Epilepsy, Focal, With Speech Disorder And With Or Without Mental Retardation
A number sign (#) is used with this entry because focal epilepsy and speech disorder (FESD) with or without mental retardation is caused by heterozygous mutation in the GRIN2A gene (138253) on chromosome 16p13.
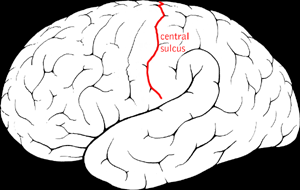
DescriptionFocal epilepsy with speech disorder is a childhood-onset seizure disorder with a highly variable phenotype. Seizures typically occur in the temporal lobe, or rolandic brain region, which affects speech and language, and electroencephalogram (EEG) characteristically shows centrotemporal spike-wave discharges. EEG abnormalities often occur during sleep and may manifest as continuous spike-wave discharges during slow-wave sleep (CSWS or CSWSS). FESD represents an electroclinical spectrum that ranges from severe early-onset seizures associated with delayed psychomotor development, persistent speech difficulties, and mental retardation to a more benign entity characterized by childhood onset of mild or asymptomatic seizures associated with transient speech difficulties followed by remission of seizures in adolescence and normal psychomotor development. There is incomplete penetrance and intrafamilial variability, even among family members who carry the same GRIN2A mutation (summary by Lesca et al., 2013; Lemke et al., 2013; Carvill et al., 2013).
The disorder represented here encompasses several clinical entities, including Landau-Kleffner syndrome (LKS), epileptic encephalopathy with continuous spike and wave during slow-wave sleep (ECSWS; CSWSS), autosomal dominant rolandic epilepsy, mental retardation, and speech dyspraxia (ADRESD; RESDAD), and benign epilepsy with centrotemporal spikes (BECTS; see 117100). LKS is classically described as a childhood-onset variant of epileptic aphasia. It is associated with EEG abnormalities occurring in the temporal lobe of the language-dominant hemisphere, even in the absence of overt clinical seizures. LKS is sometimes referred to as an 'acquired aphasia' because most affected children show normal psychomotor development until the onset of seizures, usually between 3 and 7 years, although some may have prior delayed development. A hallmark of the disorder is severe impairment in auditory language comprehension and speech. Some patients may also have persistent intellectual disability or behavioral abnormalities reminiscent of autism or attention deficit-hyperactivity disorder. EEG abnormalities typically include centrotemporal spikes suggestive of rolandic epilepsy or continuous spike and waves during slow-wave sleep. The presence of CSWS is associated with more widespread behavioral and cognitive regression than LKS, although the 2 disorders may be considered part of a spectrum. There is controversy about the precise definition of LKS and its relationship to CSWS that stems mainly from the phenotypic heterogeneity of the disorder (summary by Stefanatos, 2011).
Clinical FeaturesLandau and Kleffner (1957) described 6 children with acquired aphasia and convulsive disorder. Ansink et al. (1989) found reports of more than 170 children with this condition. Characteristically, Landau-Kleffner syndrome (LKS) affects previously normal children who undergo a regression of receptive and/or expressive language abilities. The regression may be sudden or insidious and is not accompanied by any abnormal neurologic signs, impairment of hearing, or loss of cognitive ability. Males are more frequently affected than females by a ratio of 2:1; most children develop behavioral disturbances. It appears that the younger the child at the onset, the worse the prognosis is for eventual recovery. Some children are left with such severe auditory agnosia that they are unable to identify environmental sounds, such as a dog barking or a bird calling. In contrast, others recover completely, even after several episodes of aphasia. About one-half of patients are left with severe residual language deficits. The seizures are usually easily controlled by pharmacologic means and all children are seizure-free by age 15 years. All children with LKS, regardless of seizures, have abnormalities on EEG. Pairs of affected sibs were reported by Landau and Kleffner (1957) and by Nakano et al. (1989). Feekery et al. (1993) reported monozygotic twins discordant for LKS.
