms resolve.
- 4.
Uroporphyrin from in vitro polymerization of PBG and coproporphyrin; measurement is not required for diagnosis and may mislead.
- 5.
Plasma porphyrin concentration may occasionally be normal; fluorescence emission spectroscopy does not distinguish between HCP and AIP.
- 6.
Protoporphyrin is the main stool porphyrin, but a small increase in coproporphyrin III is also observed
- 7.
Plasma porphyrin concentration is always increased and fluorescence emission spectroscopy distinguishes VP from all other porphyrias.
Lead poisoning may also mimic the symptoms (i.e., abdominal pain) of clinically manifest acute AIP and disturb heme biosynthesis; however, anemia, a feature of lead poisoning, is not a feature of AIP. Lead poisoning is characterized in urine by increased 5-aminolevulinic acid (ALA), coproporphyrin III, normal porphobilinogen and in erythrocytes, increased zinc-protoporphyrin and decreased 5-aminolevulinate dehydratase (ALAD) activity.
Red discoloration of the urine. Hematuria, ingestion of beetroot, some drugs and food additives, and porphyrin excretion in other porphyrias (e.g., porphyria cutanea tarda, congenital erythropoietic porphyria) may produce similar red discoloration of the urine.
Note: For a general review of the genetic porphyrias, see Hereditary Coproporphyria, Differential Diagnosis.
Management
Evaluations Following Initial Diagnosis of Latent AIP and Asymptomatic Individuals with a History of Overt AIP
To establish the extent of disease and needs in an individual diagnosed with acute intermittent porphyria, the following evaluations (if not performed as part of the evaluation that led to the diagnosis) are recommended:
- Full clinical history and examination, including neurologic evaluation
- Review of medications to assess risk versus benefit (see Agents/Circumstances to Avoid)
- Quantitation of urine porphobilinogen (PBG) excretion to establish a baseline for comparison with future measurements taken during symptoms suggestive of active porphyria
- Patients should be advised to register with an organization that provides warning jewelry in case of an accident (e.g., MedicAlert® or similar).
- Referral to a porphyria specialist for more detailed clinical advice on AIP (see Resources)
- Patients should be advised about support from national patient associations where available. Good-quality information is now widely available from patient or professional organizations either in paper form or from the Internet; see Resources.
- Consultation with a clinical geneticist and/or genetic counselor
Treatment of Manifestations of Overt AIP
Acute Neurovisceral Attack
Immediate treatment of an acute neurovisceral attack does not require confirmation of the specific type of acute porphyria.
Clinical assessment should include a full neurologic evaluation.
In persons known to have AIP consider other causes of abdominal pain in addition to porphyria.
Investigations should include the following:
- Full blood count
- Measurement of serum/plasma concentrations of urea, creatinine, and electrolytes
- Serum and urine osmolality if hyponatremic
- Urine sodium concentration if hyponatremic
- Other blood tests as indicated by the patient's condition and possible cause of the attack (e.g., CRP, blood cultures, CK, magnesium)
MRI should be considered if CNS symptoms are present.
General measures
- Review all medications and discontinue any that can exacerbate acute porphyria [Stein et al 2017]. See Agents/Circumstances to Avoid.
- Restore energy balance using an enteral route if possible. When required, intravenous fluid should contain a minimum of 5% dextrose; however, hypotonic dextrose-water solutions should be avoided because of the risk of hyponatremia.
- Treat intercurrent infections and other diseases promptly.
Supportive treatment
- Pain relief. Effective analgesia should be provided as soon as possible, usually in the form of parenteral opiates (morphine, diamorphine, and fentanyl are safe). Very large quantities may be required in a severe acute attack. Consider patient-controlled analgesia and support from a pain team.
- Nausea and vomiting. Prochloperazine, promazine, or ondansetron are considered safe.
