Acute Promyelocytic Leukemia
A number sign (#) is used with this entry because acute promyelocytic leukemia results from translocations that always involve the gene encoding retinoic acid receptor-alpha (RARA; 180240).
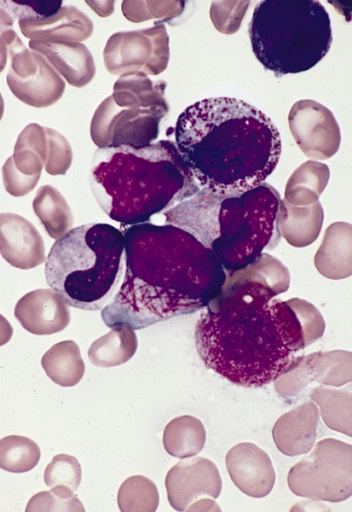
DescriptionAcute promyelocytic leukemia (APL) is associated with 2 cardinal features: a granulocytic differentiation block and reciprocal and balanced translocations that always involve rearrangement of the RARA gene (180240). The most frequent translocation is t(15,17)(q21;q22), which fuses the RARA gene with the PML gene (102578) and represents more than 98% of APL (Vitoux et al., 2007).
CytogeneticsRARA/PML Fusion Gene
APL, also known as acute myeloid leukemia-3, AML3, or M3 in the French-American-British (FAB) classification, is characterized by a predominance of malignant promyelocytes that carry a reciprocal translocation between the long arms of chromosomes 15 and 17: t(15;17)(q22;q11.2-q12). This translocation is diagnostic for APL, as it is present in almost 100% of cases. Borrow et al. (1990) used a NotI linking clone to detect this translocation on pulsed field gel electrophoresis and subsequently with conventional Southern analysis. The breakpoints in 10 APL cases examined were shown to cluster in a 12-kb region of chromosome 17, which contained 2 CpG-rich islands. A comparison of the sequence of cDNA clones from the region of the breakpoint was compared with the EMBL database revealed that the cDNA was that of RARA, which maps to 17q21.1, distal to the APL breakpoint region. They concluded that the cDNAs lay outside the 12-kb breakpoint region and that all of the 15q+ APL breakpoints lie in the first intron of RARA. Since RARA is interrupted in an intron, it is most likely that the product of the translocation is a fusion protein. Borrow et al. (1990) suggested that the chimeric fusion protein encoded by the 15q+ derivative would retain the DNA- and ligand-binding domains of RARA, whereas the transcription-activating function of the 5-prime end of RARA would be replaced with a novel N terminus, potentially changing the profile of genes activated. The involvement of RARA at the APL breakpoint may explain why the use of retinoic acid as a therapeutic differentiation agent in the treatment of acute myeloid leukemias is limited to APL. Lemons et al. (1990) also cloned the APL breakpoint region.
Because RARA maps close to the breakpoint of the t(15;17) translocation specifically associated with acute promyelocytic leukemia, and because retinoic acid has the ability to induce in vivo differentiation of APL cells into mature granulocytes, de The et al. (1990) analyzed the RARA gene structure and expression in APL cells. In one APL-derived cell line, they found that the RARA gene had been translocated to a locus, MYL (PML; 102578), on chromosome 15, resulting in the synthesis of an MYL/RARA fusion mRNA. Using 2 probes located on either side of the cloned breakpoint, they found genomic rearrangements of one or the other locus in 6 of 8 patients, demonstrating that the RARA and/or MYL genes are frequently rearranged in APL and that the breakpoints are clustered. The findings strongly implicated RARA in leukemogenesis.
Hiorns et al. (1994) showed that APL patients with cytogenetically normal chromosomes 15 and 17 may nevertheless have involvement of both PML and RARA genes. Thus there is a subgroup of APL, t(15;17)-negative/PML-RARA-positive, that is analogous to Philadelphia chromosome-negative/BCR-ABL-positive chronic myelogenous leukemia (CML; 608232). The amount of chromosome 17 material inserted into chromosome 15 in the case studied by Hiorns et al. (1994) was too small to be detected cytogenetically. In cases of Philadelphia chromosome-negative/BCR-ABL-positive CML, the amount of DNA transferred can be substantial (Rassool et al., 1990).
