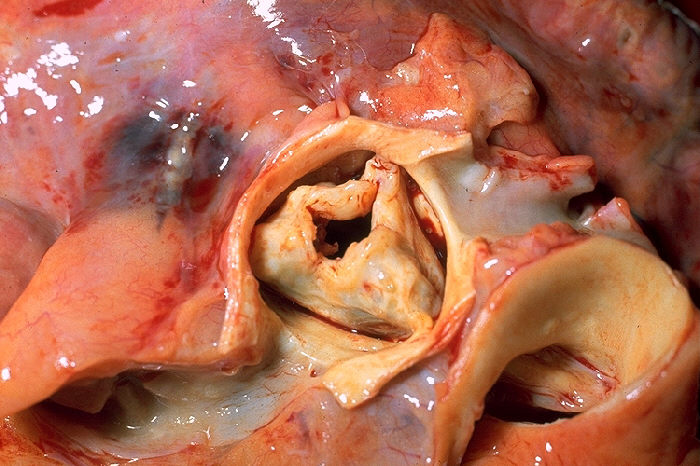
Aortic Stenosis
Aortic stenosis (AS or AoS) is the narrowing of the exit of the left ventricle of the heart (where the aorta begins), such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without narrowing is known as aortic sclerosis.
Causes include being born with a bicuspid aortic valve, and rheumatic fever; a normal valve may also harden over the decades. A bicuspid aortic valve affects about one to two percent of the population. As of 2014 rheumatic heart disease mostly occurs in the developing world. Risk factors are similar to those of coronary artery disease and include smoking, high blood pressure, high cholesterol, diabetes, and being male. The aortic valve usually has three leaflets and is located between the left ventricle of the heart, and the aorta. AS typically results in a heart murmur. Its severity can be divided into mild, moderate, severe, and very severe, distinguishable by ultrasound scan of the heart.
Aortic stenosis is typically followed using repeated ultrasound scans. Once it has become severe, treatment primarily involves valve replacement surgery, with transcatheter aortic valve replacement (TAVR) being an option in some who are at high risk from surgery. Valves may either be mechanical or bioprosthetic, with each having risks and benefits. Another less invasive procedure, balloon aortic valvuloplasty (BAV), may result in benefit, but for only a few months. Complications such as heart failure may be treated in the same way as in those with mild to moderate AS. In those with severe disease a number of medications should be avoided, including ACE inhibitors, nitroglycerin, and some beta blockers. Nitroprusside or phenylephrine may be used in those with decompensated heart failure depending on the blood pressure.
Aortic stenosis is the most common valvular heart disease in the developed world. It affects about 2% of people who are over 65 years of age. Estimated rates were not known in most of the developing world as of 2014. In those who have symptoms, without repair the chance of death at five years is about 50% and at 10 years is about 90%. Aortic stenosis was first described by French physician Lazare Rivière in 1663.
Signs and symptoms
Symptoms related to aortic stenosis depend on the degree of stenosis. Most people with mild to moderate aortic stenosis do not have symptoms. Symptoms usually present in individuals with severe aortic stenosis, though they may also occur in those with mild to moderate aortic stenosis. The three main symptoms of aortic stenosis are loss of consciousness, anginal chest pain and shortness of breath with activity or other symptoms of heart failure such as shortness of breath while lying flat, episodes of shortness of breath at night, or swollen legs and feet. It may also be accompanied by the characteristic "Dresden china" appearance of pallor with a light flush.
Angina
Angina in setting of heart failure also increases the risk of death. In people with angina, the 5-year mortality rate is 50% if the aortic valve is not replaced.
Angina in the setting of AS occurs due to left ventricular hypertrophy (LVH) that is caused by the constant production of increased pressure required to overcome the pressure gradient caused by the AS. While the muscular layer of the left ventricle thickens, the arteries that supply the muscle do not get significantly longer or bigger, so the muscle may not receive enough blood supply to meet its oxygen requirement. This ischemia may first be evident during exercise when the heart muscle requires increased blood supply to compensate for the increased workload. The individual may complain of anginal chest pain with exertion. At this stage, a cardiac stress test with imaging may be suggestive of ischemia.
