Gerstmann–sträussler–scheinker Syndrome
Gerstmann–Sträussler–Scheinker syndrome (GSS) is an extremely rare, usually familial, fatal neurodegenerative disease that affects patients from 20 to 60 years in age. It is exclusively heritable, and is found in only a few families all over the world (according to NINDS). It is, however, classified with the transmissible spongiform encephalopathies (TSE) due to the causative role played by PRNP, the human prion protein. GSS was first reported by the Austrian physicians Josef Gerstmann, Ernst Sträussler and Ilya Scheinker in 1936.
Familial cases are associated with autosomal-dominant inheritance.
Certain symptoms are common to GSS, such as progressive ataxia, pyramidal signs, and even adult-onset dementia; they progress more as the disease progresses.
Symptoms
Symptoms start with slowly developing dysarthria (difficulty speaking) and cerebellar truncal ataxia (unsteadiness) and then the progressive dementia becomes more evident. Loss of memory can be the first symptom of GSS. Extrapyramidal and pyramidal symptoms and signs may occur and the disease may mimic spinocerebellar ataxias in the beginning stages. Myoclonus (spasmodic muscle contraction) is less frequently seen than in Creutzfeldt–Jakob disease. Many patients also exhibit nystagmus (involuntary movement of the eyes), visual disturbances, and even blindness or deafness. The neuropathological findings of GSS include widespread deposition of amyloid plaques composed of abnormally folded prion protein.
Four clinical phenotypes are recognised: typical GSS, GSS with areflexia and paresthesia, pure dementia GSS and Creutzfeldt-Jakob disease-like GSS.
Causes
GSS is one of a small number of diseases that are caused by prions, a class of pathogenic proteins highly resistant to proteases.
A change in codon 102 from proline to leucine has been found in the prion protein gene (PRNP, on chromosome 20) of most affected individuals. Therefore, it appears this genetic change is usually required for the development of the disease.
Diagnosis
GSS can be identified through genetic testing. Testing for GSS involves a blood and DNA examination in order to attempt to detect the mutated gene at certain codons. If the genetic mutation is present, the patient will eventually be afflicted by GSS, and, due to the genetic nature of the disease, the offspring of the patient are predisposed to a higher risk of inheriting the mutation.
Treatment
There is no cure for GSS, nor is there any known treatment to slow the progression of the disease. However, therapies and medication are aimed at treating or slowing down the effects of the symptoms. Their goal is to try to improve the patient's quality of life as much as possible. The only treatment, which appears to be able to stop the disease, is being tested at the Medical Research Center in London. It is the monoclonal antibody PRN100.
Prognosis
Duration of illness can range from three months to 13 years with an average duration of five or six years.
Research
GSS is very rare, making its history hard to track exactly where it descended from. In 1989, the first mutation of the prion protein gene was identified in a GSS family (Elsevier Science, 2002). Prion diseases (transmissible spongiform encephalopathies) are degenerative diseases of the brain thought to be caused by a protein that converts to an abnormal form called a prion (Gambetti Pierluigi, 2013). GSS was later realized to have many different gene mutation types, with some showing different symptoms first or having other symptoms worse than others. Doctors in different parts of the world are uncovering more generations and families that have the mutation. It is hard to discover GSS for two main reasons: (1) the disease has been reported in only a few countries; and (2) the disease may be underreported due to its clinical similarity to other diseases (Ghetti B, et al., 2003). The Indiana Kindred is the largest, spanning over 8 generations, and includes over 3,000 people with 57 individuals known to be affected (B. Ghetti, et al., 1996).
Notes
- ^ Liberski, Paweł P. (2012). "Gerstmann–Sträussler–Scheinker Disease". Advances in Experimental Medicine and Biology. 724: 128–137. doi:10.1007/978-1-4614-0653-2_10. ISSN 0065-2598. PMID 22411239.
- ^ synd/2269 at Who Named It?
- ^ Gerstmann, J.; Sträussler, E.; Scheinker, I. (1936). "Über eine eigenartige hereditär-familiäre Erkrankung des Zentralnervensystems. Zugleich ein Beitrag zur Frage des vorzeitigen lokalen Alterns". Zeitschrift für die gesamte Neurologie und Psychiatrie. 154: 736–762. doi:10.1007/bf02865827.
- ^ De Michele G, Pocchiari M, Petraroli R, et al. (August 2003). "Variable phenotype in a P102L Gerstmann–Sträussler–Scheinker Italian family". Can J Neurol Sci. 30 (3): 233–6. doi:10.1017/S0317167100002651. PMID 12945948. Archived from the original on 2013-01-28.
- ^ Farlow, M.R.; et al. (1989). "Gerstmann-Sträussler-Scheinker disease. 1. Extending the clinical spectrum". Neurology. 39 (11): 1446–1452. doi:10.1212/wnl.39.11.1446. PMID 2812321.
- ^ a b c Collins S, McLean CA, Masters CL (September 2001). "Gerstmann–Sträussler–Scheinker syndrome, fatal familial insomnia, and kuru: a review of these less common human transmissible spongiform encephalopathies". J Clin Neurosci. 8 (5): 387–97. doi:10.1054/jocn.2001.0919. PMID 11535002.
- ^ a b Gambetti, Pierluigi. "Gerstmann–Sträussler–Scheinker Disease". The Merck Manuals: Online Medical Library. Archived from the original on February 22, 2011. Retrieved April 6, 2011.
- ^ Tesar A, Matej R, Kukal J, Johanidesova S, Rektorova I, Vyhnalek M, Keller J, Eliasova I, Parobkova E, Smetakova M, Musova Z, Rusina R (2019) Clinical variability in P102L Gerstmann-Sträussler-Scheinker Syndrome. Ann Neurol
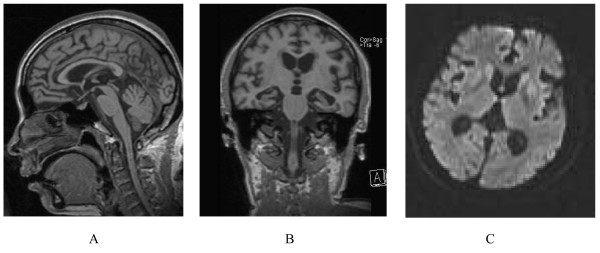
- ^ Arata H, Takashima H, Hirano R, et al. (June 2006). "Early clinical signs and imaging findings in Gerstmann–Sträussler–Scheinker syndrome (Pro102Leu)". Neurology. 66 (11): 1672–8. doi:10.1212/01.wnl.0000218211.85675.18. PMID 16769939.
- ^ "PRION DISEASES AND PRN100"
External links
- Gerstmann–Sträussler–Scheinker syndrome, MedicineNet.com