Hereditary Fructose Intolerance
Summary
Clinical characteristics.
Following dietary exposure to fructose, sucrose, or sorbitol, untreated hereditary fructose intolerance (HFI) is characterized by metabolic disturbances (hypoglycemia, lactic acidemia, hypophosphatemia, hyperuricemia, hypermagnesemia, hyperalaninemia) and clinical findings (nausea, vomiting, and abdominal distress; chronic growth restriction/failure to thrive). Untreated HFI typically first manifests when fructose- and sucrose-containing foods are introduced in the course of weaning young infants from breast milk. If large quantities of fructose are ingested, the infant may acutely develop lethargy, seizures, and/or progressive coma. Untreated HFI may result in renal and hepatic failure. If identified and treated before permanent organ injury occurs, individuals with HFI can experience a normal quality of life and life expectancy.
Diagnosis/testing.
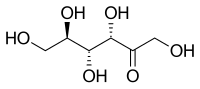
The diagnosis of HFI is established in a proband (with suggestive metabolic disturbances and clinical findings following dietary exposure to fructose, sucrose, or sorbitol) who has demonstrated either biallelic pathogenic variants in ALDOB on molecular genetic testing or deficient hepatic fructose 1-phosphate aldolase (aldolase B) activity on liver biopsy.
Management.
Treatment of manifestations: Acute manifestations (e.g., lethargy, seizures, or progressive coma and/or renal and hepatic failure) should be managed symptomatically in a hospital setting, including intravenous glucose (dextrose) administration, supportive treatment of hepatic insufficiency, and treatment of metabolic acidosis, if present.
Prevention of primary manifestations: Dietary restriction of fructose, sucrose, and sorbitol is the cornerstone of HFI treatment. Specific agents to be avoided include fructose, high-fructose corn syrup, honey, agave syrup, inverted sugar, maple-flavored syrup, molasses, palm or coconut sugar, and sorghum. In addition, medicines and formulas in which fructose/sucrose may not be listed as a primary component need to be avoided; examples include syrups, enema solutions, some immunoglobulin solutions, and many infant and pediatric nutritional drinks. During hospitalizations special caution is advised to avoid use of fructose-containing intravenous fluids.
Prevention of secondary complications: Given that reduced fruit and vegetable intake is a dietary requirement, daily supplementation with a "sugar-free" multivitamin is recommended to prevent micronutrient deficiencies, specifically water-soluble vitamins.
Surveillance: No formal guidelines for surveillance exist. Once the diagnosis of HFI has been made, periodic evaluation of liver function, renal function, and growth is reasonable, particularly if compliance with the fructose/sucrose/sorbitol-restricted diet is not absolute.
Agents/circumstances to avoid:
- Enteral or parenteral exposure to fructose, sorbitol, sucrose, sucralose, and polysorbate.
- Fructose tolerance testing ("fructose challenge") in the diagnosis of HFI.
Evaluation of relatives at risk: Presymptomatic diagnosis and treatment is warranted for sibs at risk in order to avoid life-threatening complications by restriction of fructose intake as soon as possible.
Genetic counseling.
HFI is inherited in an autosomal recessive manner. At conception, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being a carrier, and a 25% chance of being unaffected and not a carrier. Carrier testing for at-risk relatives and prenatal testing for pregnancies at increased risk are possible if both ALDOB pathogenic variants have been identified in an affected family member.
Diagnosis
There are no formal diagnostic guidelines for hereditary fructose intolerance (HFI).
Suggestive Findings
Hereditary fructose intolerance (HFI) should be suspected in individuals with the following characteristic metabolic disturbances and clinical findings following dietary exposure to fructose, sucrose, or sorbitol.
