Encephalitis
Overview
Encephalitis (en-sef-uh-LIE-tis) is inflammation of the brain. There are several causes, including viral infection, autoimmune inflammation, bacterial infection, insect bites and others. When inflammation is caused by an infection in the brain, it's known as infectious encephalitis. And when it's caused by your own immune system attacking the brain, it's known as autoimmune encephalitis. Sometimes there is no known cause.
In some cases, encephalitis can be life-threatening. Prompt diagnosis and treatment are important because it's difficult to predict how encephalitis will affect each individual.
Symptoms
Encephalitis may cause many different symptoms including confusion, personality changes, seizures or problems with movement. Encephalitis also may cause changes in sight or hearing.
Most people with infectious encephalitis have flu-like symptoms, such as:
- Headache.
- Fever.
- Aches in muscles or joints.
- Fatigue or weakness.
Typically, these are followed by more-severe symptoms over a period of hours to days, such as:
- Stiff neck.
- Confusion, agitation or hallucinations.
- Seizures.
- Loss of sensation or being unable to move certain areas of the face or body.
- Irregular movements.
- Muscle weakness.
- Problems with speech or hearing.
- Loss of consciousness, including coma.
In infants and young children, signs and symptoms also might include:
- Bulging in the soft spots of an infant's skull, known as fontanels.
- Nausea and vomiting.
- Stiffness affecting the whole body.
- Poor feeding or not waking for a feeding.
- Irritability.
In cases of autoimmune encephalitis, symptoms may develop more slowly over several weeks. Flu-like symptoms are less common, but can sometimes happen weeks before more-severe symptoms start. Symptoms are different for everyone, but it's common for people to have a combination of symptoms including:
- Changes in personality.
- Memory loss.
- Problems understanding what is real and what is not, known as psychosis.
- Seeing or hearing things that aren't there. These are called hallucinations.
- Seizures.
- Changes in vision.
- Sleep problems.
- Muscle weakness.
- Loss of sensation.
- Problems walking.
- Abnormal movements.
- Bladder and bowel problems.
When to see a doctor
Get immediate care if you are experiencing any of the more-severe symptoms associated with encephalitis. A severe headache, fever and change in consciousness require urgent care.
Infants and young children with any signs or symptoms of encephalitis should receive urgent care.
Causes
In approximately half of patients, the exact cause of encephalitis is not known.
In those for whom a cause is identified, there are two main types of encephalitis:
- Infectious encephalitis. This condition occurs when a virus or other agent directly infects the brain. The infection may affect one area or be widespread. Viruses are the most common causes of infectious encephalitis, including some that can be passed by mosquitoes or ticks. Very rarely, encephalitis may be caused by bacteria, fungus or parasites.
- Autoimmune encephalitis. This condition occurs when your own immune cells mistakenly attack the brain or make antibodies targeting proteins and receptors in the brain. The exact reason why this happens is not completely understood. Sometimes the abnormal immune response can be triggered by benign or cancerous tumors, known as paraneoplastic and autoimmune encephalitis. Other types of autoimmune encephalitis such as acute disseminated encephalomyelitis (ADEM) can be triggered by infection in your body. This is known as post-infectious autoimmune encephalitis. In many instances, no definitive trigger for the abnormal immune response is identified.
Common viral causes
The viruses that can cause encephalitis include:
- Herpes simplex virus (HSV). Both HSV type 1 — associated with cold sores and fever blisters around your mouth — and HSV type 2 — associated with genital herpes — can cause encephalitis. Encephalitis caused by HSV type 1 is rare but can result in significant brain damage or death.
- Other herpes viruses. These include the Epstein-Barr virus, which commonly causes infectious mononucleosis, and the varicella-zoster virus, which commonly causes chickenpox and shingles.
- Enteroviruses. These viruses include the poliovirus and the coxsackievirus, which usually cause an illness with flu-like symptoms, eye inflammation and abdominal pain.
- Mosquito-borne viruses. These viruses can cause infections such as West Nile, La Crosse, St. Louis, western equine and eastern equine encephalitis. Symptoms of an infection might appear within a few days to a couple of weeks after exposure to a mosquito-borne virus.
- Tick-borne viruses. The Powassan virus is carried by ticks and causes encephalitis in the Midwestern United States. Symptoms usually appear about a week after a bite from an infected tick.
- Rabies virus. Infection with the rabies virus, which is usually transmitted by a bite from an infected animal, causes a rapid progression to encephalitis once symptoms begin. Rabies is a rare cause of encephalitis in the United States.