- Hypertension. Beta blockers are considered safe. Note: End-stage renal disease, which is thought to result from chronic systemic arterial hypertension, may be delayed through effective blood pressure control [Stewart 2012].
- Convulsions can be terminated with intravenous diazepam, clonazepam, or magnesium sulphate.
- Fluid balance and electrolytes. Intravenous fluid replacement may be required to correct dehydration or electrolyte imbalance. Dextrose in water solutions should be avoided because of the risk of hyponatremia. Chronic hyponatremia (developing over >48 hours) should be corrected slowly to minimize the risk of central pontine myelinolysis [Stein et al 2017].
Specific treatment
- For mild acute neurovisceral attacks, a high carbohydrate intake, preferably oral and together with other supportive measures (see Acute Neurovisceral Attack), may be used for up to 48 hours. If improvement is unsatisfactory or if additional and progressive neurologic features present, intravenous administration of hemin preparations is recommended.
- Intravenous human hemin is the most effective treatment for acute neurovisceral attacks. Intravenous administration of hemin preparations may be life saving if employed early, when neuronal damage is still reversible, and may help to avoid paresis or prevent its progression.
- The recommended dose for hemin is 3-4 mg/kg IV, given once daily for four days. Treatment may be extended, depending on the clinical course. Note: Because 100 mg of hemin contains 8 mg of iron, frequent administration of hemin may increase the risk for iron overload. Periodic monitoring of serum ferritin concentration and/or transferrin saturation is therefore appropriate in individuals treated repeatedly with hemin.
- Panhematin™ (Ovation Pharmaceuticals, Inc) is approved for treatment of acute attacks in the US. This product is supplied as a dried powder, which must be reconstituted with sterile water immediately before intravenous injection and administered over 10-15 minutes. Because the administration of Panhematin™ reconstituted with sterile water is associated with transient, mild coagulopathy, concurrent anticoagulant therapy should be avoided.
- Heme arginate (Normosang Recordati Rare Diseases, Paris) is an arginine-stabilized form of human hemin available nearly worldwide, including in Europe, Africa, the Middle East, and South America. It is infused over at least 30 minutes. It has the same advantage as hemin in treating an acute neurovisceral attack, but has fewer reported side effects [Puy et al 2010].
Note: (1) Phlebitis after intravenous injection can be minimized by reconstituting hematin in 20% human serum albumin solution and/or by using a large vein or a central catheter for infusion. Peripheral cannulas used to administer hematin should be replaced after each use. (2) An infusion set with an in-line filter is recommended to remove any undissolved particulate matter. (3) Rigorous flushing of venous catheters with boluses of saline totaling 100 mL is recommended.
Advice on safe treatment of persons with porphyria in some specific clinical situations (e.g., epilepsy, HIV, malaria, tuberculosis, hyperlipidemia, and hypertension) is available on the Porphyria South Africa website.
Recurrent Acute Attacks
Recurrent acute attacks are best managed with support and advice from a porphyria specialist. See information and contact details of specialist porphyria centers at the European Porphyria Network website.
Medical therapy aims to reduce the frequency and or severity of acute attacks by the following measures:
- Ovulation suppression with gonadorelin analogs for patients with recurrent menstrual cycle-related acute neurovisceral attacks [Schulenburg-Brand et al 2017]. Long-acting analogs can be used to prevent ovulation and should be administered during the first few days of the menstrual cycle to minimize the early stimulation effect on hormone release which can trigger an attack. Side effects can be minimized by administering estrogen, preferably by patch. Gynecologic review and bone density monitoring are recommended.
- Prophylactic hemin infusion. The minimum effective infusion frequency should be employed, usually a weekly dose of hemin infused via an indwelling venous catheter. Problems include those associated with a venous access device (infection, blockage) and iron overload (see Prevention of Primary Manifestations).
