Glioma

A glioma is a type of tumor that starts in the glial cells of the brain or the spine. Gliomas comprise about 30 percent of all brain tumors and central nervous system tumours, and 80 percent of all malignant brain tumours.
Signs and symptoms
Symptoms of gliomas depend on which part of the central nervous system is affected. A brain glioma can cause headaches, vomiting, seizures, and cranial nerve disorders as a result of increased intracranial pressure. A glioma of the optic nerve can cause visual loss. Spinal cord gliomas can cause pain, weakness, or numbness in the extremities. Gliomas do not usually metastasize by the bloodstream, but they can spread via the cerebrospinal fluid and cause "drop metastases" to the spinal cord. Complex visual hallucinations have been described as a symptom of low-grade glioma.
A child who has a subacute disorder of the central nervous system that produces cranial nerve abnormalities (especially of cranial nerve VII and the lower bulbar nerves), long-tract signs, unsteady gait secondary to spasticity, and some behavioral changes is most likely to have a pontine glioma.
Causes
Hereditary disorders
The exact causes of gliomas are not known. Hereditary disorders such as neurofibromatoses (type 1 and type 2) and tuberous sclerosis complex are known to predispose to their development. Different oncogenes can cooperate in the development of gliomas.
Diet
Some studies of diet and vitamin supplementation seem to indicate that dietary N-nitroso compounds might influence the risk of both childhood and adult brain tumors. Researchers have observed in some studies that brain tumor patients (or their mothers) have generally consumed more cured foods (also known as Curing) than control groups. Recently, Drs. Lee, Wrensch and others found that adults with glioma were more likely to consume diets high in cured foods and low in vitamin C-rich fruits and vegetables, and to consume diets high in nitrites and low in vitamin C. The effect was more pronounced in men than women. However, the pattern of increased risk with increased consumption of cured foods, and decreased risk with greater consumption of fruits, vegetables, and antioxidant vitamins is compatible with other cancer studies that show increased consumption of vegetables and possibly of fruits is associated with decreased cancer risk.
Radiation
A link between gliomas and electromagnetic radiation from cell phones has not been conclusively proven. It was considered possible, though several large studies have found no conclusive evidence, as summarized by the NIH's National Cancer Institute review of the topic and its numerous citations, and the FCC. However, further research is still being pursued to obtain more robust evidence and verify that there is no relationship (the NIH's National Institute of Environmental Health Sciences most recent press release discussed an ongoing study showing mildly positive results, although it appears there may have been issues with the control group dying prematurely).
Infection with cytomegalovirus
Most glioblastomas are infected with cytomegalovirus, which speeds the development of tumors.
Other causes
Though some studies have shown that farmers have higher rates of gliomas compared to the general population, exposure to farm animals or manure is not associated with glioma. Later studies have not found an association between farming and gliomas; similar conflicting data concerns teachers and glioma. More consistent data show that architects, surveyors, retail workers, butchers, and engineers have higher rates of gliomas. Most studies have found that pesticide exposure is probably not a cause of glioma, though a minority of studies have found an association.
Inherited polymorphisms of the DNA repair genes
Germ-line (inherited) polymorphisms of the DNA repair genes ERCC1, ERCC2 (XPD) and XRCC1 increase the risk of glioma. This indicates that altered or deficient repair of DNA damage contributes to the formation of gliomas. DNA damages are a likely major primary cause of progression to cancer in general. Excess DNA damages can give rise to mutations through translesion synthesis. Furthermore, incomplete DNA repair can give rise to epigenetic alterations or epimutations. Such mutations and epimutations may provide a cell with a proliferative advantage which can then, by a process of natural selection, lead to progression to cancer.
Epigenetic repression of DNA repair genes is often found in progression to sporadic glioblastoma. For instance, methylation of the DNA repair gene MGMT promoter was observed in 51% to 66% of glioblastoma specimens. In addition, in some glioblastomas, the MGMT protein is deficient due to another type of epigenetic alteration. MGMT protein expression may also be reduced due to increased levels of a microRNA that inhibits the ability of the MGMT messenger RNA to produce the MGMT protein. Zhang et al. found, in the glioblastomas without methylated MGMT promoters, that the level of microRNA miR-181d is inversely correlated with protein expression of MGMT and that the direct target of miR-181d is the MGMT mRNA 3'UTR (the three prime untranslated region of MGMT messenger RNA).
Epigenetic reductions in expression of another DNA repair protein, ERCC1, were found in an assortment of 32 gliomas. For 17 of the 32 (53%) of the gliomas tested, ERCC1 protein expression was reduced or absent. In the case of 12 gliomas (37.5%) this reduction was due to methylation of the ERCC1 promoter. For the other 5 gliomas with reduced ERCC1 protein expression, the reduction could have been due to epigenetic alterations in microRNAs that affect ERCC1 expression.