Risk factors
Anyone can develop encephalitis. Factors that may increase the risk include:
- Age. Some types of encephalitis are more common or more-severe in certain age groups. In general, young children and older adults are at greater risk of most types of viral encephalitis. Similarly, some forms of autoimmune encephalitis are more common in children and young adults, whereas others are more common in older adults.
- Weakened immune system. People who have HIV/AIDS, take immune-suppressing medicines or have another condition causing a weakened immune system are at increased risk of encephalitis.
- Geographical regions. Mosquito- or tick-borne viruses are common in particular geographical regions.
- Season of the year. Mosquito- and tick-borne diseases tend to be more common in summer in many areas of the United States.
- Autoimmune disease. People who already have an autoimmune condition may be more prone to develop autoimmune encephalitis.
- Smoking. Smoking increases the chances of developing lung cancer, which in turn increases the risk of developing paraneoplastic autoimmune encephalitis.
Complications
The complications of encephalitis vary, depending on factors such as:
- Your age.
- The cause of your infection.
- The severity of your initial illness.
- The time from disease onset to treatment.
People with relatively mild illness usually recover within a few weeks with no long-term complications.
Complications of severe illness
Inflammation can injure the brain, possibly resulting in a coma or death.
Other complications may last for months or be permanent. These complications can vary widely in severity and can include:
- Persistent fatigue.
- Weakness or lack of muscle coordination.
- Personality changes.
- Memory problems.
- Hearing or vision defects.
- Speech impairments.
Prevention
The best way to prevent viral encephalitis is to take precautions to avoid exposure to viruses that can cause the disease. Try to:
- Practice good hygiene. Wash hands frequently and thoroughly with soap and water, particularly after using the toilet and before and after meals.
- Don't share utensils. Don't share tableware and beverages.
- Teach your children good habits. Make sure they practice good hygiene and avoid sharing utensils at home and school.
- Get vaccinations. Keep your own and your children's vaccinations current. Before traveling, talk to your health care provider about recommended vaccinations for different destinations.
Protection against mosquitoes and ticks
To minimize your exposure to mosquitoes and ticks:
- Dress to protect yourself. Wear long-sleeved shirts and long pants if you're outside between dusk and dawn when mosquitoes are most active, and when you're in a wooded area with tall grasses and shrubs where ticks are more common.
- Apply mosquito repellent. Chemicals such as DEET can be applied to both the skin and clothes. To apply repellent to your face, spray it on your hands and then wipe it on your face. If you're using both sunscreen and a repellent, apply sunscreen first.
- Use insecticide. The Environmental Protection Agency recommends the use of products containing permethrin, which repels and kills ticks and mosquitoes. These products can be sprayed on clothing, tents and other outdoor gear. Permethrin shouldn't be applied to the skin.
- Avoid mosquitoes. Refrain from unnecessary activity in places where mosquitoes are most common. If possible, avoid being outdoors from dusk till dawn, when mosquitoes are most active. Repair broken windows and screens.
- Get rid of water sources outside your home. Eliminate standing water in your yard, where mosquitoes can lay their eggs. Common problems include flowerpots or other gardening containers, flat roofs, old tires, and clogged gutters.
- Look for outdoor signs of viral disease. If you notice sick or dying birds or animals, report your observations to your local health department.
Protection for young children
Insect repellents aren't recommended for use on infants younger than 2 months of age. Instead, cover an infant carrier or stroller with mosquito netting.
For older infants and children, repellents with 10% to 30% DEET are considered safe. Products containing both DEET and sunscreen aren't recommended for children because reapplication — which might be necessary for the sunscreen component — will expose the child to too much DEET.
Tips for using mosquito repellent with children include:
- Always assist children with the use of mosquito repellent.
- Spray on clothing and exposed skin.
- Apply the repellent when outdoors to lessen the risk of inhaling the repellent.
- Spray repellent on your hands and then apply it to your child's face. Take care around the eyes and ears.
- Don't use repellent on the hands of young children who may put their hands in their mouths.
- Wash treated skin with soap and water when you come indoors.
Diagnosis
Your health care provider will start with a thorough physical examination and medical history.
Your provider might then recommend:
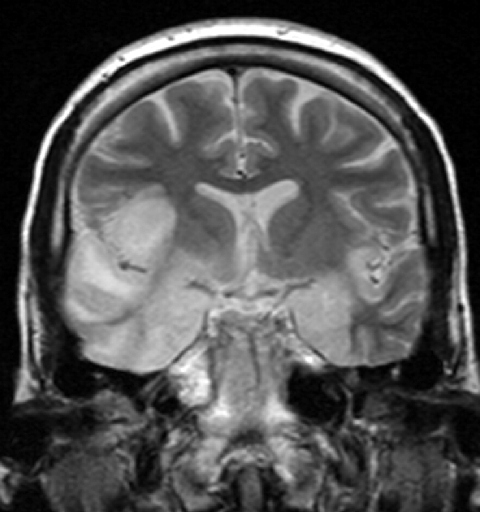
- Brain imaging. MRI or CT images can reveal any swelling of the brain or another condition that might be causing your symptoms, such as a tumor.
