Pfeiffer Syndrome
An acrocephalosyndactyly associated with craniosynostosis, midfacial hypoplasia, hand and foot malformation with a wide range of clinical expression and severity. Most of the affected patients show various other associated manifestations.
Epidemiology
Pfeiffer syndrome (PS) birth prevalence is 1/100,000. The disorder affects males and females equally.
Clinical description
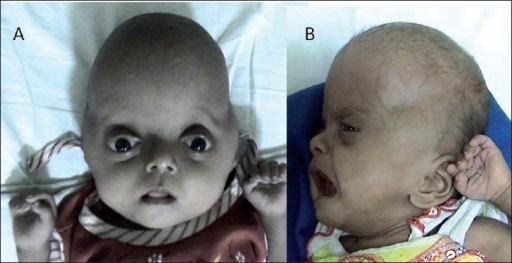
Abnormal skull shape is usually detected in the neonatal period (possibly on prenatal ultrasound). Characteristic cranial features include a wide cranial vault, a flat occiput, broad forehead, a small nose with depressed nasal bridge, orbital hypertelorism and proptosis. The clinical picture depends on the extent craniosynostosis (mostly bicoronal) and the associated functional disorders (respiratory, otological, ocular, neurological). Three forms of PS have been described (PS type 1, type 2, and type 3). Type 1 described as the "classic PD", is the less severe form of PS and is characterized by mild-to-moderate midface hypoplasia, minimal hand and foot abnormalities, little to no ocular proptosis and usually normal intellectual development. In contrast, types 2 and 3 are associated with more severe manifestations such as extreme proptosis and choanal stenosis or atresia, finger and toes abnormalities, elbow ankylosis or synostosis and complications (hydrocephalus and seizures) resulting in a poorer prognosis. Other complications include brain development disorders, exposure keratopathy, exorbitism, bilateral and symmetrical hearing loss, airway obstruction, and obstructive sleep apnea. Type 2, the most severe form, is distinguished form type 3 by the presence of kleeblattschädel, commonly referred to as trilobated or ''cloverleaf'' skull. Types 2 and 3 have occurred only in sporadic cases and have increased risk of early death due to severe neurological compromise and respiratory problems.
Etiology
The majority of cases are caused by de novo mutations in the FGFR2 gene (10q25.3-q26), and very rarely in type 1 cases, by mutations in the FGFR1 (8p11.23-p11.22) gene. Patients meeting criteria for a clinical diagnosis of Pfeiffer syndrome without a mutation in FGFR1 or FGFR2 are estimated to be as high as 21%. Spontaneous mutations have been associated with advanced paternal age.
Diagnostic methods
The diagnosis is based on the presence of the characteristic clinical findings including craniosynostosis or cloverleaf skull, facial features, and variable hand and foot malformations. Diagnosis can be confirmed by molecular genetic testing.
Differential diagnosis
Differential diagnoses include other acrocephalosyndactyly syndromes (Apert, Crouzon, Carpenter, Saethre-Chotzen, Waardenburg) and other syndromic forms of craniosynostosis such as Jackson-Weiss, Muenke and Antley-Bixler syndromes and Cutis gyrata-acanthosis nigricans-craniosynostosis.
Antenatal diagnosis
Prenatal molecular genetic testing is possible. Results of genetic testing for low-risk pregnancies are of little prognostic value. Prenatal imaging may also be used for diagnosis if physical findings are apparent. Some ultrasound findings could pose the suspicion of the disease.
Genetic counseling
Genetic counseling should be provided to affected families. Inheritance from an affected parent in an autosomal dominant manner is reported in less severe cases of Pfeiffer syndrome. PS shows complete penetrance, although the expressivity is variable. Genetic counseling should be proposed to individuals having the disease-causing mutation informing them that there is 50% risk of passing the mutation to offspring. When prenatal features are evocative for PS, gene molecular testing for mutation, after standard and molecular karyotyping should be suggested.
Management and treatment
Treatment is symptomatic and corrective, depending on the extent of disease manifestations. A multidisciplinary approach should be adopted to plan multiple-stage surgical interventions and other treatments with the aim of improving cosmetics, function and quality of life. The psychosocial aspects of the disease should also be addressed.
Prognosis
The success of timely treatment is the main prognostic factor. Favorable outcomes can be achieved but the prognosis remains poor in severe cases with a high risk of early demise due to respiratory and neurological complications.