When expression of DNA repair genes is reduced, DNA damages accumulate in cells at a higher than normal level, and such excess damages cause increased frequencies of mutation. Mutations in gliomas frequently occur in either isocitrate dehydrogenase (IDH) 1 or 2 genes. One of these mutations (mostly in IDH1) occurs in about 80% of low grade gliomas and secondary high-grade gliomas. Wang et al. pointed out that IDH1 and IDH2 mutant cells produce an excess metabolic intermediate, 2-hydroxyglutarate, which binds to catalytic sites in key enzymes that are important in altering histone and DNA promoter methylation. Thus, mutations in IDH1 and IDH2 generate a "DNA CpG island methylator phenotype or CIMP" that causes promoter hypermethylation and concomitant silencing of tumor suppressor genes such as DNA repair genes MGMT and ERCC1. On the other hand, Cohen et al. and Molenaar et al. pointed out that mutations in IDH1 or IDH2 can cause increased oxidative stress. Increased oxidative damage to DNA could be mutagenic. This is supported by an increased number of DNA double-strand breaks in IDH1-mutated glioma cells. Thus, IDH1 or IDH2 mutations act as driver mutations in glioma carcinogenesis, though it is not clear by which role they are primarily acting. A study, involving 51 patients with brain gliomas who had two or more biopsies over time, showed that mutation in the IDH1 gene occurred prior to the occurrence of a p53 mutation or a 1p/19q loss of heterozygosity, indicating that an IDH1 mutation is an early driver mutation.
Pathophysiology
High-grade gliomas are highly vascular tumors and have a tendency to infiltrate diffusely. They have extensive areas of necrosis and hypoxia. Often, tumor growth causes a breakdown of the blood–brain barrier in the vicinity of the tumor. As a rule, high-grade gliomas almost always grow back even after complete surgical excision, so are commonly called recurrent cancer of the brain.
Conversely, low-grade gliomas grow slowly, often over many years, and can be followed without treatment unless they grow and cause symptoms.
Several acquired (not inherited) genetic mutations have been found in gliomas. Tumor suppressor protein 53 (p53) is mutated early in the disease. p53 is the "guardian of the genome", which, during DNA and cell duplication, makes sure the DNA is copied correctly and destroys the cell (apoptosis) if the DNA is mutated and cannot be fixed. When p53 itself is mutated, other mutations can survive. Phosphatase and tensin homolog (PTEN), another tumor suppressor gene, is itself lost or mutated. Epidermal growth factor receptor, a growth factor that normally stimulates cells to divide, is amplified and stimulates cells to divide too much. Together, these mutations lead to cells dividing uncontrollably, a hallmark of cancer. In 2009, mutations in IDH1 and IDH2 were found to be part of the mechanism and associated with a less favorable prognosis.
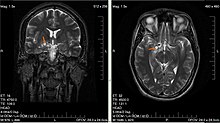
Diagnosis
Classification
Gliomas are classified by cell type, by grade, and by location.
By type of cell
Gliomas are named according to the specific type of cell with which they share histological features, but not necessarily from which they originate. The main types of gliomas are:
- Ependymomas: ependymal cells
- Astrocytomas: astrocytes (glioblastoma multiforme is a malignant astrocytoma and the most common primary brain tumor among adults).
- Oligodendrogliomas: oligodendrocytes
- Brainstem glioma: develop in the brain stem
- Optic nerve glioma: develop in or around the optic nerve
- Mixed gliomas, such as oligoastrocytomas, contain cells from different types of glia
By grade
Gliomas are further categorized according to their grade, which is determined by pathologic evaluation of the tumor. The neuropathological evaluation and diagnostics of brain tumor specimens is performed according to WHO Classification of Tumours of the Central Nervous System.
- Biologically benign gliomas [WHO grade I] are comparatively low risk and can be removed surgically depending on their location
- Low-grade gliomas [WHO grade II] are well-differentiated (not anaplastic); these tend to exhibit benign tendencies and portend a better prognosis for the patient. However, they have a uniform rate of recurrence and increase in grade over time so should be classified as malignant.
- High-grade [WHO grades III–IV] gliomas are undifferentiated or anaplastic; these are malignant and carry a worse prognosis.
Of numerous grading systems in use, the most common is the World Health Organization (WHO) grading system for astrocytoma, under which tumors are graded from I (least advanced disease—best prognosis) to IV (most advanced disease—worst prognosis).
By location
Gliomas can be classified according to whether they are above or below a membrane in the brain called the tentorium. The tentorium separates the cerebrum (above) from the cerebellum (below).
- The supratentorial is above the tentorium, in the cerebrum, and mostly found in adults (70%).
- The infratentorial is below the tentorium, in the cerebellum, and mostly found in children (70%).
- The pontine tumors are located in the pons of the brainstem. The brainstem has three parts (pons, midbrain, and medulla); the pons controls critical functions such as breathing, making surgery on these extremely dangerous.
Treatment
Treatment for brain gliomas depends on the location, the cell type, and the grade of malignancy. Often, treatment is a combined approach, using surgery, radiation therapy, and chemotherapy. The radiation therapy is in the form of external beam radiation or the stereotactic approach using radiosurgery. Spinal cord tumors can be treated by surgery and radiation. Temozolomide is a chemotherapy drug which can be administered easily in an outpatient setting and is able to cross the blood–brain barrier effectively. Treatment via immunotherapy may help some gliomas.