RARA/PLZF Fusion Gene
Chen et al. (1993) reported studies of a Chinese patient with APL and a variant translocation t(11;17)(q23;21) in which a gene on 11q23.1, designated PLZF (176797), was fused to the RARA gene on chromosome 17. Fluorescence in situ hybridization using a PLZF-specific probe localized the PLZF gene to chromosome 11q23.1. Similar to t(15;17) APL, all-trans retinoic acid treatment produced an early leukocytosis that was followed by a myeloid maturation, but the patient died too early to achieve remission.
RARA/NUMA1 Fusion Gene
Wells et al. (1997) characterized a novel APL gene fusion that linked exons encoding the retinoic acid and DNA-binding domains of RARA to 5-prime exons of NUMA1 (164009). The NUMA/RARA fusion protein existed in sheet-like nuclear aggregates with which normal NUMA partly colocalized. In contrast to t(15;17) APL, the intracellular distribution of PML was normal in these cells. Wells et al. (1997) suggested that interference with retinoid signaling, and not disruption of PML organization, is essential to the APL phenotype. Their work implicated for the first time an element of the mitotic apparatus in the molecular pathogenesis of human malignancy. The proband of their study was a Caucasian male first seen at 6 months of age for investigation of multiple cutaneous lesions. Despite this unusual clinical presentation, peripheral blood morphology and cell-surface immunophenotype were typical of APL. Routine analysis of diagnostic bone marrow revealed a clonal cytogenetic abnormality, t(11;17)(q13;q21). The patient was treated with all-trans retinoic acid and achieved complete remission; he remained in morphologic remission 38 months after autologous bone marrow transplantation.
RARA/PRKAR1A Fusion Gene
Catalano et al. (2007) reported a 66-year-old man with APL but without the classic t(15;17) translocation. FISH and RT-PCR studies identified a RARA/PRKAR1A (188830) fusion gene, possibly resulting from an insertion of RARA distal to PRKAR1A on chromosome 17q24, followed by a deletion of 3-prime PRKAR1A, 5-prime RARA, and any intervening sequences. The fusion transcript resulted from cryptic splicing of the first 100 bases of PRKAR1A exon 3 to RARA exon 3, and predicted a 495-amino acid fusion protein. The C-terminal end of RARA involved is that shared by all RARA rearrangements in APL. The patient had a good response to chemotherapy with complete remission of the disease by 11 months.
NUP98/RARG Fusion Gene
Such et al. (2011) identified a NUP98 (601021)/RARG (180190) fusion gene resulting from a t(11;12)(p15;p13) translocation in bone marrow cells derived from a 35-year-old man with AML that had morphologic and immunophenotypic features of the hypergranular subtype of acute promyelocytic leukemia. Sequence analysis determined that NUP98 exon 12 was fused in-frame to RARG exon 4, predicted to encode an 862-residue protein with aberrant RARG receptor function. The patient was treated with standard chemotherapy and bone marrow transplantation; response to ATRA was not assessed.
PathogenesisFor information on RARA fusion proteins, including their roles in APL pathogenesis, see 180240.
Pandolfi (2001) reviewed the roles of the RAR-alpha and PML (102578) genes in the pathogenesis of APL.
Zelent et al. (2001) reviewed the functions of the proteins encoded by the different RAR-alpha partner genes found in association with APL, and the implications that these may have for the molecular pathogenesis of APL. The 5 genes reviewed were PML (102578), PLZF (176797), NPM (164040), NUMA1 (164009), and STAT5B (604260).
Vitoux et al. (2007) reviewed pathogenesis and treatment response in APL.
Clinical ManagementLo Coco et al. (1999) reviewed genetic diagnosis and molecular monitoring in the management of APL. Despite its well-recognized sensitivity to anthracyclines as chemotherapeutic agents, APL was, until the late 1980s, one of the most rapidly fatal human tumors, with most patients dying early of intractable hemorrhage or disease with relapse. The cloning of the t(15;17) fusion gene (RARA/PML) and the advent of differentiation therapy with all-trans retinoic acid (ATRA) paved the way for the design of better diagnostic strategies and tailored treatment of the disease. Together with a better control of the coagulopathy, combined ATRA and anthracycline chemotherapy resulted in long-term survival and potential cure in nearly 70% of patients.
Animal ModelFor information on animal models of APL, particularly transgenic mice expressing RARA fusion genes, see 180240.