Eventually, however, the heart muscle will require more blood supply at rest than can be supplied by the coronary artery branches. At this point there may be signs of ventricular strain pattern (ST segment depression and T wave inversion) on the EKG, suggesting subendocardial ischemia. The subendocardium is the region that is most susceptible to ischemia because it is the most distant from the epicardial coronary arteries.
Syncope
Syncope (fainting spells) from aortic valve stenosis is usually exertional. In the setting of heart failure it increases the risk of death. In people with syncope, the three-year mortality rate is 50% if the aortic valve is not replaced.
It is unclear why aortic stenosis causes syncope. One theory is that severe AS produces a nearly fixed cardiac output. When a person with aortic stenosis exercises, their peripheral vascular resistance will decrease as the blood vessels of the skeletal muscles dilate to allow the muscles to receive more blood to allow them to do more work. This decrease in peripheral vascular resistance is normally compensated for by an increase in the cardiac output. Since people with severe AS cannot increase their cardiac output, the blood pressure falls and the person will faint due to decreased blood perfusion to the brain.
A second theory is that during exercise the high pressures generated in the hypertrophied left ventricle cause a vasodepressor response, which causes a secondary peripheral vasodilation that, in turn, causes decreased blood flow to the brain resulting in loss of consciousness. Indeed, in aortic stenosis, because of the fixed obstruction to blood flow out from the heart, it may be impossible for the heart to increase its output to offset peripheral vasodilation.
A third mechanism may sometimes be operative. Due to the hypertrophy of the left ventricle in aortic stenosis, including the consequent inability of the coronary arteries to adequately supply blood to the myocardium (see "Angina" below), abnormal heart rhythms may develop. These can lead to syncope.
Finally, in calcific aortic stenosis at least, the calcification in and around the aortic valve can progress and extend to involve the electrical conduction system of the heart. If that occurs, the result may be heart block, a potentially lethal condition of which syncope may be a symptom.
Congestive heart failure
Congestive heart failure (CHF) carries a grave prognosis in people with AS. People with CHF attributable to AS have a 2-year mortality rate of 50% if the aortic valve is not replaced. CHF in the setting of AS is due to a combination of left ventricular hypertrophy with fibrosis, systolic dysfunction (a decrease in the ejection fraction) and diastolic dysfunction (elevated filling pressure of the LV).
Associated symptoms
In Heyde's syndrome, aortic stenosis is associated with gastrointestinal bleeding due to angiodysplasia of the colon. Recent research has shown that the stenosis causes a form of von Willebrand disease by breaking down its associated coagulation factor (factor VIII-associated antigen, also called von Willebrand factor), due to increased turbulence around the stenotic valve.
Complications
Notwithstanding the foregoing, the American Heart Association has recently changed its recommendations regarding antibiotic prophylaxis for endocarditis. Specifically, as of 2007 it is recommended that such prophylaxis should be limited only to those with prosthetic heart valves, those with previous episode(s) of endocarditis, and those with certain types of congenital heart disease.
Since the stenosed aortic valve may limit the heart's output, people with aortic stenosis are at risk of syncope and dangerously low blood pressure should they use any of a number of medications for cardiovascular diseases that often coexist with aortic stenosis. Examples include nitroglycerin, nitrates, ACE inhibitors, terazosin (Hytrin), and hydralazine. Note that all of these substances lead to peripheral vasodilation. Under normal circumstances, in the absence of aortic stenosis, the heart is able to increase its output and thereby offset the effect of the dilated blood vessels. In some cases of aortic stenosis, however, due to the obstruction of blood flow out of the heart caused by the stenosed aortic valve, cardiac output cannot be increased. Low blood pressure or syncope may ensue.
Causes

Aortic stenosis is most commonly caused by age-related progressive calcification (>50% of cases), with a mean age of 65 to 70 years. Another major cause of aortic stenosis is the calcification of a congenital bicuspid aortic valve or, more rarely, congenital unicuspid aortic valve. Those with unicuspid aortic valve typically need intervention when very young, often as a newborn. While those with congenital bicuspid aortic valve make up 30-40% of those presenting during adulthood and typically presenting earlier (ages 40+ to 50+) than those with tricuspid aortic valves (65+).
