Emery-Dreifuss Muscular Dystrophy
Summary
Clinical characteristics.
Emery-Dreifuss muscular dystrophy (EDMD) is characterized by the clinical triad of: joint contractures that begin in early childhood; slowly progressive muscle weakness and wasting initially in a humero-peroneal distribution that later extends to the scapular and pelvic girdle muscles; and cardiac involvement that may manifest as palpitations, presyncope and syncope, poor exercise tolerance, and congestive heart failure along with variable cardiac rhythm disturbances. Age of onset, severity, and progression of muscle and cardiac involvement demonstrate both inter- and intrafamilial variability. Clinical variability ranges from early onset with severe presentation in childhood to late onset with slow progression in adulthood. In general, joint contractures appear during the first two decades, followed by muscle weakness and wasting. Cardiac involvement usually occurs after the second decade and respiratory function may be impaired in some individuals.
Diagnosis/testing.
The diagnosis of EDMD is established in a proband with:
- A clearly relevant clinical picture including limb muscle wasting and/or weakness and elbow or neck/spine joint contractures (cardiac disease may be missing in the first decades of life); AND
- A hemizygous pathogenic variant in EMD or FHL1, a heterozygous pathogenic variant in LMNA, or (more rarely) biallelic pathogenic variants in LMNA identified by molecular genetic testing.
Management.
Treatment of manifestations: Treatment for cardiac arrhythmias, AV conduction disorders, congestive heart failure, including antiarrhythmic drugs, cardiac pacemaker, implantable cardioverter defibrillator; heart transplantation for the end stages of heart failure as appropriate; respiratory aids (respiratory muscle training, assisted coughing techniques, mechanical ventilation) as needed. Surgery to release contractures and manage scoliosis as needed; aids (canes, walkers, orthoses, wheelchairs) as needed to help ambulation; physical therapy and stretching to prevent contractures.
Surveillance: At a minimum, annual cardiac assessment (ECG, Holter monitoring, echocardiography); monitoring of respiratory function.
Agents/circumstances to avoid: Triggering agents for malignant hyperthermia, such as depolarizing muscle relaxants (succinylcholine) and volatile anesthetic drugs (halothane, isoflurane); obesity.
Evaluation of relatives at risk: Molecular genetic testing if the pathogenic variant(s) in the family are known; clinical evaluation, including at least muscular and cardiac assessments if the pathogenic variant(s) in the family are not known.
Genetic counseling.
EDMD is inherited in an X-linked, autosomal dominant, or, rarely, autosomal recessive manner.
- XL-EDMD. If the mother of a proband has a pathogenic variant, the chance of transmitting it in each pregnancy is 50%. Males who inherit the pathogenic variant will be affected; females who inherit the pathogenic variant will be heterozygous. Heterozygous females are usually asymptomatic but are at risk of developing a cardiac disease, progressive muscular dystrophy, and/or an EDMD phenotype.
- AD-EDMD. 65% of probands with AD-EDMD have a de novo LMNA pathogenic variant. Each child of an individual with AD-EDMD has a 50% chance of inheriting the pathogenic variant.
- AR-EDMD. At conception, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being neither affected nor a carrier.
Once the pathogenic variant(s) have been identified in an affected family member, prenatal testing for a pregnancy at increased risk and preimplantation genetic testing for EDMD are possible.
Diagnosis
Suggestive Findings
Emery-Dreifuss muscular dystrophy (EDMD) should be suspected in individuals with the following triad [Emery 2000]:
- Early contractures of the elbow flexors, Achilles tendons (heels), and neck extensors resulting in limitation of neck flexion, followed by limitation of extension of the entire spine
- Slowly progressive wasting and weakness typically of the humero-peroneal/scapulo-peroneal muscles in the early stages
- Cardiac disease with conduction defects and arrhythmias
- Atrial fibrillation, flutter and standstill, supraventricular and ventricular arrhythmias, and atrio-ventricular and bundle-branch blocks may be identified on resting electrocardiography (ECG) or by 24-hour ambulatory ECG.
