Granulomatous Disease, Chronic, Autosomal Recessive, Cytochrome B-Negative
A number sign (#) is used with this entry because autosomal recessive cytochrome b-negative chronic granulomatous disease (CGD4) is caused by mutation in the gene encoding p22-phox (CYBA; 608508).
For a detailed phenotypic description of chronic granulomatous disease, see X-linked cytochrome b-negative CGD (306400). See also autosomal recessive cytochrome b-positive CGD, types I (233700) II (608515), and III (613960).
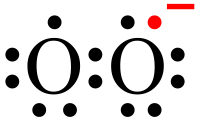
DescriptionChronic granulomatous disease is a genetically heterogeneous immunodeficiency disorder resulting from an inability of phagocytes to kill microbes that they have ingested. This impairment in killing is caused by any of several defects in the NADPH oxidase enzyme complex which generates the microbicidal 'respiratory burst.'
Clinical FeaturesBaehner and Nathan (1968) observed a 17-year-old female born of first cousins who showed a clinical course and leukocyte behavior in vitro like those in affected males with X-linked CGD. Chromosomes were normal. The nitroblue tetrazolium (NBT) test of leukocytes was normal in all relatives.
Yamada et al. (2000) reported a 33-year-old Japanese woman with cytochrome b-negative CGD who had recurrent pneumonia and osteomyelitis caused by various bacteria and Aspergillus. At the age of 33 years, she had renal insufficiency as a result of the nephrotoxic side effects of antifungal drugs and was being treated with hemodialysis. Her parents were related.
Stasia et al. (2002) reported a 5-year-old girl who presented with recurrent bacterial infections and mycosis since the first month of life. The parents were unrelated but lived in a small isolated village in which autarky was said to have existed for several generations.
Teimourian et al. (2008) reported 8 patients from 7 unrelated consanguineous Iranian families with cytochrome b-negative CGD. Patients had a clinical history of recurrent severe infections, including pneumonia, lymphadenitis, liver abscesses, and pyodermatitis. Four of the patients presented before 1 year of age. Genetic analysis identified homozygous mutation or deletion of the CYBA gene (see, e.g., 608508.0012) in all patients.
Biochemical FeaturesBy somatic cell hybridization, Weening et al. (1985) demonstrated an autosomal form of CGD in which cytochrome b was diminished. Among the children of first-cousin parents, 2 sisters and a brother had CGD with granulocytes that did not respond with a metabolic burst to various stimuli and did not kill catalase-positive microorganisms. The magnitude of the cytochrome b signal in the optical spectrum of these leukocytes was less than 4% of normal; the amount of covalently bound flavin was normal. Autosomal recessive inheritance was confirmed; the granulocytes of both parents showed intermediate levels of cytochrome b signal, low-normal or subnormal oxidative reactions during stimulation, and no mosaicism in the stimulated NBT slide test. When monocytes from these patients were fused either with monocytes from a male with X-linked cytochrome b-negative CGD or with monocytes from a male with autosomal cytochrome b-positive CGD, the hybrid cells showed NBT reductase activity after stimulation with PMA. This complementation required protein synthesis. Weening et al. (1985) concluded that the expression of cytochrome b in human phagocytes is coded by at least 2 loci, one autosomal and one X-linked.
Parkos et al. (1989) found that neither cytochrome b subunit, p22-phox or p91-phox (300481), could be detected in neutrophils from 3 patients with X-linked cytochrome b-negative CGD or in 4 patients with autosomal cytochrome b-negative CGD. The authors concluded that the stable expression of either of the 2 subunits is dependent upon the other.
Clinical ManagementLiese et al. (2000) evaluated the effect of antibiotic and antifungal long-term prophylaxis on the prognosis of CGD in 39 patients with different subtypes, both X-linked and autosomal recessive. Antibiotic prophylaxis with TMP-SMX significantly decreased the incidence of severe infections in patients with complete loss of cytochrome b activity but had no significant effect in patients with the other subtypes. Eight of the patients with complete absence of cytochrome b activity were also given itraconazole, and none developed fungal infections over 15.5 patient-years, whereas patients of all subtypes who received only antibiotics showed an increase in severe fungal infections. The different subtypes were also analyzed for age at diagnosis, age at first infection, and long-term survival.
Molecular GeneticsClark et al. (1989) concluded that the form of CGD caused by mutation in the CYBA gene represents about 5% of all CGD cases.
In 3 patients with autosomal recessive cytochrome b-negative CGD, Dinauer et al. (1990) identified 4 mutations in the CYBA gene (608508.0001-608508.0004). One of the patients had been described by Baehner and Nathan (1968).
Yamada et al. (2000) performed mutation analysis on 3 female patients with cytochrome b-negative CGD and found 2 novel mutations in the CYBA gene. One patient with the severe phenotype had a homozygous nonsense mutation in exon 1 (608508.0009); the other 2 patients with mild phenotypes shared the same homozygous missense mutation in exon 2 (608508.0010). The latter 2 patients, but not the first, were demonstrated to have detectable p22-phox expression and significant granulocyte respiratory burst activity, consistent with the milder phenotype.
In a 5-year-old girl with cytochrome b-negative CGD, Stasia et al. (2002) identified a mutation in the CYBA gene (608508.0011).
Animal ModelNakano et al. (2008) found that induced-mutant nmf333 mice were deficient in p22-phox protein due to a tyr121-to-his (Y121H) mutation in the Cyba gene. Homozygous mutant mice showed chronic granulomatous disease characterized by absence of superoxide production in phagocytes and complete absence of NADPH oxidase activity. The mutant mice were highly susceptible to fatal necrotizing B. cepacia pneumonia. In addition, mutant mice showed a severe balance disorder associated with complete absence of otoconia in the utricles and saccules of the inner ear. Transgenic expression of wildtype Cyba rescued both phenotypes. Studies on wildtype mice found Cyba expression in the endolymphatic ducts of the embryonic inner ear, which decreased by postnatal day 12. Based on these findings, Nakano et al. (2008) proposed that NOX activity in the endolymph of the embryonic inner ear regulates local ionic conditions and pH, which may favor the crystallization of calcium carbonate and thereby promote the formation of otoconia. However, the authors noted that balance disorders had not been described in humans with CYBA-associated disease.