Acute rheumatic fever post-inflammatory is the cause of less than 10% of cases. Rare causes of aortic stenosis include Fabry disease, systemic lupus erythematosus, Paget disease, high blood uric acid levels, and infection.
Pathophysiology

The human aortic valve normally consists of three cusps or leaflets and has an opening of 3.0-4.0 square centimeters. When the left ventricle contracts, it forces blood through the valve into the aorta and subsequently to the rest of the body. When the left ventricle expands again, the aortic valve closes and prevents the blood in the aorta from flowing backward (regurgitation) into the left ventricle. In aortic stenosis, the opening of the aortic valve becomes narrowed or constricted (stenotic) (e.g., due to calcification). Degenerative (the most common variety), and bicuspid aortic stenosis both begin with damage to endothelial cells from increased mechanical stress. Inflammation is thought to be involved in the earlier stages of the pathogenesis of AS and its associated risk factors are known to promote the deposition of LDL cholesterol and lipoprotein(a), a highly damaging substance, into the aortic valve, causing significant damage and stenosis over time.
As a consequence of this stenosis, the left ventricle must generate a higher pressure with each contraction to effectively move blood forward into the aorta. Initially, the LV generates this increased pressure by thickening its muscular walls (myocardial hypertrophy). The type of hypertrophy most commonly seen in AS is known as concentric hypertrophy, in which the walls of the LV are (approximately) equally thickened.
In the later stages, the left ventricle dilates, the wall thins, and the systolic function deteriorates (resulting in impaired ability to pump blood forward). Morris and Innasimuthu et al. showed that different coronary anatomy is associated with different valve diseases. Research was in progress in 2010 to see if different coronary anatomy might lead to turbulent flow at the level of valves leading to inflammation and degeneration.
Diagnosis

Aortic stenosis is most often diagnosed when it is asymptomatic and can sometimes be detected during routine examination of the heart and circulatory system. Good evidence exists to demonstrate that certain characteristics of the peripheral pulse can rule in the diagnosis. In particular, there may be a slow and/or sustained upstroke of the arterial pulse, and the pulse may be of low volume. This is sometimes referred to as pulsus parvus et tardus. There may also be a noticeable delay between the first heart sound (on auscultation) and the corresponding pulse in the carotid artery (so-called 'apical-carotid delay'). In a similar manner, there may be a delay between the appearance of each pulse in the brachial artery (in the arm) and the radial artery (in the wrist).
The first heart sound may be followed by a sharp ejection sound ("ejection click") best heard at the lower left sternal border and the apex, and, thus, appear to be "split". The ejection sound, caused by the impact of left ventricular outflow against the partially fused aortic valve leaflets, is more commonly associated with a mobile bicuspid aortic valve than an immobile calcified aortic valve. The intensity of this sound does not vary with respiration, which helps distinguish it from the ejection click produced by a stenotic pulmonary valve, which will diminish slightly in intensity during inspiration.
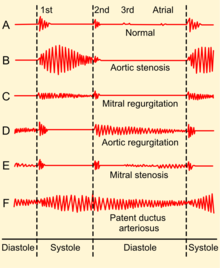
An easily heard systolic, crescendo-decrescendo (i.e., 'ejection') murmur is heard loudest at the upper right sternal border, at the 2nd right intercostal space, and radiates to the carotid arteries bilaterally. The murmur increases with squatting and decreases with standing and isometric muscular contraction such as the Valsalva maneuver, which helps distinguish it from hypertrophic obstructive cardiomyopathy (HOCM). The murmur is louder during expiration but is also easily heard during inspiration. The more severe the degree of the stenosis, the later the peak occurs in the crescendo-decrescendo of the murmur.
The second heart sound (A2) tends to become decreased and softer as the aortic stenosis becomes more severe. This is a result of the increasing calcification of the valve preventing it from "snapping" shut and producing a sharp, loud sound. Due to increases in left ventricular pressure from the stenotic aortic valve, over time the ventricle may hypertrophy, resulting in a diastolic dysfunction. As a result, there may be a fourth heart sound due to the stiff ventricle. With continued increases in ventricular pressure, dilatation of the ventricle will occur, and a third heart sound may be manifest.