- Dilated or hypertrophic cardiomyopathy may be detected by the performance of echocardiographic evaluation.
Age of onset. Onset usually occurs between age five and ten years, rarely before age five years.
Family history. May be positive (autosomal dominant, X-linked, or, rarely, autosomal recessive). However, simplex cases due to de novo genetic events are not rare.
Note: Diagnosis guidelines have been published [Emery 1997, Bonne et al 2002b, Madej-Pilarczyk 2018].
Establishing the Diagnosis
The diagnosis of EDMD is established in a proband with a clearly relevant clinical picture including limb muscle wasting and/or weakness and elbow or neck/spine joint contractures (cardiac disease may be missing in the first decades of life) and a hemizygous pathogenic variant in EMD or FHL1, a heterozygous pathogenic variant in LMNA, or (more rarely) biallelic pathogenic variants in LMNA identified by molecular genetic testing (see Table 1).
Molecular genetic testing approaches can include a combination of gene-targeted testing (single-gene testing, multigene panel) and comprehensive genomic testing (exome sequencing, exome array, genome sequencing) depending on the phenotype.
Gene-targeted testing requires that the clinician determine which gene(s) are likely involved, whereas genomic testing does not. Because the phenotype of EDMD is broad, individuals with the distinctive findings described in Suggestive Findings are likely to be diagnosed using gene-targeted testing (see Option 1), whereas those with atypical features in whom the diagnosis of EDMD has not been considered are more likely to be diagnosed using genomic testing (see Option 2).
Option 1
When the phenotypic and laboratory findings suggest the diagnosis of EDMD, molecular genetic testing approaches can include single-gene testing or use of a multigene panel.
Single-gene testing. Sequence analysis detects small intragenic deletions/insertions and missense, nonsense, and splice site variants. If no pathogenic variant is found, perform gene-targeted deletion/duplication analysis to detect intragenic deletions or duplications. Note: Lack of amplification by PCR prior to sequence analysis can suggest a putative (multi)exon or whole-gene deletion on the X chromosome in affected males; confirmation requires additional testing by gene-targeted deletion/duplication analysis.
The likelihood of identifying a causative variant in EMD, FHL1, or LMNA is dependent on known or suspected mode of inheritance.
- In cases of X-linked inheritance, EMD-related disease is most likely, followed by FHL1.
- In cases of autosomal dominant or recessive inheritance, LMNA-related disease is most likely.
- In the absence of a clear inheritance pattern, LMNA-related disease is most likely followed by EMD- and then FHL1-related disease.
In an affected female who represents a simplex case (i.e., a single occurrence in a family) LMNA-related disease is more likely than an X-linked disorder. Carrier females rarely manifest X-linked EDMD (XL-EDMD); thus, affected females are much more likely to have AD-EDMD.
A multigene panel that includes EMD, FHL1, LMNA, and other genes of interest (see Differential Diagnosis) is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests. For this disorder a multigene panel that also includes deletion/duplication analysis is recommended (see Table 1).
For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
Option 2
When the diagnosis of EDMD is not considered because an individual has atypical phenotypic features, comprehensive genomic testing (which does not require the clinician to determine which gene[s] are likely involved) is the best option. Exome sequencing is most commonly used; genome sequencing is also possible.
Exome array (when clinically available) may be considered if exome sequencing is not diagnostic.
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 1.
Molecular Genetic Testing Used in Emery-Dreifuss Muscular Dystrophy (EDMD)
| Gene 1, 2 | Proportion of EDMD Attributed to Pathogenic Variants in Gene 3 | Proportion of Pathogenic Variants 4 Detectable by This Method | |
|---|---|---|---|
| Sequence analysis 5 | Gene-targeted deletion/duplication analysis 6 | ||
| EMD | 8.5% | 99% 7 | Rare 8, 9 |
| FHL1 | 1.2% | 99% 10 | Rare 7, 11 |
| LMNA | 26.5%% | 99% 12 | None reported 13 |
| Unknown | 63.4% | NA | |
- 1.