Huppke et al. (2005) reported an isolated case of Landau-Kleffner syndrome in a boy. Speech development was normal until 2.5 years, when he developed dysarthria. At age 3, he began to stutter and intermittently failed to respond to spoken words. Over the following years, he had 2- to 3-week period in which he only used sign language or spoke and reacted to speech normally. At age 6 years, he had a prolonged 2-month phase of no speech or reaction to words. Seizures were never noted. EEG at age 7 years showed bilateral temporal spike-wave discharges, and MRI showed bilateral perisylvian polymicrogyria. Treatment with sulthiame, a central carbonic anhydrase inhibitor, resulted in normalization of his speech behavior and EEG changes. Huppke et al. (2005) noted that most patients with LKS have normal brain imaging studies, but concluded that bilateral perisylvian polymicrogyria was the etiology of LKS in their patient.
Scheffer et al. (1995) described a syndrome of nocturnal partial seizures involving the face and an arm associated with oral dyspraxia and cognitive impairment in a family with 9 affected individuals in 3 generations. Clinically significant cognitive impairment was only obvious in the most recent generation. However, all affected individuals had oromotor apraxia with difficulty organizing and coordinating movements necessary to produce fluent speech but without dysarthria. There were also mild impairments of perceptive language. There were electroencephalographic similarities to benign rolandic epilepsy. The authors suggested that this disorder may be part of a spectrum, the extremes of which are represented by benign rolandic epilepsy, a mild disorder, and the more severe Landau-Kleffner or continuous spike and wave syndromes, which are more severe. Because of more severe impairments in the third generation, the authors suggested possible expansion of a triplet repeat. They further distinguished this disorder from autosomal dominant nocturnal frontal lobe epilepsy (600513) and familial temporal lobe epilepsy (600512). Carvill et al. (2013) reported follow-up of the family reported by Scheffer et al. (1995). Three patients had remission of seizures at age 13 years, whereas 3 had ongoing seizures. All had normal intellect, except for 2 with mild or borderline intellectual disability.
Kugler et al. (2008) reported a 3-generation pedigree in which 12 of 22 individuals were affected with at least 1 of 3 traits, including rolandic epilepsy, cognitive impairment, and a speech/sound disorder. Three illustrative case histories noted asymmetric facial seizures, language delay or speech difficulties with oromotor apraxia, and learning difficulties. Two patients had migraines. Some family members had dysdiadochokinesis, suggesting cerebellar involvement. There was no evidence of anticipation in this family. The inheritance pattern was autosomal dominant. Linkage was excluded from loci on chromosome 11p, 15q14, 16p12, and Xq22. Kugler et al. (2008) noted the phenotypic similarities to the family reported by Scheffer et al. (1995).
Endele et al. (2010) reported a Belgian family with epilepsy and neurodevelopmental defects, manifested as mental retardation or learning difficulties, that was associated with a heterozygous translocation t(16;17)(p13.2;q11.2) disrupting the GRIN2A gene. The proband was a 26-year-old man with a history of febrile seizures followed by tonic-clonic seizures and severe mental retardation. His father, paternal aunt, and cousin all had a history of generalized seizures with onset at the end of their first decade that spontaneously decreased during adolescence. All 4 family members had behavioral problems, and the cousin also had moderate mental retardation. EEG available from 3 of the patients showed bilateral spike-wave bursts with temporal predominance, diffuse slow and rapid dysrhythmia, and triphasic spike-waves with temporal predominance, respectively. Endele et al. (2010) also reported a German family in which a 4-year-old boy had mild to moderate mental retardation and abnormal EEG, but no overt seizures. He also had hypotonia, facial dysmorphism, and microcephaly. His mother had febrile seizures at age 11 months followed by focal seizures until age 3. EEG of the proband and his mother showed centrotemporal spikes, reminiscent of rolandic epilepsy. The maternal grandmother had a history of seizures in the first year of life that disappeared in adolescence. Both the mother and grandmother had learning difficulties. The authors also reported a 3-year-old French girl with severe mental retardation and early-onset epileptic spasms and myoclonic seizures. She also had hypotonia and behavioral abnormalities.
Carvill et al. (2013) reported a father and son with epileptic encephalopathy with continuous spike and wave in slow-wave sleep. The patients had onset of seizures in early childhood, remission of seizures in adolescence, and mild to moderate intellectual disability. Both showed developmental regression after seizure onset. The father had focal dyscognitive and tonic-clonic seizures, whereas the son had rolandic seizures. Both had speech and language difficulties. Carvill et al. (2013) reported another family with an overlapping phenotype. Two sibs were diagnosed with intermediate epilepsy aphasia disorder, and a third with CSWS. Two had mild globally delayed early development with regression and mild intellectual disability, and the third had normal development with mild borderline intellectual disability. All had speech and language difficulties. Their mother had learning difficulties and speech/language disorder. Carvill et al. (2013) also reported 2 sisters with Landau-Kleffner syndrome with onset of seizures in early childhood, mild intellectual disability, and speech and language difficulties. Seizures in 1 sister remitted at age 2.5 years, whereas seizures in the other sister were ongoing at age 7 years. Both had normal early development with regression after seizure onset. EEG in both showed continuous centrotemporal spikes, apparent in sleep in 1 patient.
