Iminoglycinuria
A number sign (#) is used with this entry because of evidence that iminoglycinuria is a digenic phenotype that can be caused by homozygous mutation in the SLC36A2 gene (608331) combined with heterozygous mutation in the SLC6A20 gene (605616) or homozygous mutation in the SLC6A19 gene (608893).
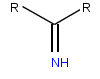
DescriptionThe imino acids, proline and hydroxyproline, share a renal tubular reabsorptive mechanism with glycine. Iminoglycinuria (IG), a benign inborn error of amino acid transport, is also a normal finding in neonates and infants under 6 months of age (Chesney, 2001). Early studies of families with iminoglycinuria suggested genetic complexity, with homozygotes developing IG and heterozygotes manifesting only hyperglycinuria (HG; 138500) (summary by Broer et al., 2008).
Iminoglycinuria may be more frequent in Ashkenazim than in others (Tancredi et al., 1970).
Iminoglycinuria also occurs as part of the generalized amino aciduria of the Fanconi renotubular syndrome (134600).
Clinical FeaturesRosenberg et al. (1968) found increased amounts of the 2 imino acids proline and hydroxyproline as well as glycine in the urine of a 6-year-old boy with congenital nerve deafness. Both parents had hyperglycinuria without imino aciduria. No defect in intestinal transport of these substances was found. These authors, as well as Whelan and Scriver (1968), concluded that iminoglycinuria is the homozygous form of the trait that presents as hyperglycinuria (HG; 138500) in the heterozygote.
Genetic heterogeneity in iminoglycinuria was suggested by the facts that only some apparent homozygotes show a defect in intestinal absorption of L-proline (Goodman et al., 1967; Scriver, 1968), and that only some obligate heterozygotes show hyperglycinuria with glycine loading (Scriver, 1968). Scriver (1968) observed the instructive case of an apparent homozygote's child whose father had hyperglycinuria and whose mother did not. He suggested that this child was a 'compound' carrying 2 different mutant alleles. Similar presumed genetic compounds for cystinuria (220100) had been observed.
Based on observations of inheritance patterns in affected families, Scriver (1989) suggested that the different putative mutations are allelic, inasmuch as the same renal phenotype had been observed in probands inheriting 2 'silent' mutant alleles, 2 'hyperglycinuric' alleles, or 2 different alleles. In addition, Scriver (1989) stated that several different forms of renal hyperglycinuria are known which must be distinguished from the hyperglycinuric phenotype that occurs in heterozygotes for the 'incompletely recessive' form of renal iminoglycinuria, e.g., hyperglycinuria and nephrolithiasis (138500), glucoglycinuria (138070), and x-linked hypophosphatemia with glucoglycinuria (see 307800).
Associated Features
Further heterogeneity is suggested by description of associated mental retardation (Statter et al., 1976). The deafness associated in the case of Rosenberg et al. (1968) and the blindness in the cases of Tancredi et al. (1970) and Fraser (1971) were probably coincidental associations related to the populations screened.
Saito et al. (1981) described atypical gyrate atrophy in a 44-year-old woman whose parents were first cousins and who showed strikingly increased urinary excretion of proline, hydroxyproline, and glycine. They suggested that the occurrence of gyrate atrophy with ornithinemia (258870), together with this observation, indicates that proline deficiency in chorioretinal tissues may be the mechanism of gyrate atrophy.
Molecular GeneticsBroer et al. (2008) studied 3 French Canadian and 4 Australian families, each with an index case previously identified from newborn urinary screening programs for iminoglycinuria (IG). IG was reconfirmed in all but 2 of the probands: in 2 of the Australian families, the probands had only persistent hyperglycinuria (HG; 138500). Broer et al. (2008) sequenced 5 known imino acid and glycine transporter candidates and found that the main contribution to IG and HG arose from defects in the gene encoding the proton amino acid transporter SLC36A2 (608331.0001-608331.0002), with a classic semidominant inheritance pattern in which 2 nonfunctional alleles conferred the IG phenotype whereas 1 nonfunctional allele was sufficient to confer the HG phenotype. Mutations in SLC36A2 that retained residual transport activity resulted in the IG phenotype only when combined with haploinsufficiency of the imino acid transporter SLC6A20 (605616.0001) or deficiency of the neutral amino acid transporter SLC6A19 (608893.0005). Broer et al. (2008) noted that additional polymorphisms and mutations were identified in the gene encoding the putative glycine transporter SLC6A18 (610300) in these affected individuals, and suggested that variation in SLC6A18 might also contribute to these phenotypes. Thus, IG and HG exhibit complex molecular explanations depending on a major gene and accompanying modifier genes.