Genes are listed in alphabetic order.
- 2.
See Table A. Genes and Databases for chromosome locus and protein.
- 3.
Gueneau et al [2009]
- 4.
See Molecular Genetics for information on allelic variants detected in this gene.
- 5.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 6.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 7.
UMD-EMD Database
- 8.
Lack of amplification by PCR prior to sequence analysis can suggest a putative (multi)exon or whole-gene deletion on the X chromosome in affected males; confirmation requires additional testing by deletion/duplication analysis.
- 9.
Manilal et al [1998], Small & Warren [1998], Fujimoto et al [1999], Ankala et al [2012], Askree et al [2013]
- 10.
Gueneau et al [2009], Knoblauch et al [2010]
- 11.
Gueneau et al [2009], Tiffin et al [2013]
- 12.
UMD-LMNA Database
- 13.
Intragenic LMNA deletions and duplications have been associated with cardiomyopathy.
Clinical Characteristics
Clinical Description
AD-EDMD and XL-EDMD
Autosomal dominant Emery-Dreifuss muscular dystrophy (AD-EDMD) and X-linked EDMD (XL-EDMD) have similar but not identical neuromuscular and cardiac involvement [Yates et al 1999, Bonne et al 2000, Bonne et al 2002b, Boriani et al 2003, Astejada et al 2007, Gueneau et al 2009, Cowling et al 2011, Carboni et al 2012b, Madej-Pilarczyk 2018].
EDMD is characterized by the presence of the following clinical triad:
- Joint contractures that begin in early childhood in both XL-EDMD and AD-EDMD. In XL-EDMD, joint contractures are usually the first sign, whereas in AD-EDMD, joint contractures may appear after the onset of muscle weakness. Joint contractures predominate in the elbows, ankles, and posterior cervical muscles (responsible for limitation of neck flexion followed by limitation in movement of the entire spine). The degree and the progression of contractures are variable and not always age related [Bonne et al 2000]. Severe contractures may lead to loss of ambulation by limitation of movement of the spine and lower limbs.
- Slowly progressive muscle weakness and wasting that are initially in a humero-peroneal distribution and can later extend to the scapular and pelvic girdle muscles. The progression of muscle wasting is usually slow in the first three decades of life, after which it becomes more rapid. Loss of ambulation due to muscle weakness can occur in AD-EDMD but is rare in XL-EDMD [Bonne et al 2000].
- Cardiac involvement usually appears within the end of the second to third decades of life and may include palpitations, presyncope and syncope, poor exercise tolerance, congestive heart failure, and a variable combination of supraventricular arrhythmias, disorders of atrioventricular conduction, ventricular arrhythmias, dilated cardiomyopathy, and sudden death despite pacemaker implantation [Bécane et al 2000, Boriani et al 2003, Sanna et al 2003, Sakata et al 2005, Astejada et al 2007, Carboni et al 2012b].
- Cardiac conduction defects can include sinus bradycardia, first-degree atrioventricular block, bundle-branch blocks, Wenckebach phenomenon, and third-degree atrioventricular block requiring pacemaker implantation.
- Atrial arrhythmias (extrasystoles, atrial fibrillation, flutter) and ventricular arrhythmias (extrasystoles, ventricular tachycardia) are frequent.
- The risk for ventricular tachyarrhythmia and dilated cardiomyopathy manifested by left ventricular dilation and dysfunction is higher in AD-EDMD than in XL-EDMD.
- In both XL- and AD/AR-EDMD, affected individuals are at risk for cerebral emboli and sudden death [Boriani et al 2003, Redondo-Vergé et al 2011, Homma et al 2018].