- Spinal tap, known as a lumbar puncture. A needle inserted into your lower back removes a small amount of cerebrospinal fluid (CSF), the protective fluid that surrounds the brain and spinal column. Changes in this fluid can point to infection and inflammation in the brain. Sometimes samples of CSF can be tested to identify the cause. This may include testing for infection or presence of antibodies associated with autoimmune encephalitis.
- Other lab tests. Samples of blood, urine or excretions from the back of the throat can be tested for viruses or other infectious agents.
- Electroencephalogram (EEG). Electrodes affixed to your scalp record the brain's electrical activity. Certain abnormal patterns may indicate a diagnosis of encephalitis.
- Body imaging. Sometimes, autoimmune encephalitis may be triggered by an abnormal immune response to a tumor, benign or cancerous, in your body. Your health care provider may order imaging studies, such as ultrasound, MRI, CT or CT-PET scans. These scans may look at your chest, abdomen or pelvis to check for these tumors. If a mass is found, a small piece of it may be removed to study it in a lab. This is known as a biopsy.
- Brain biopsy. Rarely, a small sample of brain tissue might be removed for testing. A brain biopsy is usually done only if symptoms are worsening and treatments are having no effect.
Treatment
Treatment for mild encephalitis usually consists of:
- Bed rest.
- Plenty of fluids.
- Anti-inflammatory medicines — such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) — to relieve headaches and fevers.
Antiviral medicines
Encephalitis caused by certain viruses usually requires antiviral treatment.
Antiviral medicines commonly used to treat encephalitis include:
- Acyclovir (Zovirax).
- Ganciclovir (Zirgan).
- Foscarnet (Foscavir).
Some viruses, such as insect-borne viruses, don't respond to these treatments. But because the specific virus may not be identified immediately or at all, health care providers often recommend immediate treatment with acyclovir. Acyclovir can be effective against HSV, which can result in significant complications when not treated promptly.
Antiviral medicines are generally well tolerated. Rarely, side effects can include kidney damage.
Autoimmune encephalitis
If the tests show an autoimmune cause of encephalitis, then medicines that target your immune system, known as immunomodulatory medicines, or other treatments may be started. These may include:
- Intravenous or oral corticosteroids.
- Intravenous immunoglobulin.
- Plasma exchange.
Some people with autoimmune encephalitis need long-term treatment with immunosuppressive medicines. These may include azathioprine (Imuran, Azasan), mycophenolate mofetil (CellCept), rituximab (Rituxan) or tocilizumab (Actemra).
Autoimmune encephalitis caused by tumors may require treatment of those tumors. This may include surgery, radiation, chemotherapy or a combination of treatments.
Supportive care
People who are hospitalized with severe encephalitis might need:
- Breathing assistance, as well as careful monitoring of breathing and heart function.
- Intravenous fluids to ensure proper hydration and levels of essential minerals.
- Anti-inflammatory medicines, such as corticosteroids, to reduce swelling and pressure within the skull.
- Anticonvulsant medicines, such as phenytoin (Dilantin), to stop or prevent seizures.
Follow-up therapy
If you experience complications of encephalitis, you might need additional therapy, such as:
- Brain rehabilitation to improve cognition and memory.
- Physical therapy to improve strength, flexibility, balance, motor coordination and mobility.
- Occupational therapy to develop everyday skills and to use adaptive products that help with everyday activities.
- Speech therapy to relearn muscle control and coordination to produce speech.
- Psychotherapy to learn coping strategies and new behavioral skills to improve mood disorders or address personality changes.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
Serious illness associated with encephalitis is usually severe and relatively sudden, so seek emergency care. The emergency care team will likely include specialists in infectious diseases, the brain and nervous system (neurologist).
Questions from your doctor
You may need to answer these questions, or answer them on behalf of your child or another person with severe illness:
- When did the symptoms begin?
- Have you recently started taking any new medicines? If so, what is the medicine?
- Have you been bitten by a mosquito or tick during the past few weeks?
- Have you traveled recently? Where?
- Have you recently had a cold, flu or other illness?
- Are you up to date on your immunizations? When was your last one?
- Have you had any exposure to wild animals or known toxins recently?
- Have you had unprotected sex with a new or long-term sexual partner?
- Do you have a condition or take any medicines that result in a weakened immune system?
- Do you have an autoimmune condition or do autoimmune conditions run in the family?