Neurocutaneous Melanocytosis
Neurocutaneous melanocytosis (NCM) is a rare congenital neurological disorder characterized by abnormal aggregations of nevomelanocytes within the central nervous system (leptomeningeal melanocytosis) associated with large or giant congenital melanocytic nevi (CMN; see this term). NCM can be asymptomatic or present as variably severe and progressive neurological impairment, sometimes resulting in death.
Epidemiology
Prevalence is estimated at 1/50,000-1/200,000. The incidence of symptomatic NCM appears to be approximately a third to a half of these.
Clinical description
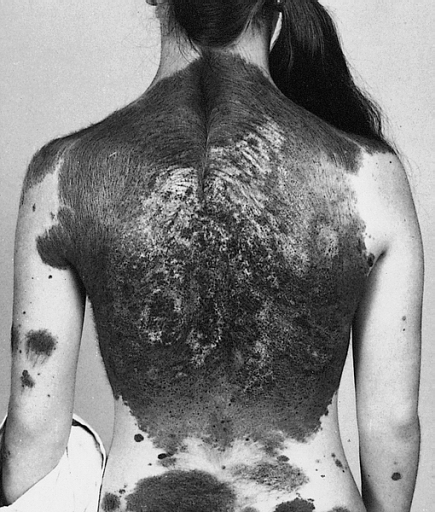
A large, or giant, CMN is a pigmented skin lesion of more than 20 cm projected adult diameter (40 for "giant"), composed of aggregated melanocytes in a delimited area of the body, and presenting with an elevated risk of malignant transformation. Leptomeningeal melanocytosis nearly always presents with CMN, though not conversely; a case with no pigmented lesions and another with only café-au-lait spots have been reported. Symptoms of NCM, when they do occur, generally appear before the age of five and can include headaches, seizures, vomiting, visual disorders, movement and learning disorders, paralysis, intellectual deficit, papilledema, and/or hydrocephalus associated with other brain malformations, such as Dandy-Walker complex. NCM has also been reported with Chiari malformation of the brainstem, congenital heart anomalies (transposition of the great arteries, ventricular septal defect), renal agenesis, skeletal malformations, lipomatosis, or hemihypertrophy.
Etiology
NCM is believed to result from the prenatal, abnormal proliferation of neural crest-derived melanocytes in the central nervous system, but the pathogenic mechanism is still unclear. Their common origin with forebrain-specific pericytes may favor the differentiation and dissemination of nevomelanocytes in situ during meningeal development.
Diagnostic methods
Diagnosis is based on physical examination and neuroimaging. CMN patients with more than twenty CMN or with a large/giant CMN covering the posterior midline axis are more likely to have NCM, though these signs are not in themselves pathognomic. Neuroimaging is based on MRI examination of either symptomatic or asymptomatic NCM, that may reveal areas of increased signal on T1 corresponding to melanocyte aggregation, generally involving the anterior temporal lobes, amygdala, or cerebellum. Biopsy shows variable degrees of differentiation of proliferating nevomelanocytes, ranging from benign-looking cells to atypical melanoma-like cells within the leptomeninges and focally invading the brain.
Differential diagnosis
Differential diagnosis includes primary central nervous system melanoma, meningeal melanocytoma (see these terms), idiopathic hydrocephalus, idiopathic epilepsy, and meningeal melanoma.
Genetic counseling
Only sporadic cases of NCM have been reported to date.
Management and treatment
Close dermatologic and neurologic follow-up for asymptomatic patients is recommended at least annually. In cases with hydrocephalus, ventriculo-peritoneal shunt is generally performed to reduce intracranial pressure with a reported risk of clogging the shunting catheter with the proliferating nevomelanocytes. Seizures have been successfully treated with standard temporal lobotomy.
Prognosis
Asymptomatic NCM shows a normal life expectancy. Symptomatic NCM has a poor prognosis in retrospective studies, though this can be extremely variable (from weeks to months). Death can result from complications of hydrocephalus or from the development of melanocytoma or CNS melanoma.