Characteristic metabolic disturbances
- Hypoglycemia (plasma glucose <60 mg/dL; reference range 70-120 mg/dL)
- Lactic acidemia (plasma lactate >2.5 mmol/L; reference range: 0.5-2.2 mmol/L)
- Hypophosphatemia
- Hyperuricemia (plasma uric acid >5.0 mg/dL; reference range 2.0-5.0 mmol/L)
- Hypermagnesemia
- Hyperalaninemia
Characteristic clinical findings
- Nausea, vomiting, and abdominal distress
- Chronic growth restriction/failure to thrive
Establishing the Diagnosis
The diagnosis of HFI is established in a proband with suggestive metabolic disturbances and clinical findings following dietary exposure to fructose, sucrose, or sorbitol who has demonstrated EITHER of the following:
- Biallelic pathogenic variants in ALDOB on molecular genetic testing (Table 1)
- Deficient hepatic fructose 1-phosphate aldolase (aldolase B) activity on liver biopsy
Note: Because of the relatively high sensitivity of ALDOB molecular genetic testing, it is increasingly the preferred confirmatory test for HFI and can obviate the need for liver biopsy.
Molecular testing approaches can include single-gene testing, use of a multigene panel, and more comprehensive genomic testing.
Single-gene-testing
- Sequence analysis is performed first and followed by gene-targeted deletion/duplication analysis if only one or no pathogenic variant is identified.
- Targeted analysis for the following pathogenic variants can be performed first – if appropriate – in individuals with specific ancestry:
- European: p.Ala150Pro and p.Ala175Asp
- Northern Indian: c.324+1G>A
A multigene panel that includes ALDOB and other genes of interest (see Differential Diagnosis) may also be considered. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview; thus, clinicians need to determine which multigene panel is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
More comprehensive genomic testing (when available) including exome sequencing, mitochondrial sequencing, and genome sequencing may be considered if serial single-gene testing (and/or use of a multigene panel that includes ALDOB) fails to confirm a diagnosis in an individual with features of hereditary fructose intolerance. Such testing may provide or suggest a diagnosis not previously considered (e.g., mutation of a different gene that results in a similar clinical presentation).
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 1.
Molecular Genetic Testing Used in Hereditary Fructose Intolerance
| Gene 1 | Method | Proportion of Probands with Pathogenic Variants 2 Detectable by Method |
|---|---|---|
| ALDOB | Sequence analysis 3 | 66%-100% 4 |
| Gene-targeted deletion/duplication analysis 5 | 0%-20% 6, 7, 8 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on allelic variants detected in this gene.
- 3.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 4.
The most commonly identified pathogenic variants in European and North American populations are p.Ala150Pro and p.Ala175Asp. The c.324+1G>A splice variant is common in a population from Northern India [Dursun et al 2001, Sánchez-Gutiérrez et al 2002, Santer et al 2005, Gruchota et al 2006, Davit-Spraul et al 2008, Coffee et al 2010, Ferri et al 2012, Bijarnia-Mahay et al 2015].
- 5.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 6.
Cross & Cox [1990], Santer et al [2005], Davit-Spraul et al [2008], Esposito et al [2010]
- 7.
No large deletions were identified by Southern blotting in 56 individuals from Spain [Sánchez-Gutiérrez et al 2002].
- 8.
A large (6.5-kb) intragenic deletion with an allele frequency of 11% was identified in a small Italian cohort [Ferri et al 2012].
Deficient hepatic fructose 1-phosphate aldolase (aldolase B) activity on liver biopsy. Specific fructose-1-phosphate aldolase B enzyme assays and fructose assay enzyme panels on frozen liver tissue may be important options for the diagnosis in individuals with clinical and biochemical features of HFI in whom sequence analysis has failed to identify biallelic ALDOB pathogenic variants.
Clinical Characteristics
Clinical Description
Hereditary fructose intolerance (HFI) typically manifests when fructose- and sucrose-containing foods are introduced in the course of weaning young infants from breast milk [Ali et al 1998]. Manifestations include nausea, bloating, vomiting, sweating, abdominal pain, and growth retardation [Odièvre et al 1978].
Impaired gluconeogenesis following fructose ingestion may result in acute hypoglycemia that is refractory to glucagon [Van Den Berghe et al 1973]. For example, infants who ingest large quantities of fructose may develop lethargy, seizures, and/or progressive coma, or neonates given a 24% sucrose solution for analgesia during minor procedures may develop hypoglycemia.