- A generalized dilated (in LMNA- or EMD-related EDMD) or hypertrophic cardiomyopathy (in FHL1-related EDMD) often occurs.
Other clinical findings may be nonspecific:
- Electromyogram usually shows myopathic features with normal nerve conduction studies, but neuropathic patterns have been described for both XL-EDMD [Hopkins et al 1981] and AD- EDMD [Witt et al 1988].
- CT scan of muscle. Characteristic findings in the calf and posterior thigh muscles on MRI or CT scan have been reported in AD-EDMD [Mercuri et al 2002, Deconinck et al 2010, Carboni et al 2012a]. A similar pattern of muscle fatty infiltration was reported and mainly involves paravertebral, gluteal, quadriceps, biceps, semitendinosus, semimembranosus, adductor major, soleus, and gastrocnemius muscles [Díaz-Manera et al 2016].
Other laboratory findings:
- Serum CK concentration is normal or moderately elevated (2-20x upper normal level). Increases in serum CK concentration are more often seen at the beginning of the disease than in later stages [Bonne et al 2000, Bonne et al 2002a].
- Muscle histopathology shows nonspecific myopathic or dystrophic changes, including variation in fiber size, increase in internal nuclei, increase in endomysial connective tissue, and necrotic fibers. Electron microscopy may reveal specific alterations in nuclear architecture [Fidziańska et al 1998, Sabatelli et al 2001, Sewry et al 2001, Fidziańska & Hausmanowa-Petrusewicz 2003, Fidziańska & Glinka 2007]. Inflammatory changes may also be found in LMNA-related myopathies including EDMD [Komaki et al 2011]. Muscle biopsy is now rarely performed for diagnostic purposes because of the lack of specificity of the dystrophic changes observed.
- Immunodetection of emerin. In normal individuals, the protein emerin is ubiquitously expressed on the nuclear membrane. Emerin can be detected by immunofluorescence and/or by western blot in various tissues: exfoliative buccal cells, lymphocytes, lymphoblastoid cell lines, skin biopsy, or muscle biopsy [Manilal et al 1997, Mora et al 1997].
- In individuals with XL-EDMD, emerin is absent in 95% [Yates & Wehnert 1999].
- In female carriers of XL-EDMD, emerin is absent in varying proportions in nuclei, as demonstrated by immunofluorescence. However, western blot is not reliable in carrier detection because it may show either a normal or a reduced amount of emerin, depending on the proportion of nuclei expressing emerin.
- In individuals with AD-EDMD, emerin is normally expressed.
- Immunodetection of FHL1. In controls, the three FHL1 isoforms (A, B, and C) are ubiquitously expressed in the cytoplasm as well as in the nucleus. The isoforms can be detected by immunofluorescence and/or western blot in fresh muscle biopsy or myoblasts, fibroblasts, and cardiomyocytes [Sheikh et al 2008, Gueneau et al 2009].
- In individuals with FHL1-related XL-EDMD, FHL1 is absent or significantly decreased [Gueneau et al 2009].
- In female carriers of FHL1-related XL-EDMD, FHL1 is expected to be variably expressed.
- Immunodetection of lamins A/C. Lamins A/C are expressed at the nuclear rim (i.e., nuclear membrane) and within the nucleoplasm (i.e., nuclear matrix). Depending on the antibody used, lamins A/C can be localized to both the nuclear membrane and matrix or to the nuclear matrix only. However, this test is not reliable for confirmation of the diagnosis of AD-EDMD because in AD-EDMD lamins A/C are always present due to expression of the wild type allele at the nuclear membrane and in the nuclear matrix. Western blot analysis for lamin A/C may contribute to the diagnosis, but yields normal results in many affected individuals [Menezes et al 2012].