Finally, aortic stenosis often co-exists with some degree of aortic insufficiency (aortic regurgitation). Hence, the physical exam in aortic stenosis may also reveal signs of the latter, for example, an early diastolic decrescendo murmur. Indeed, when both valve abnormalities are present, the expected findings of either may be modified or may not even be present. Rather, new signs that reflect the presence of simultaneous aortic stenosis and insufficiency, e.g., pulsus bisferiens, emerge.
According to a meta-analysis, the most useful findings for ruling in aortic stenosis in the clinical setting were slow rate of rise of the carotid pulse (positive likelihood ratio ranged 2.8–130 across studies), mid to late peak intensity of the murmur (positive likelihood ratio, 8.0–101), and decreased intensity of the second heart sound (positive likelihood ratio, 3.1–50).
Other peripheral signs include:
- sustained, heaving apex beat, which is not displaced unless systolic dysfunction of the left ventricle has developed
- A precordial thrill
- narrowed pulse pressure
Electrocardiogram
Although aortic stenosis does not lead to any specific findings on the electrocardiogram (ECG), it still often leads to a number of electrocardiographic abnormalities. ECG manifestations of left ventricular hypertrophy (LVH) are common in aortic stenosis and arise as a result of the stenosis having placed a chronically high pressure load on the left ventricle (with LVH being the expected response to chronic pressure loads on the left ventricle no matter what the cause).
As noted above, the calcification process that occurs in aortic stenosis can progress to extend beyond the aortic valve and into the electrical conduction system of the heart. Evidence of this phenomenon may rarely include ECG patterns characteristic of certain types of heart block such as Left bundle branch block.
Heart catheterization
Cardiac chamber catheterization provides a definitive diagnosis, indicating severe stenosis in valve area of <1.0 cm2 (normally about 3 cm2). It can directly measure the pressure on both sides of the aortic valve. The pressure gradient may be used as a decision point for treatment. It is useful in symptomatic people before surgery. The standard for diagnosis of aortic stenosis is non-invasive testing with echocardiography. Cardiac catheterization is reserved for cases in which there is discrepancy between the clinical picture and non-invasive testing, due to risks inherent to crossing the aortic valve, such as stroke.
Echocardiogram
| Severity of aortic stenosis | ||
|---|---|---|
| Degree | Mean gradient (mmHg) |
Aortic valve area (cm2) |
| Mild | <25 | >1.5 |
| Moderate | 25 - 40 | 1.0 - 1.5 |
| Severe | >40 | < 1.0 |
| Very severe | >70 | < 0.6 |
Echocardiogram (heart ultrasound) is the best non-invasive way to evaluate the aortic valve anatomy and function.
The aortic valve area can be calculated non-invasively using echocardiographic flow velocities. Using the velocity of the blood through the valve, the pressure gradient across the valve can be calculated by the continuity equation or using the modified Bernoulli's equation:
Gradient = 4(velocity)² mmHg
A normal aortic valve has a gradient of only a few mmHg. A decreased valvular area causes increased pressure gradient, and these parameters are used to classify and grade the aortic stenosis as mild, moderate or severe. The pressure gradient can be abnormally low in the presence of mitral stenosis, heart failure, co-existent aortic regurgitation and also ischaemic heart disease (disease related to decreased blood supply and oxygen causing ischemia).
Echocardiogram may also show left ventricular hypertrophy, thickened and immobile aortic valve and dilated aortic root. However, it may appear deceptively normal in acute cases.
Chest X-ray
A chest X-ray can also assist in the diagnosis and provide clues as to the severity of the disease, showing the degree of calcification of the valve, and in a chronic condition, an enlarged left ventricle and atrium.