Other biochemical features of HFI include hypermagnesemia, hyperuricemia, hypophosphatemia, and metabolic acidosis [Bouteldja & Timson 2010].
Other less common findings in HFI include:
- Lenticular cataracts, intermittent liver enzyme abnormalities, or chronic liver disease of early or late onset [Locher 1987, Krawczyński et al 1994, Wössmann et al 2000, Ananth et al 2003];
- Coagulopathy [Hosková & Mrskos 1977];
- Isolated poor growth [Mock et al 1983];
- Intermittent vomiting in the setting of fructose aversion and pristine dentition [Newbrun et al 1980].
Typically, when complete dietary fructose, sucrose, and sorbitol restriction is implemented early in life and adherence is maintained (see Management, Prevention of Primary Manifestations), the prognosis for individuals with HFI is excellent (i.e., normal neurocognitive development, health, and life expectancy).
Conversely, when individuals with HFI do not adhere to recommended dietary restrictions, chronic liver and/or renal disease are expected; however, long-term natural history studies in untreated individuals are lacking [Odièvre et al 1978]. Of note, historical reports describe adults with HFI who survived following self-imposed low fructose diets that they refined through trial and error.
Of note, dental researchers have conflicting observations about oral health in individuals with HFI: one group observed a lower incidence of dental caries and periodontal disease as a result of self-imposed dietary restrictions of sugar [Marthaler & Froesch 1967], whereas another group speculated that fructose restriction may itself contribute to periodontal disease as oral microbiome changes appeared to increase the risk for gingival bleeding and calculi in treated individuals [Saxén et al 1989].
Heterozygotes (carriers) are not at increased risk of developing HFI. While carriers are generally asymptomatic, in older reports hyperuricemia was observed in some presumed or obligate carriers and, thus, these individuals may be predisposed to gout/crystal arthropathy [Oberhaensli et al 1987, Seegmiller et al 1990].
Genotype-Phenotype Correlations
No genotype-phenotype correlations have been identified for HFI; clinical severity and extent of organ damage appear to depend on an individual's nutritional environment.
Nomenclature
Chambers & Pratt [1956] reported "idiosyncrasy to fructose" in a female age 24 years who developed gastrointestinal symptoms and syncopal symptoms following fructose or sugar ingestion.
"Fructosaemia," a term originally proposed by Levin et al [1963] to describe the presence of abnormal quantities of fructose in plasma, is now considered obsolete. This finding, which is not specific to HFI, is also observed in fructokinase deficiency and other disorders [Hommes 1993].
Prevalence
Hereditary fructose intolerance (HFI) is rare, making precise prevalence estimates challenging.
European estimates for the prevalence (based on results of carrier testing for common ALDOB pathogenic variants and use of the Hardy-Weinberg principle after correction for the estimated detection rate) are between 1:18,000 and 1:31,000 (Table 2).
It is important to note that the US study that targeted five specific ALDOB alleles [Lazarin et al 2013] may underestimate the prevalence in persons of non-European ancestry. Applying a Bayesian framework to population-based genomic data, Schrodi et al [2015] devised posterior probability density prevalence estimates for HFI; based on available data, prevalence of HFI was estimated as 1:34,461 (95% credible interval 1:16,800 to 1:94,500).
Table 2.
HFI Prevalence by Population Based on Carrier Testing for Specific ALDOB Pathogenic Variants
| UK 1 | Germany 2 | Poland 3 | US | ||||
|---|---|---|---|---|---|---|---|
| All 4 | ME 4 | AA 4 | |||||
| Extrapolated HFI prevalence 5 | 1:18,000 | 1:26,000 | 1:31,000 | 1:60,000 | 1:38,000 | 1:205,000 | |
| Variants tested | p.Ala150Pro | X | X | X | X | ||
| p.Ala175Asp | X | X | |||||
| p.Asn335Lys | X | X | |||||
| Other | p.Tyr205Ter, p.Asn120LysfsTer32 | ||||||
AA = African American; ME = Middle Eastern
- 1.