Variability. Age of onset, severity, and progression of the muscle and cardiac involvement demonstrate both inter- and intrafamilial variability [Mercuri et al 2000, Mercuri et al 2004, Carboni et al 2010]. Clinical variability ranges from early and severe presentation in childhood to late onset and a slowly progressive course. In general, joint contractures appear during the first two decades, followed by muscle weakness and wasting. In a large published series of affected individuals, Astejada et al [2007] found a range of onset of 10.1 ± 9.5 and 3.3 ± 2.9 years respectively in 20 individuals with pathogenic variants in EMD and 27 individuals with pathogenic variants in LMNA.
Progression. Cardiac involvement usually arises after the second decade of life. Respiratory function can be impaired in some individuals [Emery 2000, Mercuri et al 2000, Talkop et al 2002, Mercuri et al 2004, Ben Yaou et al 2007, Gueneau et al 2009]. On occasion, sudden cardiac death is the first manifestation of the disorder [Bécane et al 2000, Kärkkäinen et al 2004, De Backer et al 2010].
AR-EDMD
Nine individuals with genetically confirmed isolated autosomal recessive EDMD (i.e., homozygous or compound heterozygous for a LMNA pathogenic variant) have been reported [Raffaele Di Barletta et al 2000, Brown et al 2001, Vytopil et al 2002, Mittelbronn et al 2006, Scharner et al 2011, Jimenez-Escrig et al 2012, Sframeli et al 2017] (see Table 2). When reported, heterozygous relatives were asymptomatic.
Table 2.
Clinical Characteristics in Ten Reported Individuals with Biallelic LMNA Pathogenic Variants
| Reference | # of Reported Individuals | Onset | Last Muscular Assessment | Heart Involvement | ||
|---|---|---|---|---|---|---|
| Age | Symptoms | Age | Findings | |||
| Raffaele Di Barletta et al [2000] | 1 | 14 mos | Walking difficulties | 40 yrs | Initial wheelchair use at age 4 yrs; severe & diffuse muscle wasting, wheelchair bound | None |
| Brown et al [2001] | 1 | 3 yrs | Not reported | 12 yrs | Proximal upper & distal lower limb weakness; ankle, elbow, & knee contractures | None |
| Vytopil et al [2002] | 1 | Childhood | Stumbled frequently; slower than peers | 16 yrs | Head flexion & scapulo-humero-peroneal weakness; stiff neck; ankle, hip, & elbow contractures | Polymorphic ventricular premature beats; salvos of atrial premature beats |
| Scharner et al [2011] | 1 | <1 yr | Not reported | 6 yrs | Proximal upper & limb-girdle weakness; stiff neck; elbow, ankle, & knee contractures | Cardiomyopathy from age 3 yrs |
| Jimenez-Escrig et al [2012] | 4 | 14 yrs | Difficulty in running | 50 yrs | Initial wheelchair use at age 35 yrs; stiff neck; ankle & elbow contractures | Supraventricular premature beats |
| 12 yrs | Clumsy gait | 46 yrs | Still ambulant; elbow & ankle contractures | Supraventricular & ventricular premature beats | ||
| 4 yrs | Difficulty rising from the floor | 43 yrs | Wheelchair use at age 25 yrs; elbow, hip, & ankle contractures | Supraventricular & ventricular premature beats | ||
| 3rd decade | Not reported | 41 yrs | Still ambulant w/cane; lower- & upper-limb proximal weakness; no contractures | Supraventricular premature beats | ||
| Sframeli et al [2017] | 1 | Early childhood | Mobility difficulties | Child | Upper- & lower-limb weakness; elbow & ankle contractures | None |
Genotype-Phenotype Correlations
EMD. Intra- and interfamilial variability in the severity of clinical features are observed. However,
- Null variants, the majority of EMD pathogenic variants that result in complete absence of emerin expression, tend to have a more severe phenotype [Muntoni et al 1998, Hoeltzenbein et al 1999, Canki-Klain et al 2000, Ellis et al 2000].
- Missense variants associated with decreased or normal amounts of emerin and result in a milder phenotype [Yates et al 1999].