Lesca et al. (2013) reported a 3-generation French family in which the proband presented with typical LKS. He had onset of nocturnal and partial seizures at age 4 years, delayed language and language regression, mild cognitive impairment during the acute phase, and status epilepticus during slow-wave sleep. He had a favorable neurologic outcome at age 26 years and no autistic features. Family history revealed that several relatives had either atypical rolandic epilepsy or CSWS with onset in early childhood and often associated with impaired speech and developmental regression. EEG was abnormal in all affected family members, showing either centrotemporal spikes or status epilepticus during slow-wave sleep. Eight additional families with LKS, CSWS, or atypical rolandic epilepsy, often associated with verbal dyspraxia, were subsequently identified. Seizure onset occurred between ages 2 and 6 years, and seizure types included nocturnal, partial, complex partial, febrile, and generalized tonic-clonic. Although motor and cognitive regression was common, most patients had a favorable neurologic outcome. Some individuals showed initial developmental delay, presumably before seizure onset. EEG showed centrotemporal spikes and/or status epilepticus during slow-wave sleep. Lesca et al. (2013) also identified 6 unrelated patients with apparently sporadic LKS or CSWS and 1 patient with sporadic atypical rolandic epilepsy. Two had delayed initial development, whereas the others showed regression only after onset of seizures in early childhood. Almost all had mild cognitive impairment, about half had a slow or poor neurologic outcome, and 4 had persistent behavioral abnormalities, including autistic features and attention deficit-hyperactivity disorder. EEG in all showed centrotemporal spikes or ECSWS.
Turner et al. (2015) analyzed the speech phenotype associated with GRIN2A mutations in 11 individuals, aged 16 to 64 years, from 3 families, all of whom had previously been reported (Scheffer et al., 1995; Tsai et al., 2013; Carvill et al., 2013). Affected individuals had dysarthria and vocal dyspraxia with lifelong impact on speech intelligibility in some. Speech was characterized by imprecise articulation (100%), impaired pitch (monopitch, 91%) and prosody (stress errors, 64%), and hypernasality (64%). Other findings included oral motor impairments and poor performance on maximum vowel duration (73%), repetition of monosyllables (91%), and trisyllables (64%). Deficits in language skills were evident before seizure onset in 8 of 10 patients, suggesting that epileptiform abnormalities were not the cause of language impairment. The speech phenotype was also present in 1 individual who did not have seizures, reinforcing an important role for GRIN2A in motor speech function.
CytogeneticsReutlinger et al. (2010) reported 3 unrelated patients with different deletions of chromosome 16p13 including the GRIN2A gene who had early-onset focal epilepsy, severe intellectual disability, and lack of speech or delayed speech development. EEG available from 2 patients showed centrotemporal spikes, reminiscent of rolandic epilepsy, and electrical status epilepticus in sleep (ESES). All showed delayed global development from birth or early infancy. All had variable dysmorphic features, including low-set ears, epicanthal folds, hypertelorism, deep-set eyes, broad nasal tip, short nose, and brachydactyly. Genomewide screening for structural genomic variants identified 3 different deletions, ranging in size from 980 kb to 2.6 Mb, in the 3 patients. Two of the deletions were confirmed to be de novo; parental samples from the third patient were unavailable. The only gene located in the critical shared region of all 3 patients was GRIN2A.
InheritanceThe transmission pattern of FESD in the 3-generation family reported by Kugler et al. (2008) was consistent with autosomal dominant inheritance.
Molecular GeneticsIn a proband, mother, and grandmother from a German family with childhood seizures and variable neurodevelopmental defects ranging from mental retardation to learning difficulties, Endele et al. (2010) identified a heterozygous mutation in the GRIN2A gene (Q218X; 138253.0001), resulting in a loss of function. In a 3-year-old French girl with severe mental retardation, the authors identified a heterozygous de novo mutation (N615K; 138253.0002) in the GRIN2A gene. The N615K-mutant protein was demonstrated to exert a dominant-negative effect, which may have explained the severe phenotype.