Based on the UK population prevalence of the p.Ala150Pro allele, the final estimate for the incidence of HFI was 1:18,000 live births [James et al 1996]
- 2.
Santer et al [2005]
- 3.
Gruchota et al [2006]
- 4.
In a large carrier screening study of multiple disorders in an ethnically diverse population in the United States, overall carrier frequency for an ALDOB pathogenic variant was 1:122 (~0.8%). Carrier frequencies in persons self-identifying as Middle Eastern (n=388) and African American (n=678) were 1:97 (~1.0%) and 1:226 (~0.4%), respectively. Using the Hardy-Weinberg principle, these data yield disease frequency estimates of 1:60,000 for all the US population, 1:38,000 for US population identified as Middle Eastern, and 1:205,000 for US population identified as African American [Lazarin et al 2013].
- 5.
Extrapolated prevalence based on detection rate of variants tested
Differential Diagnosis
In addition to hereditary fructose intolerance (HFI), the following disorders should be considered in the evaluation of hepatic insufficiency, unexplained jaundice [Leonardi et al 1986], and hypoglycemia, or in the setting of Reye-like illness in infancy or early childhood [Yang et al 2000, Thabet et al 2002]:
- Infectious hepatitis, sepsis, or disseminated intravascular coagulation [Maggiore & Borgna-Pignatti 1982]
- Autoimmune liver disease
- Neonatal hemochromatosis, which is considered a congenital alloimmune hepatitis
- Toxic ingestion
- Hemophagocytic lymphohistiocytosis [Mandel et al 1990]
- Alpha-1 antitrypsin deficiency
- Tyrosinemia type 1
- Galactosemia
- Urea cycle disorders
- Citrin deficiency
- Fatty acid oxidation disorders (including MCAD deficiency, LCHAD deficiency [OMIM 609016], and VLCAD deficiency)
- Organic acidemias
- Maple syrup urine disease
- Wilson disease
- Hepatic glycogenosis: glycogen storage disease (GSD) types Ia and Ib, GSD III, GSD IV, GSD VI, GSD types IXa1 and IXa2 (OMIM 306000), GSD IXb (OMIM 261750), GSD IXc (OMIM 613027), and GSD XI (OMIM 612933)
- Disorders of mitochondrial DNA depletion (including DGUOK-, MPV17-, and POLG-related disorders)
- Transaldolase deficiency
- Congenital disorders of glycosylation
In addition to HFI, the following disorders should be considered in the evaluation of infants with hyperlacticemia in combination with hypoglycemia:
- Severe infection/sepsis
- Disorders of gluconeogenesis (including 1,6-fructose bisphosphatase and pyruvate dehydrogenase deficiencies)
- Fatty acid oxidation disorders (including MCAD deficiency, LCHAD deficiency [OMIM 609016], and VLCAD deficiency)
- Organic acidemias
- Mitochondrial disorders
- Disorders of ketone metabolism (including HMG-CoA-lyase deficiency)
- Glycogenosis (including glycogen synthase deficiency)
In addition to HFI, the following disorders should be considered in the evaluation of infants with renal Fanconi/aminoaciduria and failure to thrive:
- Fanconi-Bickel syndrome (OMIM 227810)
- Renal tubular acidosis
- Mitochondrial disorders
- Congenital disorders of glycosylation
- Cystinosis
- Cystic fibrosis
Fructose malabsorption (or "dietary fructose intolerance"), in which fructose transporters in the small intestine are dysfunctional, is distinct from HFI. Symptoms overlap with those observed in HFI and include diarrhea, bloating, and increased flatulence with ingestion of fructose-containing substances. In severe cases, vomiting and abdominal pain may exist, leading to potential confusion with symptoms of HFI. The two disorders can be distinguished clinically by the presence of fructose in the urine in HFI and the presence of fructose in the stool in fructose malabsorption. Hydrogen breath test may be positive in fructose malabsorption; however, this requires oral fructose loading, which is potentially hazardous in the setting of true HFI [Müller et al 2003]. (See Agents/Circumstances to Avoid.)
