Congenital Thrombotic Thrombocytopenic Purpura
A hereditary form of thrombotic thrombocytopenic purpura (TTP) characterized by profound peripheral thrombocytopenia, microangiopathic hemolytic anemia (MAHA) and single or multiple organ failure of variable severity.
Epidemiology
Congenital TTP is much less common than the immune-mediated form of the disease (immune-mediated TTP), accounting for up to only 5% of all TTP cases. Up until 2017, 123 cases had been reported by the International Hereditary Thrombotic Thrombocytopenic Purpura Registry. The annual incidence is estimated at less than 1/1,000,000.
Clinical description
The majority of patients present during the neonatal period or during childhood but the clinical manifestations are highly variable with mild manifestations of isolated thrombocytopenia throughout childhood in some, and severe neonatal hyperbilirubinemia with episodes of thrombocytopenia and MAHA developing soon after birth in others. In addition, onset may also occur during adulthood, particularly in women when the initial episode of overt TTP is triggered by the first pregnancy. Infections and vaccinations are also precipitating factors. The clinical course in congenital TTP is characterized typically by more long term relapses than in the immune-mediated form (iTTP), with around 50% of congenital TTP patients developing chronic, frequently relapsing disease. As in immune-mediated TTP, patients may also develop neurological anomalies, renal manifestations, cardiac dysfunction and gastrointestinal symptoms due to widespread microvascular thrombosis.
Etiology
Congenital TTP is caused by a mutation in the ADAMTS13 gene (9q34), encoding ADAMTS13, a metalloprotease involved in the cleavage of ultra-large von Willebrand factor multimers with a penetrance of over 90%. Mutations are mainly compound heterozygous and less commonly homozygous, which explains the varied age of onset and severity/frequency of episodes seen in patients with congenital TTP.
Diagnostic methods
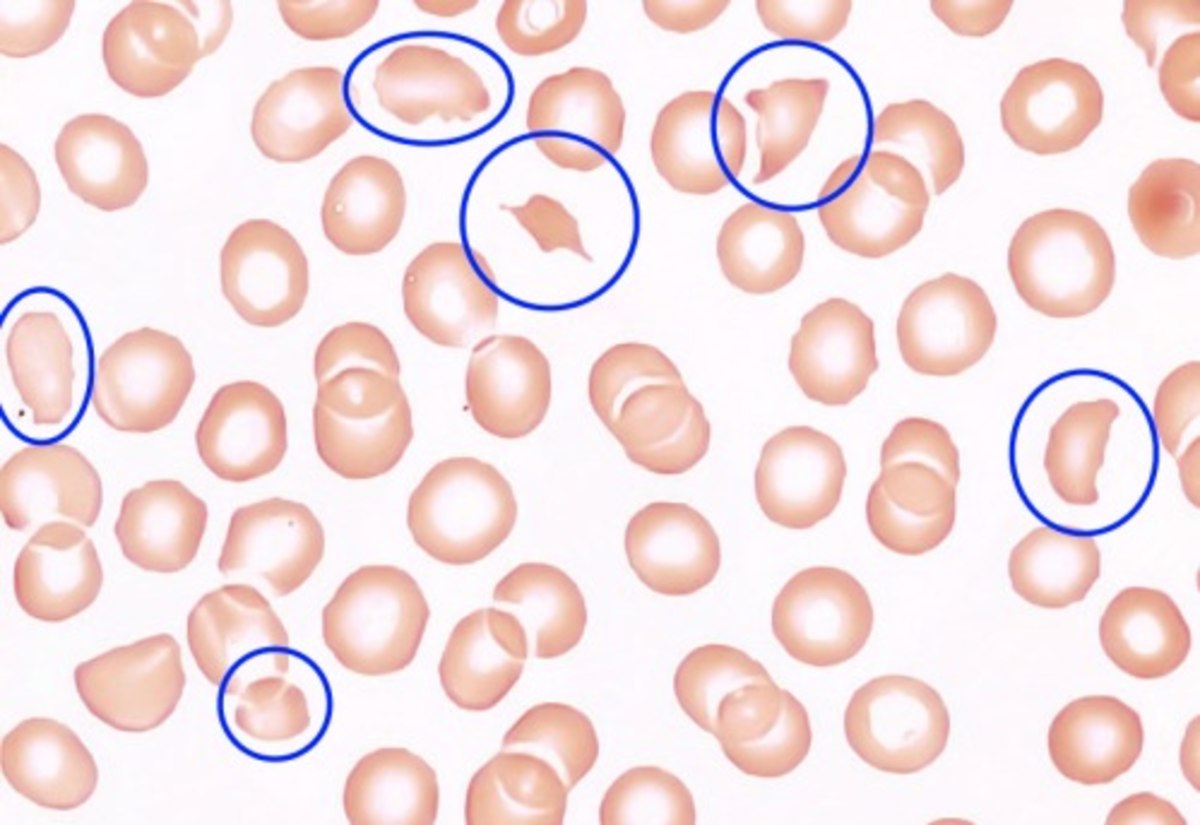
A diagnosis of TTP should be considered in all patients with thrombocytopenia and microangiopathic hemolytic anemia. A positive familial history, laboratory studies (revealing schistocytes on peripheral blood smears, high serum lactate dehydrogenase levels, low platelet counts and reticulocytosis) and a severe ADAMTS13 deficiency (< 10% of normal values), in the absence of anti-ADAMTS13 antibodies, suggests a diagnosis of congenital TTP. Diagnosis is confirmed by molecular analysis revealing a double heterozygous or homozygous mutation in the ADAMTS13 gene.
Differential diagnosis
In pregnant patients, congenital TTP needs to be distinguished from iTTP, atypical hemolytic-uremic syndrome and HELLP syndrome.
Genetic counseling
Congenital TTP is transmitted in an autosomal recessive manner. Genetic counseling should be provided to affected families. Women diagnosed with congenital TTP should also receive pregnancy counseling in order to inform them of the major risk of TTP exacerbations and to allow for the timely planning of a management strategy (from conception to post-partum period), which mainly includes a prophylactic plasmatherapy. Screening of siblings for ADAMTS13 activity is also recommended.
Management and treatment
Acute episodes in congenital TTP can be treated by plasma infusion (10-15 ml/kg/day until remission) but exchange transfusion is usually required in newborns. Patients with a chronic relapsing disease course may be considered for prophylactic plasma therapy. Regular plasma infusions to maintain ADAMTS13 activity level around 15% are required during pregnancy, in addition to close clinical and biological monitoring by a reference center. During the third trimester, therapeutic plasma exchanges may be required to prevent fluid overload.
Prognosis
In the absence of treatment, TTP is a rapidly fatal disease (mortality rate > 90%). The introduction of therapeutic plasma exchange and plasma infusion has led to a decrease in the mortality rate to around 15%. Plasmatherapy also prevents long term organ complications due to chronic relapses.