Congenital Rubella Syndrome
An infectious embryofetopathy that may present in an infant as a result of maternal infection early in pregnancy and subsequent fetal infection with rubella virus. The disorder can lead to deafness, cataract, and variety of other permanent manifestations including cardiac and neurological defects.
Epidemiology
Congenital rubella syndrome (CRS) has been reported to affect an estimated 100,000 infants each year, mainly in developing countries.
Clinical description
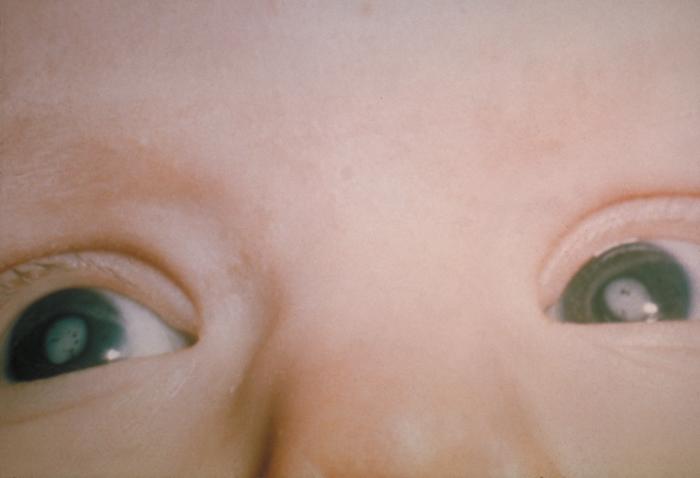
Acquired during the first 8-12 weeks of gestation, rubella infection may cause multiple fetal defects (up to 90% of cases) including neurological (microcephaly), ophthalmic (cataracts, microphthalmia, glaucoma, pigmentary retinopathy, chorioretinitis), auditory (sensorineural deafness), cardiac (peripheral pulmonary artery stenosis, patent ductus arteriosus or ventricular septal defects, etc) defects and fetal wastage or stillbirth. Infection occurring later in gestation is associated with a decline in the risk of birth defects. Fetal defects are rarely associated with maternal rubella occurring after the 14th week of pregnancy, although sensorineural hearing deficit can occur with infection as late as week 20. Additional findings may include: meningoencephalitis, interstitial pneumonitis hepatitis with jaundice (within 24 hours after birth), hepatosplenomegaly, purpura, squint, congenital glaucoma and developmental delay. Infants with congenitally acquired infection may develop manifestations of late-onset disease in later childhood or as adults. Endocrine organs, eyes, hearing and central nervous system may be affected and autoimmune disorders and/or behavioral problems may occur.
Etiology
In pregnant women the virus infects the placenta and the developing fetus. Infants with CRS may excrete the virus for a year or more in pharyngeal secretions and urine.
Diagnostic methods
In the prenatal period, ultrasound examination may fail to diagnose CRS but molecular analysis performed on amniotic fluid (collected at least 6 weeks after maternal infection and after 21 weeks of gestation) will confirm or infirm congenital infection. World Health Organization has established diagnostic criteria. In the postnatal period, its classic triad of clinical signs may suspect CRS: cataract, heart disease, and deafness and confirmed by positive Rubella specific IgM in the newborn.
Differential diagnosis
Differential diagnosis of maternal rubella includes all infections responsible of maculo-papular rash (parvovirus B19, measles, streptococcus A, enteroviruses, cytomegalovirus (CMV), Epstein-Barr virus, human immunodeficiency virus) and other rashes from non infectious causes. Differential diagnosis of congenital rubella includes congenital infection with Toxoplasma gondii, enteroviruses, CMV, Herpes simplex virus, Varicella, Syphilis.
Management and treatment
To date, no treatment for rubella or CRS is available. In order to prevent CRS, vaccination of adolescent girls and women of childbearing age is recommended.
Prognosis
Prognosis of rubella congenital infection mainly depends on the term at maternal infection. Infected children surviving the neonatal period may face serious developmental disabilities (for example, visual and hearing impairments) and have an increased risk for developmental delay, including autism, type I diabetes mellitus and thyroiditis. A progressive encephalopathy resembling subacute sclerosing leukoencephalitis has been observed in patients with CRS.