Symptoms similar to those of HFI can also be seen in sucrase-isomaltase deficiency (OMIM 222900), but simple fructose is well tolerated in that disorder.
Autoimmune sensitivity to fructose in food protein-induced enterocolitis syndrome (FPIES) has also been reported [Fiocchi et al 2014].
Type I congenital disorders of glycosylation should be considered in the differential diagnosis of HFI [Adamowicz et al 2007, Pronicka et al 2007] due in part to the overlap in symptoms (including potential for hepatic insufficiency, failure to thrive, and aminoaciduria/renal Fanconi syndrome), but, more importantly, because HFI causes a secondary disorder of glycosylation [Quintana et al 2009] reflecting inhibitory effects of fructose-1-phosphate on phosphomannose isomerase [Jaeken et al 1996]. In HFI, clinical analysis of transferrin glycosylation may be positive, and should correct once fructose is adequately restricted and liver disease subsides. The pattern of abnormal glycosylation is not characteristic of a particular glycosylation defect, and sequencing of ALDOB or enzyme analysis in liver should be considered in instances where there is clinical suspicion for HFI. It should also be noted that in individuals who self-restrict fructose, quantifiable glycosylation abnormalities may resolve spontaneously, and thus transferrin glycosylation should be used with caution and not in isolation in the diagnosis of HFI.
Other
- In addition to HFI, the following disorders should be considered in the evaluation of adult- or childhood-onset of chronic liver disease: infection, toxic ingestion, and neoplasm.
- In addition to HFI, the following disorders should be considered in the evaluation of infantile/childhood-onset unexplained vomiting: gastroesophageal reflux, pyloric stenosis, urea cycle disorders, or galactose epimerase deficiency.
- In children or adults with early-onset and unexplained cataracts, cerebrotendinous xanthomatosis or galactokinase deficiency (OMIM 230200) should be considered.
- The co-occurrence of HFI and other conditions (e.g., phenylketonuria, celiac disease, and Duchenne muscular dystrophy) have delayed diagnosis and/or initiation of treatment of HFI in some instances [Celiker et al 1993, Ciacci et al 2006, Paolella et al 2012].
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with hereditary fructose intolerance (HFI), evaluation by the following specialists is recommended:
- Biochemical geneticist or pediatrician with an interest in metabolic disorders
- Dietician with experience in managing inherited metabolic diseases
- Hepatologist
- Nephrologist
- Clinical geneticist and/or genetic counselor
Treatment of Manifestations
Acute presentations should be managed symptomatically in a hospital setting, including intravenous glucose (dextrose) administration, supportive treatment of hepatic insufficiency (including fresh frozen plasma or exchange transfusion), and treatment of metabolic acidosis, if present.
Dietary restriction of fructose, sucrose, and sorbitol is the cornerstone of HFI treatment (see Prevention of Primary Manifestations). During acute episodes of intoxication, including at the time of initial diagnosis, immediate and absolute elimination of fructose (by substitution of fructose with other carbohydrate sources including glucose, maltose, and cornstarch) rapidly reverses symptoms and should result in normalization of related metabolic disturbances.
Ongoing education for children and adults concerning the need for dietary restriction is recommended, and should ideally be handled by nutritionists with specific experience in treating HFI and other inherited metabolic diseases.
Individuals with HFI are advised to wear a medically approved alert bracelet/necklace at all times.
Hepatomegaly with steatosis and lipid vacuolization may remain a persistent complication despite fructose restriction and resolution of initial fibrosis. This includes individuals ascertained by family history and treated from birth [Odièvre et al 1978]. The reason for this remains to be determined, but may be related to insufficient fructose restriction as well as lower tolerance of fructose early in life [Froesch et al 1963].