Management
Treatment is generally not necessary in people without symptoms. In moderate cases echocardiography is performed every 1–2 years to monitor the progression, possibly complemented with a cardiac stress test. In severe cases, echocardiography is performed every 3–6 months. In both moderate and mild cases, the person should immediately make a revisit or be admitted for inpatient care if any new related symptoms appear. There are no therapeutic options currently available to treat people with aortic valve stenosis; however, studies have indicated that the disease occurs as a result of active cellular processes, suggesting that targeting these processes may lead to viable therapeutic approaches.
Medication
The effect of statins on the progression of AS is unclear. The latest trials do not show any benefit in slowing AS progression, but did demonstrate a decrease in ischemic cardiovascular events.
In general, medical therapy has relatively poor efficacy in treating aortic stenosis. However, it may be useful to manage commonly coexisting conditions that correlate with aortic stenosis:
- Any angina is generally treated with beta-blockers and/or calcium blockers. Nitrates are contraindicated due to their potential to cause profound hypotension in aortic stenosis.
- Any hypertension is treated aggressively, but caution must be taken in administering beta-blockers.
- Any heart failure is generally treated with digoxin and diuretics, and, if not contraindicated, cautious administration of ACE inhibitors.
While observational studies demonstrated an association between lowered cholesterol with statins and decreased progression, a randomized clinical trial published in 2005 failed to find any effect on calcific aortic stenosis. A 2007 study did find a slowing of aortic stenosis with the statin rosuvastatin.
Aortic valve repair
Aortic valve repair or aortic valve reconstruction describes the reconstruction of both form and function of the native and dysfunctioning aortic valve. Most frequently it is applied for the treatment of aortic regurgitation. It can also become necessary for the treatment of an aortic aneurysm, less frequently for congenital aortic stenosis.
Aortic valve replacement
In adults, symptomatic severe aortic stenosis usually requires aortic valve replacement (AVR). While AVR has been the standard of care for aortic stenosis for several decades, As of 2016[update] aortic valve replacement approaches include open heart surgery, minimally invasive cardiac surgery (MICS) and minimally invasive catheter-based (percutaneous) aortic valve replacement. However, surgical aortic valve replacement is well-studied, and generally has a good and well-established longer-term prognosis.
A diseased aortic valve is most commonly replaced using a surgical procedure with either a mechanical or a tissue valve. The procedure is done either in an open-heart surgical procedure or, in a smaller but growing number of cases, a minimally invasive cardiac surgery (MICS) procedure.
Transcatheter aortic valve replacement
Globally more than 250,000 people have received transcatheter aortic valve replacement (TAVR). For people who are not candidates for surgical valve replacement and most patients who are older than 75, TAVR may be a suitable alternative.
Balloon valvuloplasty
For infants and children, balloon valvuloplasty, where a balloon is inflated to stretch the valve and allow greater flow, may also be effective. In adults, however, it is generally ineffective, as the valve tends to return to a stenosed state. The surgeon will make a small incision at the top of the person's leg and proceed to insert the balloon into the artery. The balloon is then advanced up to the valve and is inflated to stretch the valve open.
Heart failure
Acute decompensated heart failure due to AS may be temporarily managed by an intra-aortic balloon pump while pending surgery. In those with high blood pressure nitroprusside may be carefully used. Phenylephrine may be used in those with very low blood pressure.
Prognosis
If untreated, severe symptomatic aortic stenosis carries a poor prognosis with a 2-year mortality rate of 50-60% and a 3-year survival rate of less than 30%. Prognosis after aortic valve replacement for people who are younger than 65 is about five years less than that of the general population; for people older than 65 it is about the same.
Epidemiology
Approximately 2% of people over the age of 65, 3% of people over age 75, and 4% percent of people over age 85 have aortic valve stenosis. The prevalence is increasing with the aging population in North America and Europe.
Risk factors known to influence disease progression of AS include lifestyle habits similar to those of coronary artery disease such as hypertension, advanced age, being male, hyperlipidemia, diabetes mellitus, cigarette smoking, metabolic syndrome, and end-stage kidney disease.
History
Aortic stenosis was first described by French physician Lazare Rivière in 1663.
Research
People on bisphosphonates were found in a 2010 study to have less progression of aortic stenosis, and some regressed. This finding led to multiple trials, ongoing as of 2012[update]. Subsequent research failed to confirm the initial positive result.