Granulomatous Disease, Chronic, Autosomal Recessive, Cytochrome B-Positive, Type I
A number sign (#) is used with this entry because autosomal recessive cytochrome b-positive chronic granulomatous disease (CGD) type I is caused by mutation in the NCF1 gene (608512), which encodes the p47-phox (phagocyte oxidase) protein.
A less common form of autosomal cytochrome b-positive chronic granulomatous disease, type II (233710), is caused by mutation in the NCF2 gene (608515), which encodes the p67-phox protein.
For a phenotypic description of chronic granulomatous disease, see the well-established X-linked recessive cytochrome b-negative form (CGD; 306400).
Clinical FeaturesAzimi et al. (1968) described 3 black sisters with a clinical course and leukocyte behavior in vitro like those in affected males with X-linked CGD. In both families, parents showed normal leukocyte function.
In 8 patients, including 7 women with an autosomal recessive form of CGD, Segal et al. (1983) found that cytochrome b(-245) was present, but nonfunctional. Among 22 cases of clinically typical CGD, Bohler et al. (1986) found 4 (2 males, 2 females) with normal amounts of cytochrome b in granulocytes, but absent oxidative activity.
In 7 patients with the autosomal recessive, cytochrome b-positive form of CGD, Curnutte et al. (1988) found severe deficiency of a cytosol factor necessary for the activation of NADPH oxidase. Obligate heterozygotes showed an intermediate level of cytosol factor activity. They commented that the clinical severity of the autosomal recessive, cytochrome b-positive form of CGD appeared to be less than that in the cytochrome b-negative form. In their series, CGD was not diagnosed in 2 of the patients until ages 30 and 9, respectively, when each developed hepatic abscesses. Their previous medical histories were significant only for impetiginous skin lesions. Another patient had only 1 serious illness, Legionella pneumonia, in addition to occasional skin infections. A patient who had the highest level of cytosol factor activity had been healthy and was diagnosed only after her brother died of Aspergillus pneumonitis.
Van de Vosse et al. (2009) reported a 25-year-old woman with CGD who first presented with a Staphylococcus aureus-positive hepatic abscess. Molecular studies showed compound heterozygosity for 2 truncating mutations in the NCF1 gene, resulting in complete absence of the NADPH-oxidase complex. The authors commented on the late presentation of this individual.
PathogenesisHamers et al. (1984) showed that when monocytes of the X-linked cytochrome b-negative form (306400) of CGD are fused with monocytes from the autosomal cytochrome b-positive form, the resultant hybrid cells are cytochrome b-positive and express nitroblue tetrazolium (NBT) reductase activity, indicating complementation of the superoxide/hydrogen peroxide generating system. The findings demonstrated genetic heterogeneity of CGD.
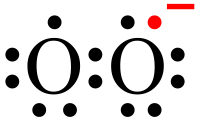
In an editorial, Karnovsky (1983) noted that in the autosomal form of CGD, cytochrome b(-245) is normally present, but the machinery that reduces (adds electrons or hydrogen to) the cytochrome is defective, indicating 2 main divisions of cellular enzymology in these patients. Segal (1985) gave a useful review of the molecular basis of CGD, viewed as a syndrome caused by any defect in the function of the electron transport chain essential to the microbicidal activity of white cells.
One of the major common pathways for activation of neutrophils seems to be protein phosphorylation, which can be directly activated by phorbol myristate acetate (PMA), a potent stimulus of the oxidase system. Using SDS-polyacrylamide gel electrophoresis followed by autoradiography, Segal et al. (1985) demonstrated that cells from 4 patients with autosomal recessive CGD demonstrated a consistent failure to phosphorylate a protein band with an apparent molecular weight of 47 kD. Cells from normal subjects and from 2 patients with X-linked CGD showed normal phosphorylation. The authors suggested that failure to phosphorylate the protein in autosomal CGD could result either from an absence of the protein or replacement of the amino acid target of phosphorylation, usually serine or threonine, due to a point mutation.
Caldwell et al. (1988) demonstrated that the cytosolic factor that is required for activation of NADPH oxidase and is deficient in the autosomal recessive form of CGD also regulates phosphorylation of a specific 48-kD protein. The authors suggested that the protein may be related to the functional and phosphorylation defects present in CGD polymorphonuclear leukocytes and to the activation of NADPH oxidase in the cell-free system. Nunoi et al. (1988) found that a 47-kD neutrophil cytosol factor separated from normal neutrophil cytosol can restore normal respiratory burst activity to defective neutrophil cytosol from most patients with autosomally inherited CGD when tested in a cell-free superoxide-generating system. In their studies they found that a 65-kD factor, NCF2, also restored activity to defective neutrophil cytosol from 1 patient with autosomal CGD. NCF1, NCF2, and a third cytosol fraction, NCF3, were inactive alone or in pairs, but together the 3 replaced unfractionated cytosol in cell-free superoxide generation. Volpp et al. (1988) raised a polyclonal antiserum that recognized the 47-kD and 67-kD proteins and showed that the neutrophils from patients with 2 different forms of autosomal CGD lacked either the 47- or the 67-kD protein. A deficiency of the 47-kD protein is more frequent than that of the 67-kD protein.
