Autosomal Erythropoietic Protoporphyria
Erythropoietic protoporphyria (EPP) is an inherited disorder of the heme metabolic pathway characterized by accumulation of protoporphyrin in blood, erythrocytes and tissues, and cutaneous manifestations of photosensitivity.
Epidemiology
EPP has been reported worldwide, with prevalence ranging between 1/75,000 and 1/200,000.
Clinical description
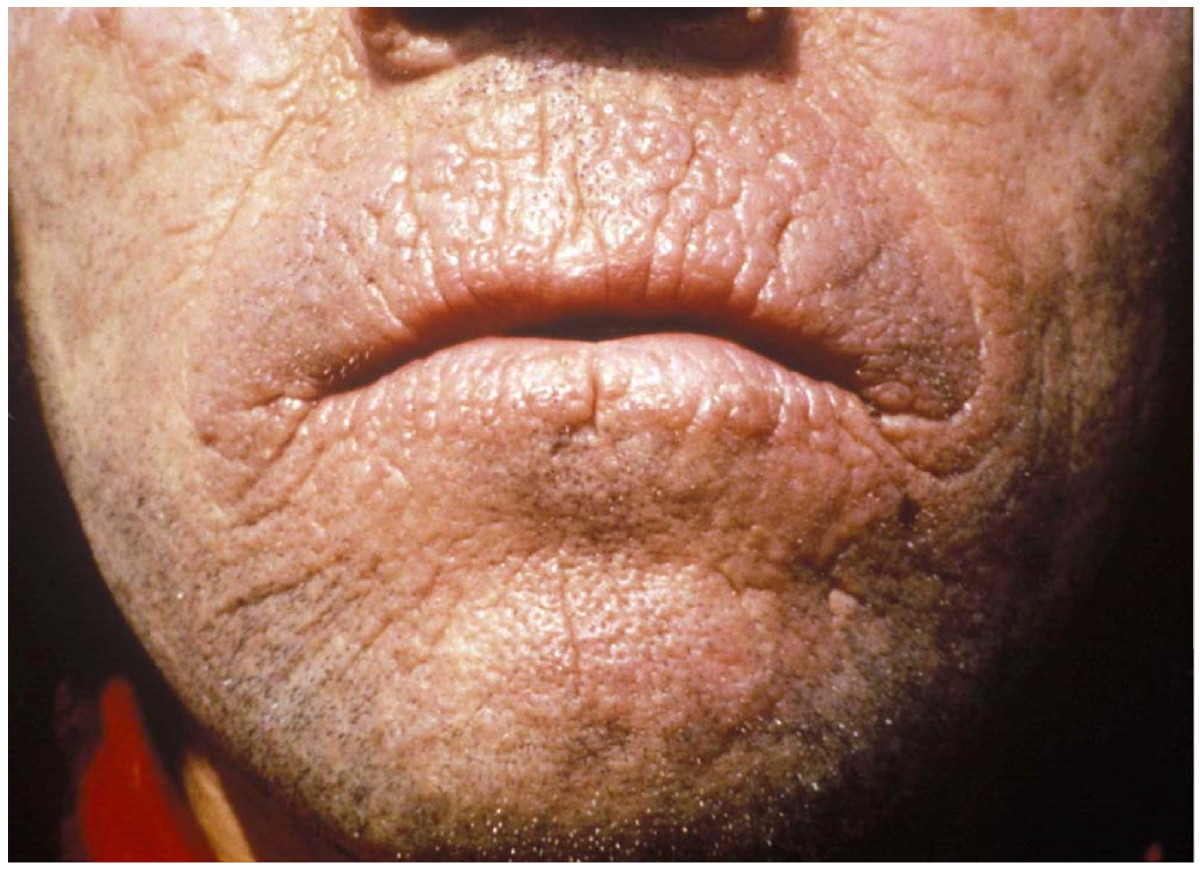
EPP usually manifests in early infancy upon the first exposure to sun. EPP is characterized by cutaneous manifestations of acute painful photosensitivity with erythema and edema, sometimes with petechiae, together with stinging and burning sensations without blistering, upon exposure to sunlight or artificial light (400-700 nm). These episodes have a variable severity depending on the exposure duration and may result in chronic permanent lesions on exposed skin. As protoporphyrin is a lipophilic molecule that is excreted by the liver, EPP patients are at risk of cholelithiasis with obstructive episodes, and chronic liver disease that might evolve to acute liver failure.
Etiology
In most patients, EPP results from a partial deficiency of the last enzyme of the heme biosynthetic pathway, ferrochelatase (encoded by the (FECH gene; 18q21.2-q21.3). EPP appears to be inherited as an autosomal dominant disease, the clinical expression of which is modulated by the presence of the hypomorphic FECH IVS3-48C allele trans, but recessive inheritance with two mutated FECH alleles has also been described. In about 2% of patients, overt disease was recently shown to be caused by gain-of-function mutations in the erythroid-specific aminolevulinic acid synthase 2 (ALAS2; Xp11.21) gene and named X-linked dominant protoporphyria.
Diagnostic methods
Diagnosis is established by finding increased levels of protoporphyrin in plasma and red blood cells, and detection of a plasma fluorescence peak at 634 nm. Investigations for hepatic involvement, ferrochelatase activity level, genetic analysis (FECH mutations, presence of the hypomorphic FECH IVS3-48C allele trans and ALAS2 mutations) and family studies are advisable.
Differential diagnosis
Differential diagnosis includes phototoxic drug reactions, hydroa vacciniforme, solar urticaria, contact dermatitis, angioedema and, in some cases, other types of porphyria (see these terms).
Management and treatment
Management includes avoidance of exposure to light and protection against visible light using sunscreen with a high UVA index and a high critical wavelength (>370 nm), reduction of protoporphyrin levels (either through reduction of erythropoiesis by transfusion or administration of the bile sequestering agent cholestyramine) and prevention of progression of possible liver disease to liver failure. As the major risk in EPP patients is liver disease, a regular follow-up of hepatic involvement is essential. Sequential hepatic and bone marrow transplantation should be considered as a suitable treatment for the most severe cases of EPP with hepatic involvement.
Prognosis
EPP is a lifelong disorder for which the prognosis depends on the evolution of the hepatic disease. However, photosensitivity may have a significant impact on quality of life of EPP patients.