Chronic renal insufficiency, specifically proximal tubular dysfunction, may also persist despite fructose restriction. Typically resolution of renal disease occurs shortly after starting fructose restriction [Odièvre et al 1978]. In rare historical instances, dietary modification did not affect renal dysfunction [Mass et al 1966, Morris 1968]. This may be a result of earlier, incomplete attempts at restriction, as reported patients tended to manage themselves with self-restriction alone. It may also be in part due to primary defects in aldolase function and ATPase interaction within the proximal tubule, leading to dysfunctional acid-base regulation, renal tubular insufficiency (manifesting as glucosuria, aminoaciduria, and phosphaturia), and nephrocalcinosis [Mass et al 1966, Morris 1968, Lu et al 2001, Steinmann & Santer 2011].
Prevention of Primary Manifestations
Dietary restriction of fructose, sucrose, and sorbitol is necessary for the treatment/management of HFI (Table 3).
Specific ingredients to avoid include fructose, high-fructose corn syrup, honey, agave syrup, inverted sugar, maple-flavored syrup, molasses, palm or coconut sugar, and sorghum.
In addition, medicines and formulas in which fructose/sucrose may not be listed as a primary component, examples of which include syrups, enema solutions, some immunoglobulin solutions, and many infant and pediatric nutritional drinks. When ingredients are listed, the terms "sugar," "table sugar," "natural flavorings," and even in some cases "sugar-free" or "no added sugar" (with no further clarification on the type of carbohydrate used) should raise suspicion for the presence of fructose, sucrose, or sorbitol.
Table 3.
Dietary Guidelines for Hereditary Fructose Intolerance (HFI)
| Food Category | Foods Permitted | Foods Prohibited |
|---|---|---|
| Dairy | Any milk, cheese, eggs | Milk products w/added sugar (sweetened yogurt, fruit yogurt, milkshake, chocolate milk) |
| Meat | Beef, veal, lamb, pork | Ham, bacon, hot dogs, processed meats; any other meat where sugar is used in processing |
| Fish | All fish | None |
| Poultry | Chicken, turkey | None |
| Cereal | Cooked or ready-to-eat cereals (except sweetened & sugar-coated cereals) | Sweetened/sugar-coated cereals |
| Fruit | None | All fruits, fruit juices, including squashes & cordials, & fruit extracts prohibited |
| Vegetables | Asparagus, cabbage, cauliflower, celery, green beans, green peppers, lettuce, nuts, onions, potatoes, spinach, wax beans | All other vegetables, including sweet potatoes |
| Bread | Breads prepared w/out fructose, sucrose, sugar, or sorbitol; soda crackers & saltines | Any breads or crackers prepared w/fructose/sucrose/sugar/sorbitol |
| Fat sources | Butter, margarine, oil, mayonnaise / mustard prepared w/out sugar | Mayonnaises, mustards, & salad dressings made with sugar |
| Desserts and sweeteners | Dietetic jello, dietetic ice cream, dietetic puddings; natural yogurt; glucose, dextrose, dextrin, maltose & zero-calorie sweeteners | All desserts containing sugar (cake, pie, cookies, candy, jello, ice cream, sherbet, honey, fruit juice); sugar, sucrose, sorbitol, fructose |
| Miscellaneous | Vegetable juices, coffee, tea, salt, pepper, broths/soups from permitted vegetables; some sugar substitutes; some dietetic beverages; pasta; rice; cinnamon, garlic, poppy seeds; peanut butter (when pure & w/out added sugars) | Ketchup & any other sauces / condiments containing sugar, jam, jelly, preserves, carbonated beverages / soda; peanut butter if prepared w/added sugars; chewing gum w/sorbitol |
Adapted from www
.bu.edu/aldolase/HFI /treatment/sugar_table.htm
During hospitalizations special caution should be taken to avoid use of fructose-containing intravenous fluids. A number of reported accidental and iatrogenic fructose infusion-related deaths have prompted greater awareness of HFI [Locher 1987, Sachs et al 1993, Curran & Havill 2002, Müller et al 2003]; however, with a rare disorder such as HFI and in circumstances in which specific dietary (and infusion) restrictions may not be adequately disclosed, the danger of exposure in a hospital setting remains [Cox 1993]. The following are recommendations:
- During any hospitalization, all members of the care team should be aware of the diagnosis of HFI and the patient is advised to wear at all times a medically approved alert bracelet/necklace that provides information about the diagnosis of HFI.