Refractory disease
For recurrent high-grade glioblastoma, recent studies have taken advantage of angiogenic blockers such as bevacizumab in combination with conventional chemotherapy, with encouraging results.
Relative effectiveness
A 2017 meta-analysis compared surgical resection versus biopsy as the initial surgical management option for a person with a low-grade glioma. Results show the evidence is insufficient to make a reliable decision. The relative effectiveness of surgical resection compared to biopsy for people with malignant glioma (high-grade) is unknown.
For high-grade gliomas, a 2003 meta-analysis compared radiotherapy with radiotherapy and chemotherapy. It showed a small but clear improvement from using chemotherapy with radiotherapy. A 2019 meta-analysis suggested that for people with less aggressive gliomas, radiotherapy may increase the risk of long term neurocognitive side effects. Whilst, evidence is uncertain on whether there are long term neurocognitive side effects associated with chemoradiotherapy.
Temozolomide is effective for treating Glioblastoma Multiforme (GBM) compared to radiotherapy alone. A 2013 meta-analysis showed that Temozolomide prolongs survival and delays progression, but is associated with an increase in side effects such as blood complications, fatigue, and infection. For people with recurrent GBM, when comparing temozolomide with chemotherapy, there may be an improvement in the time-to-progression and the person's quality of life, but no improvement in overall survival, with temozolomide treatment. Evidence suggests that for people with recurrent high-grade gliomas who have not had chemotherapy before, there are similar survival and time-to-progression outcomes between treatment with temozolomide or the chemotherapy multidrug known as PCV (procarvazine, lomustine and vincristine).
A mutational analysis of 23 initial low-grade gliomas and recurrent tumors from the same patients has challenged the benefits and usage of Temozolomide. The study showed that when lower-grade brain tumors of patients are removed and patients are further treated with Temozolomide, 6 out of 10 times the recurrent tumors were more aggressive and acquired alternative and more mutations. As one of the last authors, Costello, stated "They had a 20- to 50-fold increase in the number of mutations. A patient who received surgery alone who might have had 50 mutations in the initial tumor and 60 in the recurrence. But patients who received TMZ might have 2,000 mutations in the recurrence." Further, new mutations were verified to carry known signatures of Temozolomide induced mutations. The research suggests that Temozolomide for the treatment of certain brain tumors should be thoroughly thought. Unjudicious usage of Temozolomide might lower the prognosis of the patients further, or increase their burden. Further understanding of the mechanisms of Temozolomide induced mutations and novel combination approaches could be promising.
Prognosis
Prognosis of gliomas is given in relation to what grade (as scored by the World Health Organization system) of tumour the patient presents with. Typically, any tumour presenting as above WHO grade I (i.e. a malignant tumour as opposed to a benign tumour) will have a prognosis resulting in eventual death, varying from years (WHO grade II/III) to months (WHO grade IV). Prognosis can also be given based on cellular subtype, which may also impact prognosis.
Low grade
For low-grade tumors, the prognosis is somewhat more optimistic. Patients diagnosed with a low-grade glioma are 17 times as likely to die as matched patients in the general population. The age-standardized 10-year relative survival rate was 47%. One study reported that low-grade oligodendroglioma patients have a median survival of 11.6 years; another reported a median survival of 16.7 years. Unfortunately, approximately 70% of low-grade (WHO grade-II) will progress to high-grade tumours within 5–10 years
High grade
This group comprises anaplastic astrocytomas and glioblastoma multiforme. Whereas the median overall survival of anaplastic (WHO grade III) gliomas is approximately 3 years, glioblastoma multiforme has a poor median overall survival of c. 15 months.
Postoperative conventional daily radiotherapy improves survival for adults with good functional well‐being and high grade glioma compared to no postoperative radiotherapy. Hypofractionated radiation therapy has similar efficacy for survival as compared to conventional radiotherapy, particularly for individuals aged 60 and older with glioblastoma.
Diffuse intrinsic pontine glioma
Diffuse intrinsic pontine glioma primarily affects children, usually between the ages of 5 and 7. The median survival time with DIPG is under 12 months. Surgery to attempt tumour removal is usually not possible or advisable for DIPG. By their very nature, these tumours invade diffusely throughout the brain stem, growing between normal nerve cells. Aggressive surgery would cause severe damage to neural structures vital for arm and leg movement, eye movement, swallowing, breathing, and even consciousness. Trials of drug candidates have been unsuccessful. The disease is primarily treated with radiation therapy alone.
IDH1 and IDH2-mutated glioma
Patients with glioma carrying mutations in either IDH1 or IDH2 have a relatively favorable survival, compared with patients with glioma with wild-type IDH1/2 genes. In WHO grade III glioma, IDH1/2-mutated glioma have a median prognosis of ~3.5 years, whereas IDH1/2 wild-type glioma perform poor with a median overall survival of c. 1.5 years. In glioblastoma, the difference is larger. There, IDH1/2 wild-type glioblastoma have a median overall survival of 1 year, whereas IDH1/2-mutated glioblastoma have a median overall survival of more than 3 years.