Short-Rib Thoracic Dysplasia 10 With Or Without Polydactyly
A number sign (#) is used with this entry because of evidence that short-rib thoracic dysplasia-10 with or without polydactyly (SRTD10) is caused by homozygous or compound heterozygous mutation in the IFT172 gene (607386) on chromosome 2p23.
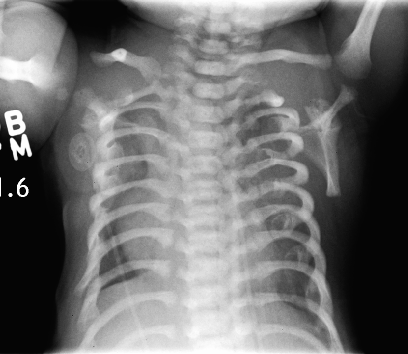
DescriptionShort-rib thoracic dysplasia (SRTD) with or without polydactyly refers to a group of autosomal recessive skeletal ciliopathies that are characterized by a constricted thoracic cage, short ribs, shortened tubular bones, and a 'trident' appearance of the acetabular roof. SRTD encompasses Ellis-van Creveld syndrome (EVC) and the disorders previously designated as Jeune syndrome or asphyxiating thoracic dystrophy (ATD), short rib-polydactyly syndrome (SRPS), and Mainzer-Saldino syndrome (MZSDS). Polydactyly is variably present, and there is phenotypic overlap in the various forms of SRTDs, which differ by visceral malformation and metaphyseal appearance. Nonskeletal involvement can include cleft lip/palate as well as anomalies of major organs such as the brain, eye, heart, kidneys, liver, pancreas, intestines, and genitalia. Some forms of SRTD are lethal in the neonatal period due to respiratory insufficiency secondary to a severely restricted thoracic cage, whereas others are compatible with life (summary by Huber and Cormier-Daire, 2012 and Schmidts et al., 2013).
There is phenotypic overlap with the cranioectodermal dysplasias (Sensenbrenner syndrome; see CED1, 218330).
For a discussion of genetic heterogeneity of short-rib thoracic dysplasia, see SRTD1 (208500).
Clinical FeaturesCasteels et al. (2000) reported a 5.5-year-old girl who presented with vision loss and night blindness. Her visual acuity was 20/200 bilaterally, and she could not read Ishihara color plates. There was an inferior visual field defect bilaterally, with waxy optic discs, narrow blood vessels, and midperiphery irregular pigmentation on funduscopy, and no rod or cone response could be detected by electroretinography (ERG). Further examination revealed a hypoplastic right thoracic cage and a mildly hypoplastic left hemithorax. Her limbs showed rhizomelic shortening, with brachydactyly and short phalanges; her height was within the 3rd to 25th percentile for age. She had been born with an extra fifth digit on each hand (postaxial polydactyly), which had been surgically removed. Radiographs from the neonatal period showed trident acetabulum with median spur arising from the acetabulum, and x-rays at 5 years of age showed cone-shaped epiphyses in several phalangeal bones of the hands and feet. Due to the combination of thoracic hypoplasia with pelvic and phalangeal abnormalities, a clinical diagnosis of Jeune syndrome was made.
Halbritter et al. (2013) studied 14 patients from 12 families with mutations in the IFT172 gene who shared a phenotype that included skeletal abnormalities, nephronophthisis, and liver and eye involvement, consistent with a clinical diagnosis of complex asphyxiating thoracic dystrophy or Mainzer-Saldino syndrome. Most affected individuals exhibited nephronophthisis with progressive renal insufficiency in childhood and reached end-stage renal disease by 20 years of age. In addition, 2 Filipino sibs and a South American patient had thoracic dystrophy with chronic respiratory distress, necessitating intermittent mechanical ventilation; all 3 presented the ATD features of thoracic dystrophy with a trident acetabular roof and shortening of the long bones. The 2 Filipino sibs as well as 2 European American sibs and a German patient displayed phalangeal cone-shaped epiphyses, a hallmark of MZSDS, in addition to liver fibrosis and retinal dystrophy. Both Filipino sibs and a female Hungarian patient also had cerebellar vermis hypoplasia, which Halbritter et al. (2013) noted was a classic feature of Joubert syndrome (see 213300). In addition, 3 of the patients with an MZSDS phenotype as well as the female Hungarian patient exhibited obesity and impaired glucose tolerance, suggesting phenotypic overlap with Bardet-Biedl syndrome (209900).
Molecular GeneticsIn a multicenter cohort of 1,530 individuals with nephronophthisis (NPHP)-related ciliopathies, Halbritter et al. (2013) performed a candidate gene screening of all 14 genes encoding IFTB-complex proteins and identified homozygous or compound heterozygous mutations in the IFT172 gene (607386.0001-607386.0007) in 7 patients from 5 families. Sanger sequencing of exons and intron-exon boundaries of the 14 IFTB-complex genes in another cohort of 296 individuals with ciliopathies revealed compound heterozygous mutations in IFT172 (607386.0001; 607386.0008) in a Belgian girl with a clinical diagnosis of Jeune syndrome, originally described by Casteels et al. (2000). Exon-enriched next-generation sequencing in another 155 patients with NPHP-related ciliopathies identified 2 female patients with compound heterozygous IFT172 mutations (see, e.g., 607386.0001 and 607386.0009). Whole-exome resequencing, independently performed in a cohort of 116 individuals with ATD in the United Kingdom and 7 ATD patients in Australia, identified 4 more patients with mutations in IFT172 (607386.0001 and 607386.0010-607386.0012). Fibroblasts from affected individuals showed disturbed ciliary composition, suggesting alteration of ciliary transport and signaling, and knockdown of ift172 in zebrafish recapitulated the human phenotype.
NomenclatureSome of the patients with SRTD10 reported by Halbritter et al. (2013) had nephronophthisis; Halbritter et al. (2013) designated the nephronophthisis in this disorder as 'NPHP17.'