- "Red flags" should be placed in the patient's chart or medical record to alert practitioners to the HFI diagnosis and to medical risks associated with exposures to foods and/or medications (oral or parenteral) containing fructose, sucrose, or sorbitol.
- Specific medicines known to contain fructose or fructose-like substances should be avoided.
- For parenteral medications, hospital pharmacists should be utilized and medications should be cleared for use on a case-by-case basis.
- Oral fructose challenge is no longer considered a favorable approach to diagnosis of HFI.
Dietary restriction should be strictly followed and maintained, especially in infancy. Although some have suggested that after age two years dietary restrictions can be relaxed somewhat [Steinmann & Santer 2011], currently, there are no specific guidelines regarding dietary fructose limits in any age group.
Tolerance of dietary fructose probably depends on an individual's residual enzyme activity. Furthermore, because actual fructose content in foods may be unreliably reported or difficult to ascertain, adherence to complete dietary restriction of fructose, sucrose, and sorbitol may be difficult attain and unrealistic for some patients with HFI.
Prevention of Secondary Complications
Ensuring adequate vitamin supplementation in the setting of reduced fruit and vegetable intake is imperative. Daily supplementation with a "sugar-free" multivitamin is recommended to prevent micronutrient deficiencies, specifically the water-soluble vitamins.
Surveillance
There are no formal guidelines for surveillance for individuals with HFI (e.g., frequency of subspecialty visits with physicians and/or dieticians with expertise in management of inherited metabolic diseases).
Once the diagnosis of HFI has been made, periodic evaluation of liver function, renal function, and growth is reasonable, particularly if there are concerns regarding compliance with the fructose/sucrose/sorbitol-restricted diet.
While isoelectric focusing of transferrin and/or monitoring of aspartylglucosaminidase (elevated in untreated HFI) have been suggested as markers of disease control in HFI, neither of these clinically available tests has definitively proven utility in diagnosis or surveillance [Pronicka et al 2007, Michelakakis et al 2009, Quintana et al 2009].
Agents/Circumstances to Avoid
Great care should be taken to avoid enteral or parenteral exposure to fructose, sorbitol, sucrose, sucralose, and polysorbate as administration of these substances to individuals with HFI can be fatal.
The following resources can be valuable in determining medical and dietary safety.
- Dietary guidance –including prohibited foods- is outlined in Table 3.
- An extensive list of tolerated and non-tolerated sugars in HFI can be found online, a site curated by the Boston University HFI laboratory.
- Although there is no single consolidated list of medications that contain these or related sugars, an advanced search on www.medicines.org.uk using the search term "fructose OR sorbitol OR sucrose OR sucralose" yielded 1776 results. Many such medications are oral suspensions or chewable flavored tabs designed for pediatric use. Also listed were injectable medications like immunoglobulin solutions (e.g., trastuzumab, filgrastim, some intravenous immunoglobulin solutions), vaccines (e.g., certain influenza, meningococcal), and iron supplements, as well as enema solutions and rinsing aids. For many preparations, it may not be apparent that fructose or similar compounds are present.
- For parenteral medications, hospital pharmacists should clear use of medications on a case-by-case basis. Of particular note, a 24% sucrose solution (routinely administered to hospitalized neonates for minor procedures) should not be given to neonates known to have HFI.
- The fructose tolerance testing ("fructose challenge") to diagnose HFI can be hazardous and should not be used.
Evaluation of Relatives at Risk
It may be appropriate to evaluate apparently asymptomatic older and younger sibs in order to identify individuals who would benefit from fructose restriction (see Prevention of Primary Manifestations). If the ALDOB pathogenic variants in the family are known, targeted molecular genetic testing can be used to clarify the genetic status of at-risk family members