LMNA. Marked intra- and interfamilial variability is observed for the same LMNA pathogenic variant [Bécane et al 2000, Bonne et al 2000, Mercuri et al 2005, Carboni et al 2010]. For example, within the same family the same pathogenic variant can lead to AD-EDMD, LGMD1B, or isolated DCM-CD (i.e., laminopathies involving striated muscle) [Bécane et al 2000, Brodsky et al 2000, Granger et al 2011]. However,
- Missense variants have been associated with early skeletal muscle involvement and joint contractures (i.e., EDMD type) while frameshift variants have been associated with later-onset muscle symptoms of limb girdle type [Benedetti et al 2007].
- Homozygous and compound heterozygous pathogenic variants appear to lead to a more severe muscular phenotype [Raffaele Di Barletta et al 2000, Brown et al 2001, Scharner et al 2011, Jimenez-Escrig et al 2012].
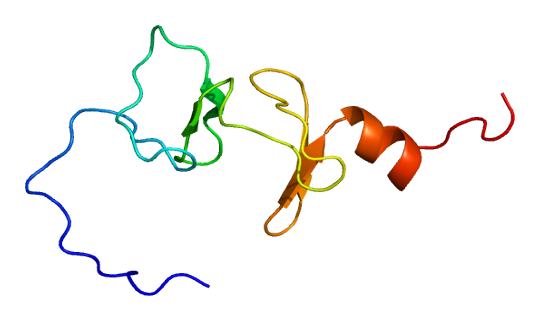
- Pathogenic variants destabilizing the 3D structure of the C-terminal domain of lamin A/C lead to EDMD [Krimm et al 2002].
EMD and LMNA. Severe EDMD has been reported in individuals with pathogenic variants in both EMD and LMNA [Muntoni et al 2006, Meinke et al 2011]. A range of clinical presentations (i.e., CMT2, CMT2-EDMD, and isolated cardiomyopathy) were found in a large family in which pathogenic variants in EMD and LMNA cosegregate [Ben Yaou et al 2007, Meinke et al 2011].
FHL. No definite genotype-phenotype correlations for FHL1 have been identified.
Penetrance
Five LMNA pathogenic variants were reported with reduced penetrance in families with AD-EDMD or other LMNA-related disorders [Vytopil et al 2002, Rankin et al 2008].
Prevalence
The prevalence of XL-EDMD has been estimated at 0.13:100,000-0.2:100,000 [Norwood et al 2009]. This form of EDMD accounts for approximately 10% of the total cases of EDMD (see Table 1). Therefore, the prevalence of EDMD of all types is estimated to be 1.3:100,000-2:100,000.
Differential Diagnosis
Some neuromuscular disorders result in a similar pattern of muscle involvement, joint contractures, or cardiac disease, but most do not feature the complete triad observed in Emery-Dreifuss muscular dystrophy (EDMD).
Table 3.
Disorders to Consider in the Differential Diagnosis of Emery-Dreifuss Muscular Dystrophy
| Disorder Name | Gene(s) | MOI 1 | Clinical Findings | |||
|---|---|---|---|---|---|---|
| Muscle involvement | Joint contractures | Cardiac disease | Distinguishing feature(s) | |||
| Facioscapulohumeral muscular dystrophy | DNMT3B DUX4L1 SMCHD1 | AD | +++ (scapulo-peroneal) | – | – | No joint contractures or cardiac disease |
| Other scapuloperoneal syndromes (neurogenic & myopathic types) (OMIM 181400, 181405, 181430, 608358, 255160) | DES MYH7 TRPV4 | AD AR | +++ | – (DES, MYH) | ++ (DES, MYH) |
|
| SYNE1-related disorders (OMIM 612998) | SYNE1 | AD | ± | ++ | ± | Unavailable (pending description of clear phenotype) |
| SYNE2-related disorders (OMIM 612999) | SYNE2 | |||||