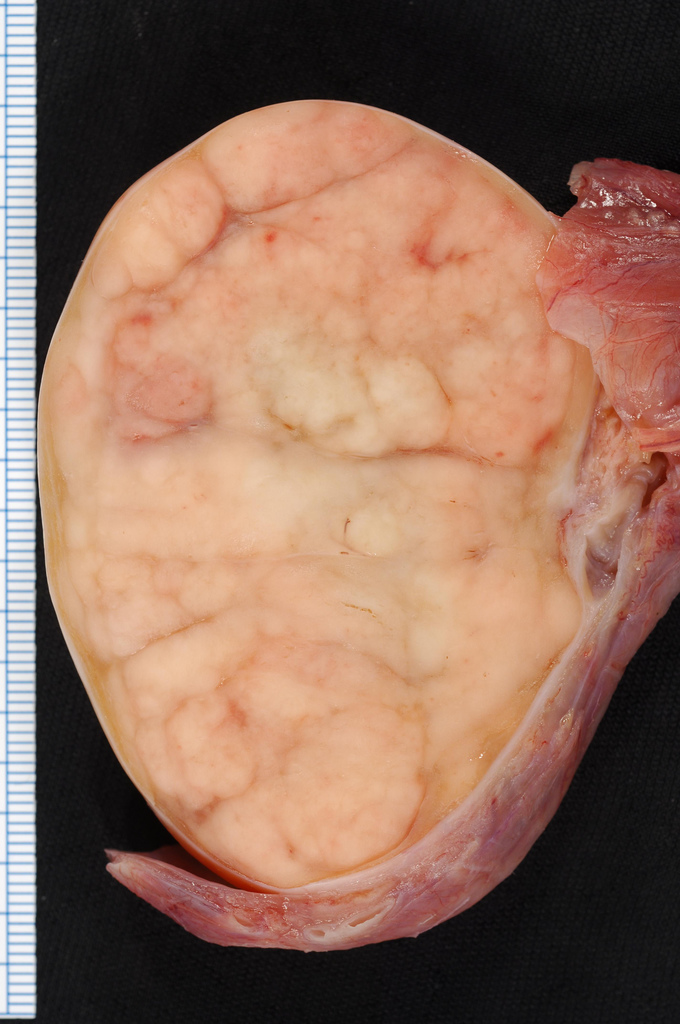
Testicular Seminomatous Germ Cell Tumor
Testicular seminomatous germ cell tumor is a rare testicular germ cell tumor (see this term), most commonly presenting with a painless mass in the scrotum, with a very high cure rate if caught in the early stages.
Epidemiology
Annual incidence in Europe is 1/62,000 people. It accounts for 40% of testicular cancer cases.
Clinical description
Seminoma usually presents in males between the ages of 30-40. A painless mass in the scrotum is indicative of disease. A long-standing hydrocele may be noted causing a feeling of heaviness in the testicle. Gynecomastia and back and flank pain are symptoms that are seen in some patients. Relapse after surgery can occur, usually (in 97% of cases) in the high iliac or retroperitoneal lymph nodes. Metastasis, although rare, can occur in some cases, affecting the lungs, liver, bones and central nervous system.
Etiology
Etiology is unknown but tumors are thought to arise from an embryonic germ cell leading to testicular intraepithelial neoplasia (the precursor to classical seminoma). Cryptorchidism is a risk factor for the development of testicular seminomatous germ cell tumors.
Diagnostic methods
Ultrasound usually confirms the presence of a testicular mass. Measurement of tumor markers in blood such as alpha-fetoprotein (AFP), beta human chorionic gonadotropin (BHC) and lactate dehydrogenase (LDH) is needed as it can be useful in cases where the tumor is still very small. Classical seminoma does not secrete AFP and patients with raised levels of this tumor marker are given a diagnosis of non-seminoma. After surgical removal of testicle, histopathological characteristics are analyzed and a stage can be assigned. In stage 1 disease the primary tumor is limited to the testis and epididymus with possible invasion of the tunica albuginea, tunica vaginalis, spermatic cord and scrotum but no lymph node or distant metastasis. Stage 2 (2A, 2B and 2C) disease features regional lymph node metastasis and stage 3 has distant metastasis of varying degrees.
Differential diagnosis
Testicular non seminomatous germ cell tumors (see this term) must be excluded.
Management and treatment
Treatment for stage 1 seminoma involves an orchiectomy or partial orchiectomy in some cases. Most patients (88%) do not require any further treatment and only surveillance is necessary. In those cases where follow up is difficult, adjuvant carboplatin or radiotherapy can be applied. Para-aortic and ipsilateral iliac radiotherapy (30 Gy in 2 Gy fractions) is the standard treatment of stage 2A seminoma. Cisplatin, etoposide and bleomycin (PEB) chemotherapy (three cycles) or cisplatin and etoposide (PE) chemotherapy (4 cycles) is an alternative to radiotherapy (but has more acute toxicity). Those with stage 2B, 2C and stage 3 seminomas are given PEB chemotherapy (three or four cycles depending on prognosis). In those with a reduced lung capacity or with emphysema or in severe smokers, 4 cycles of PE is preferred over PEB. Ifosfamide is given instead of bleomycin in certain cases (i.e. patients with existing lung damage). Follow up and sometimes a PET scan is recommended to monitor for residual lesions. Due to cosmetic and psychological reasons, patients may be offered testicular prostheses after an orchidectomy.
Prognosis
Prognosis is good but depends on the stage of disease with 5- year survival rates as high as 99% in stage 1 disease. Relapse rates at 5 years depend on risk factors (ex. invasion of the rete testis, tumor size >4cm) present, but is only 12% in those with no risk factors.