Bolscher et al. (1989) studied the soluble fraction that is required for NADPH oxidase activation in a cell-free system. They showed that at least 2 soluble components are necessary for reconstitution of the NADPH oxidase activity: one that does not bind to carboxymethyl Sepharose and one that does bind. These components were designated soluble oxidase component I (SOC1) and II (SOC2), respectively. SOC2 copurified with the 47-kD phosphoprotein previously found to be defective in patients with the autosomal form of CGD. Inactive soluble fractions of cells from autosomal CGD patients were reconstituted with a SOC2 fraction from control cells. The authors concluded that some autosomal CGD patients are normal in SOC1 and defective in SOC2.
Rodaway et al. (1990) raised the possibility that patients with CGD may have a defect in lymphocyte function.
Clinical ManagementLiese et al. (2000) evaluated the effect of antibiotic and antifungal long-term prophylaxis on the prognosis of CGD in 39 patients with different subtypes, both X-linked and autosomal recessive. Antibiotic prophylaxis with TMP-SMX significantly decreased the incidence of severe infections in patients with complete loss of cytochrome b activity but had no significant effect in patients with the other subtypes. Eight of the patients with complete absence of cytochrome b activity were also given itraconazole, and none developed fungal infections over 15.5 patient-years, whereas patients of all subtypes who received only antibiotics showed an increase in severe fungal infections. The different subtypes were also analyzed for age at diagnosis, age at first infection, and long-term survival.
Molecular GeneticsClark et al. (1989) concluded that the autosomal form of CGD due to deficiency of NCF1 represents about 33% of all cases of CGD; the autosomal form due to deficiency of NCF2 represents about 5% of cases.
In 3 unrelated patients with autosomal recessive CGD, Casimir et al. (1991) identified a 2-bp deletion in the NCF1 gene (608512.0001). Casimir et al. (1991) stated that about 30% of CGD cases are autosomal recessive and that more than 90% of the autosomal recessive cases have a defect in the 47-kD cytosolic protein.
Unlike other CGD subtypes, in which there is great heterogeneity among mutations, 97% of affected alleles in patients with p47-PHOX deficiency carry the 2-bp deletion in the NCF1 gene (Noack et al., 2001). In each of the 4 patients who were heterozygous for the GT deletion, Noack et al. (2001) identified additional mutations in the NCF1 gene (see, e.g., 608512.0003-608512.0004).
Gorlach et al. (1997) found that in each of 34 consecutive unrelated normal individuals, both the normal and mutant delta-GT sequences were present in genomic DNA. Further study revealed that this finding was due to the p47-phox pseudogene containing the delta-GT mutation. This close linkage, together with the presence within each gene of multiple recombination hotspots, suggested that the predominance of the delta-GT mutation in this autosomal recessive form of CGD is caused by recombination events between the wildtype gene and the pseudogene(s). Gene conversion events between homologous genes and their pseudogenes had been described in the pathogenesis of several genetic disorders, such as 21-hydroxylase deficiency (201910), von Willebrand disease (193400), and Gaucher disease (230800).
Roesler et al. (2000) performed sequence analysis of 28 unrelated, racially diverse patients with the p47-phox-deficient form of CGD and 37 healthy individuals. In 25 patients, the CGD deletion in exon 2 was present in all alleles. Three patients and all healthy individuals contained GTGT and delta-GT sequences, the latter being a characteristic of the NCF1 pseudogene. A total of 22 patients carried additional pseudogene-specific intronic sequences on all alleles, either only in intron 1 or in intron 1 and intron 2, which led to different types of chimeric DNA strands. Roesler et al. (2000) concluded that recombination events between the NCF1 gene and its highly homologous pseudogenes result in the incorporation of delta-GT into the NCF1 gene, thereby leading to the high frequency of GT deletion in CGD patients with the p47-phox-deficient form.
Roos et al. (2006) identified 7 different mutations and a large deletion in the NCF1 gene in affected individuals from 9 unrelated families with autosomal recessive CGD. In 6 families, the patients were compound heterozygous for the common GT deletion and another pathogenic mutation. Patients from 2 families had a homozygous mutation, and a patient from 1 family was compound heterozygous for 2 mutations (see, e.g., 608512.0005-608512.0007).
HeterogeneityBy haplotype analysis and homozygosity mapping in 15 Tunisian patients with CDG from 14 unrelated families, El Kares et al. (2006) assigned the genetic defect to the NCF1 gene in 5 patients, the NCF2 gene in 4 patients, and the CYBA gene (608508) in 2 patients, and 2 patients appeared to have X-linked CDG. Haplotype analysis of 2 patients from a large consanguineous family showed heterozygosity around the 3 known CDG genes, and X-linked disease was excluded by the presence of a healthy male sib of unaffected parents, suggesting further genetic heterogeneity for CDG.