Lesca et al. (2013) examined the role of the GRIN2A gene in 66 probands with LKS or CSWS. Heterozygous inherited or de novo mutations (see, e.g., 138253.0008-138253.0010) were found in 7 of 7 families and in 6 of 59 patients with sporadic disease. Segregation studies in the families showed that some mutation carriers had atypical rolandic epilepsy. Two mutation carriers reportedly had benign childhood epilepsy. Most mutation carriers had dysphasia or verbal dyspraxia. Some mutation carriers were unaffected, indicating incomplete penetrance. Heterozygous GRIN2A mutations were subsequently found in 2 families with atypical rolandic epilepsy. One family with a mutation in the SRPX2 gene (300642.0001; Roll et al., 2006; 300643) also carried a heterozygous GRIN2A mutation. In total, 14 point mutations and 2 small deletions involving the GRIN2A gene (15 kb and 75 kb, respectively) were identified. Functional studies showed that 2 of the missense mutations caused a significant increase in the open time and a decrease in the closed time of NMDA channels compared to wildtype, consistent with a modulatory effect on the excitatory postsynaptic current. GRIN2A mutations were located in different domains of the protein, and there were no apparent genotype/phenotype correlations. Lesca et al. (2013) concluded that GRIN2A mutations represent a major genetic determinant of LKS and CSWS, as well as related epileptic disorders in the same clinical continuum, such as atypical rolandic epilepsy and speech impairment.
Lemke et al. (2013) identified heterozygous mutations in the GRIN2A gene (see, e.g., 138253.0005; 138253.0011-138253.0013) in 27 (7.5%) of 359 patients from 2 independent cohorts with idiopathic focal epilepsy syndromes, including Landau-Kleffner syndrome, CSWS, atypical rolandic epilepsy, and benign epilepsy of childhood with centrotemporal spikes (BECTS; 117100). Mutations occurred at a significantly higher frequency in patients compared to the Exome Variant Server (0.6%; p = 4.83 x 10(-18)) or in controls of European ancestry (p = 1.18 x 10(-16)). Mutations occurred significantly more frequently in the more severe phenotypes, with mutation detection rates ranging from 12 (4.9%) of 245 individuals with BECTS to 9 (17.6%) of 51 with LKS/CSWS. Splice site, truncating, and frameshift mutations were more commonly associated with the more severe phenotypes, and missense mutations were more commonly associated with the more benign phenotypes. Segregation status was available for 18 families. The mutations segregated with a phenotype of different epileptic disorders within the families, ranging from BECTS to learning disabilities and intellectual disability to atypical rolandic epilepsy and CSWS; some mutations carriers were unaffected. Exon-disrupting microdeletions of the GRIN2A gene were also found in 3 (1%) of 286 individuals screened for copy number variations. The findings indicated that alterations of the GRIN2A gene are a major genetic risk factor for various types of idiopathic focal epilepsy.
By sequence analysis of the GRIN2A gene in 519 probands with a range of epileptic encephalopathies, Carvill et al. (2013) identified heterozygous mutations in 4 probands, all of whom came from the cohort of 44 patients with epilepsy-aphasia syndromes (9% of probands with epilepsy-aphasia syndromes). One of the probands was from the family reported by Scheffer et al. (1995), and a heterozygous splice site mutation (138253.0005) segregated with the disorder in all 7 patients in this family. Two affected members of an unrelated family with epileptic encephalopathy with continuous spike and wave in slow-wave sleep also carried this mutation. Both were Australian families of European descent, and haplotype analysis indicated a founder effect. Turner et al. (2015) reported that genealogic work indicated that the 2 families with the splice site mutation reported by Scheffer et al. (1995) and Carvill et al. (2013) were in fact related. In 3 sibs from another family with CSWS or intermediate epilepsy-aphasia disorder, Carvill et al. (2013) identified a different heterozygous mutation (138253.0007). The fourth family with a GRIN2A mutation was diagnosed with LKS. The findings indicated that GRIN2A mutations can be associated with a wide range of epilepsy-aphasia spectrum phenotypes. No GRIN2A mutations were found in 475 patients with other epileptic encephalopathy phenotypes or in 81 patients with BECTS.