Craniosynostosis 4
A number sign (#) is used with this entry because of evidence that craniosynostosis-4 (CRS4) is caused by heterozygous mutation in the ERF gene (611888) on chromosome 19q13.
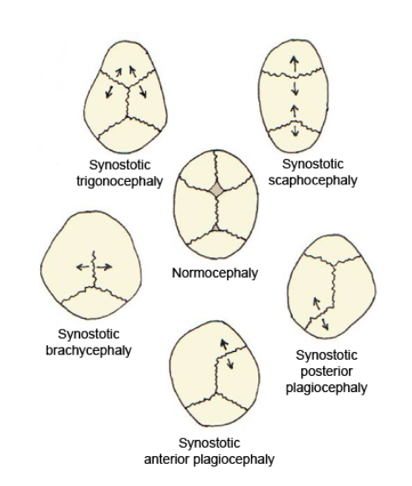
DescriptionCraniosynostosis is a primary abnormality of skull growth involving premature fusion of the cranial sutures such that the growth velocity of the skull often cannot match that of the developing brain. This produces skull deformity and, in some cases, raises intracranial pressure, which must be treated promptly to avoid permanent neurodevelopmental disability (summary by Fitzpatrick, 2013). Craniosynostosis-4 includes lambdoid, sagittal, metopic, coronal, and multisuture forms.
For a discussion of genetic heterogeneity of craniosynostosis, see CRS1 (123100).
Clinical FeaturesFryburg et al. (1995) reported 2 families in which multiple members had proven or suspected lambdoid craniosynostosis. The synostosis resulted in occipital flattening. In the first family, a brother and sister were affected and a maternal great-grandmother was reported to have had a flat occiput similar to the patient's. Posterior plagiocephaly was noted at a 4-month checkup in the proposita, who underwent corrective cranioplasty at age 8 months. Her brother, 4 years older, had likewise undergone cranioplasty at age 8 months for posterior plagiocephaly thought to be due to lambdoid suture craniosynostosis. Another brother had a normal skull shape. In the second family, the propositus had unilateral (right-sided) occipital flattening with ipsilateral frontal bossing. Twin sisters were affected likewise, 1 having frontal bossing and occipital skull flattening and the other having right occipital skull flattening accompanied by ipsilateral frontal bossing. Their father had a normal skull but his brother had documented posterior skull flattening and the paternal great-grandmother of the propositus was reported to have plagiocephaly. In most of these cases, the lambdoid synostosis was what McComb (1991) referred to as 'functional' lambdoid synostosis because the flattening of the posterior skull was not due to postural molding and was not associated with true craniosynostosis.
Rieubland et al. (2011) reported an infant, born of unrelated parents by cesarean section, with bilateral lambdoid synostosis resulting in pseudoencephalocele through the posterior fontanel. In addition, the infant had prominent scalp veins, unusual hair whorl, hypertelorism, telecanthus, short nose with anteverted nostrils, small and low-set ears, microretrognathia, and small hands and feet with horizontal nail ridges. Growth, development, hearing, and vision were all normal. Screening of targeted exons in known craniosynostosis genes did not reveal any pathogenic mutations. The pattern of abnormalities suggested a genetic etiology, but the mode of inheritance could not be determined; there was no family history of a similar disorder. Rieubland et al. (2011) concluded that the patient represented a previously undescribed craniosynostosis syndrome.
Twigg et al. (2013) studied 26 mutation-positive individuals from 12 families with craniosynostosis associated with heterozygous mutation in the ERF gene (see MOLECULAR GENETICS). Of 14 pediatric cases, 13 had craniosynostosis; 1 boy who carried a mutation exhibited only hypertelorism and exorbitism, whereas his sister had pansynostosis. In the 8 children who underwent 3D CT scan of the skull, fusion was observed to have affected the sagittal suture in 7 cases, the lambdoid suture in 5 cases, the coronal suture in 3 cases, and the metopic suture in 1 case. Seven of 12 probands had syndromic multiple suture synostosis, 2 had only sagittal synostosis, 1 had only lambdoid synostosis, and in 1 proband the sutures were not specified. In half of the families, a diagnosis of Crouzon syndrome (123500) had been suggested because of exorbitism and midface hypoplasia, but FGFR2 (176943) testing was normal. Increased intracranial pressure was documented in 9 cases, and Chiari type I malformations were diagnosed in 4 patients. Twelve (86%) of 14 pediatric patients had behavioral or learning problems, particularly affecting concentration and language acquisition. Despite multisuture involvement, many affected individuals presented after infancy, and primary surgery was frequently delayed. Extracranial growth was normal, except for occasional mild shortening of the digits; no health problems of later onset were consistently found in carrier adults, in many of whom the only clinical feature was macrocephaly or mild craniofacial signs. Three-dimensional scanning of 14 mutation-positive individuals from 6 families showed that hypertelorism, shortening and/or vertical displacement of the nose, and prominent orbits and forehead were consistently present but varied in severity.
Chaudhry et al. (2015) studied 2 unrelated boys with craniosynostosis, and mutation in the ERF gene. The first patient presented at 6.5 years of age with involvement of all sutures, whereas the second presented at 3 months of age with bicoronal and metopic involvement. Both exhibited dysmorphic features, including proptosis, hypertelorism, depressed nasal bridge, and retrognathia. Additional features in the first patient included malar hypoplasia as well as ectopic posterior pituitary, Chiari I malformation, and hypoplastic optic nerves with dilated cerebrospinal fluid sheaths. The second patient, who underwent frontoorbital remodeling at age 10 months, showed speech delay at age 19 months.
Molecular GeneticsIn a family in which 1 brother had synostosis of all cranial sutures, another brother had metopic, sagittal, and left coronal synostosis, and their mother had exorbitism and midface hypoplasia but no documented craniosynostosis, Twigg et al. (2013) performed exome sequencing and identified a heterozygous nonsense mutation in the ERF gene (R183X; 611888.0001) that segregated with disease. Sequencing of ERF in 411 samples from unrelated individuals with craniosynostosis identified 8 heterozygous mutations in 11 additional families with synostosis of variable sutures (see, e.g., 611888.0002-611888.0005). No genotype-phenotype correlation was found.
Chaudhry et al. (2015) analyzed the ERF gene in 40 patients with genetically undiagnosed multiple suture or sagittal synostosis, and identified 2 heterozygous mutations, one in the start codon (611888.0006 and the other in a splice site 611888.0007), in 2 affected boys. Chaudhry et al. (2015) noted that 2 (5%) of 40 patients in their study population had a pathogenic variant in the ERF gene, similar to the 3% frequency that was observed in a larger cohort (Twigg et al., 2013).