Gene TherapySekhsaria et al. (1993) demonstrated that hematopoietic progenitors, which can be harvested from peripheral blood in clinically relevant numbers by apheresis, can be used for gene therapy in this form of CGD. They used a replication-defective retrovirus encoding p47-phox to transduce peripheral blood hematopoietic progenitors (PBHPs) from patients with this disorder and demonstrated significant correction of microbicidal superoxide generation when the PBHPs were differentiated to mature neutrophils and monocytes.
HistoryHolmes et al. (1970) presented evidence suggesting that leukocyte glutathione peroxidase activity (138320) is defective in females with chronic granulomatous disease. Later studies of the patients reported by Holmes et al. (1970) showed normal glutathione peroxidase activity and mutations in the CYBB gene (300481) (Newburger et al., 1994).
Matsuda et al. (1976) described a male child with CGD who had glutathione peroxidase deficiency. Both parents had an intermediate level of glutathione peroxidase. Data interpreted as indicating deficiency of leukocyte glutathione peroxidase are suspect, however, since investigators using cells from infected normals as controls have not found low GPX (Johnston and Winkelstein, 1982). Furthermore, animals with severe deficiency of GPX are said to have no bactericidal defect.
Good (1975) listed the Ford familial lipochrome histiocytosis (235900) as type 3 CGD. Corberand et al. (1978) described G6PD-deficient CGD in a female with first-cousin parents. (See 300908 for further discussion of G6PD-deficient CGD.)
Kimpen et al. (1991) proposed that the autosomal recessive form of CGD might be due to a mutation on 18q because they observed the association of CGD with 18q- syndrome. In fact, the 3 forms of autosomal recessive CGD are known to map to chromosomes 1, 7, and 16.
Animal ModelJackson et al. (1995) developed a p47(phox-/-) 'knock-out' CGD mouse that had a phenotype identical to its human counterpart, including increased susceptibility to spontaneous lethal infections. Mardiney et al. (1997) used this CGD mouse model to study retrovirus-mediated gene therapy targeting hematopoietic stem cells to address some of the issues raised in an ongoing human phase 1 clinical study of gene therapy of this form of CGD. Hematopoietic progenitor cells (HPCs) were derived from nonprimed bone marrow, and the recipient mice received a moderate dose of radiation as conditioning before transplantation. Using these conditions, gene therapy in the p47-deficient CGD mice resulted in long-term correction of NADPH oxidase function in a percentage of neutrophils sufficient to restore NADPH oxidase-dependent host-defense function.
During inflammation, indoleamine 2,3-dioxygenase (IDO; 147435) is upregulated in dendritic cells and phagocytes by proinflammatory stimuli, most notably, IFNG (147570), and the enzyme then uses superoxide as a 'cofactor' for oxidative cleavage of the indole ring of tryptophan, yielding an intermediate that deformylates to L-kynurenine. Romani et al. (2008) demonstrated that a superoxide-dependent step in tryptophan metabolism along the kynurenine pathway is blocked in CGD mice deficient in p47 with lethal pulmonary aspergillosis (see 614079), leading to unrestrained V-gamma-1+ gamma-delta T-cell reactivity, dominant production of interleukin-17 (IL17; 603149), defective regulatory T-cell activity, and acute inflammatory lung injury. Although beneficial effects are induced by IL17 neutralization or gamma-delta T-cell contraction, complete cure and reversal of the hyperinflammatory phenotype are achieved by replacement therapy with a natural kynurenine distal to the blockade in the pathway. Effective therapy, which includes coadministration of recombinant IFNG, restores production of downstream immunoactive metabolites and enables the emergence of regulatory V-gamma-4+ gamma-delta and Foxp3+ (300292) alpha-beta T cells. Therefore, Romani et al. (2008) concluded that paradoxically, the lack of reactive oxygen species contributes to the hyperinflammatory phenotype associated with NADPH oxidase deficiencies, through a dysfunctional kynurenine pathway of tryptophan catabolism. Yet this condition can be reverted by reactivating the pathway downstream of the superoxide-dependent step.
Deffert et al. (2014) conducted a literature search that found nearly 300 cases of mycobacterial infection in CGD, principally caused by M. bovis bacillus Calmette-Guerin (BCG). The authors then investigated BCG infection in 3 different mouse models of CGD: 2 strains of mice lacking Ncf1 and mice lacking Cybb. All 3 CGD mouse strains were highly susceptible to intravenous BCG infection, manifest as severe weight loss, hemorrhagic pneumonia with high numbers of neutrophils, and 50% mortality. These mice had only moderately increased bacterial load. Macrophage-specific rescue of Cybb restored BCG resistance. Reactive oxygen species was generated in granulomas of wildtype mice, but not CGD mice. Massive increases in the release of the cytokines Tnf (191160), Ifng, Il17, and Il12 (161561), as well as Cxcl1 (155730), a neutrophil chemoattractant, occurred early after infection in CGD mice, possibly explaining disease severity. Macrophages clustered in granulomas in wildtype mice, whereas macrophages were diffusely distributed in lungs of CGD mice. Deffert et al. (2014) concluded that lack of NADPH oxidase leads to markedly increased severity of BCG infection through increased cytokine production and reduced granuloma formation.