- Givosiran (ALN-AS1), an interference RNA that represses ALAS1, has completed Phase I and III clinical trials and was approved by the US Food and Drug Administration (FDA) in November 2019. The trial showed a reduction of ALA and PBG excretion to near normal levels and a reduction in the rate of porphyria attacks when compared to a placebo. Adverse events included elevated liver enzymes and chronic kidney disease [Sardh et al 2019].
Other Treatments
Liver transplantation is curative and reported from several centers [Wahlin et al 2010]. Indications include repeated life-threatening acute attacks, failure of medical therapy, and poor quality of life.
Combined liver and kidney transplantation, which has been successful, can be considered in those with AIP with repeated severe attacks and renal failure [Wahlin et al 2010]. Patients with AIP may require dialysis or renal transplantation [Wang et al 2018].
Prevention of Primary Manifestations for all Individuals with AIP
To prevent acute attacks patients are advised on the potential triggers as follows:
- Assure that adequate nutrition is provided by a normal balanced diet. Avoid unsupervised calorie restriction diets, particularly those that exclude carbohydrate completely.
- Avoid drugs and chemicals known to exacerbate porphyria, particularly prescribed medication and over-the-counter medication. See Agents/Circumstances to Avoid.
- Seek timely treatment of systemic illness or infection.
- Avoid excessive alcohol consumption and smoking.
Surveillance
Individuals with Overt AIP
Annual hepatic imaging for HCC in individuals older than age 50 years has been shown to improve survival [Innala & Andersson 2011]. The incidence of HCC in this group of patients with AIP is 0.6% and it has been recommended in Europe that imaging should probably be biannual to bring it in line with other liver diseases that infer an increased risk for HCC [Peoc'h et al 2018].
Note: (1) Serum α-fetoprotein measurement is not helpful. (2) Protein induced by Vitamin K absence (PIVKA-II) may be useful as a biomarker [Peoc'h et al 2018].
Individuals with Latent AIP
Peoc'h et al [2018] reviewed five published studies that reported 77 individuals with acute hepatic porphyria (AHP) diagnosed with primary liver cancer. The proportion of patients with latent AHP varied between 0 and 43%.
Agents/Circumstances to Avoid for All Individuals with AIP
Excessive alcohol consumption and smoking should be avoided.
Knowledge about the safety of many drugs and other over-the-counter preparations in acute porphyrias is incomplete; however, evidence-based guidelines for assessment of drug porphyrogenicity have been published [Hift et al 2011].
- Searchable drug safety databases are available at the following websites:
- The Drug Database for Acute Porphyria
- The American Porphyria Foundation
- Information on prescribing in certain conditions (e.g. HIV, epilepsy, malaria): Porphyria South Africa
- Safe drug lists are available at the following website: Welsh Medicines Information Centre - Porphyria Information Service
- Unsafe drug lists are available at the following website: British National Formulary (subscription required)
Evaluation of Relatives at Risk for All Individuals with AIP
It is appropriate to clarify the genetic status of apparently asymptomatic at-risk relatives of an individual with either overt or latent AIP so that those who are heterozygous for an HMBS pathogenic variant (and thus at increased risk of developing acute attacks of AIP) can be identified early and counseled about preventive measures and surveillance (see Prevention of Primary Manifestations, Agents/Circumstances to Avoid, and Surveillance).
- When the HMBS pathogenic variant has been identified in the family, molecular genetic testing is the method of choice for identification of individuals heterozygous for an HMBS pathogenic variant who are thus at risk for an acute attack.
- Measurement of erythrocyte HMBS activity is less sensitive but may be useful for the few families in which an HMBS pathogenic variant cannot be identified or when molecular testing is unavailable.
- Urinary porphobilinogen (PBG) excretion should not be used as it is normal in all prepubertal children with latent AIP and in at least 50% of adults.
Note: Although acute attacks are rare before puberty, children in families with AIP should be offered testing with appropriate consent from parents or guardians in order to provide advice/education on avoidance of precipitating factors and ensure rapid