Heparin-Induced Thrombocytopenia
A rare drug-induced, immune-mediated prothrombotic disorder associated with thrombocytopenia and venous and/or arterial thrombosis.
Epidemiology
Approximately 1% of patients exposed to heparin for at least one week develop HIT, and approximately 50% of them will have thrombosis. HIT is slightly more common in females.
Clinical description
HIT may develop at any age (>3 months) but pediatric cases are rare. Moderate thrombocytopenia begins typically 5- 10 days after heparin administration. If the patient had already been exposed to heparin within the last 100 days, rapid-onset is possible, with the platelet count drop occurring within minutes or hours after heparin administration. Delayed-onset HIT is also possible with thrombocytopenia beginning after heparin has already been discontinued. Thrombocytopenia is usually asymptomatic; bleeding is rare. HIT is associated with a high risk of thrombotic complications (e.g. pulmonary embolism, myocardial infarction, thrombotic stroke), with a strong predilection for arterial thrombosis involving limb arteries and deep vein thrombosis. Additional microvascular thrombosis can lead to venous limb gangrene/amputation. Other complications include skin necrosis at heparin injection sites and anaphylactoid reactions (e.g. fever, hypotension, chest pain, dyspnea, cardiorespiratory arrest) that could be secondary to post-intravenous heparin bolus.
Etiology
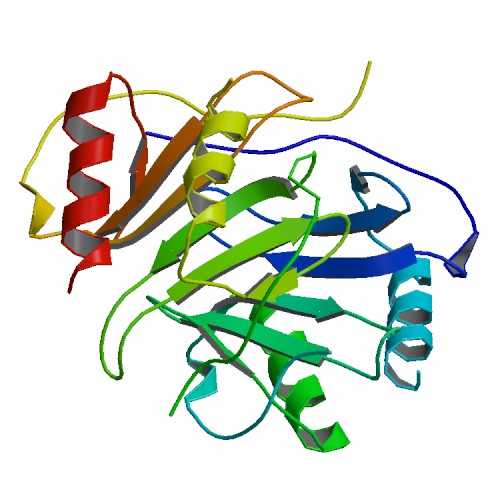
HIT results from a humoral immune reaction directed against a complex involving endogenous platelet factor 4 (PF4) and exogenous heparin: auto-antibodies recognize PF4 only when it is complexed with heparin. This immune complex activates the circulating platelets via their FcγRIIA surface receptors, leading to consumptive thrombocytopenia and hypercoagulability. The source of heparin (bovine >porcine), its formulation (unfractionated >low molecular weight >fondaparinux), the dose (prophylactic >therapeutic >heparin flushes), route of administration (subcutaneous >intravenous) and duration of administration (over 4 days >4 days or less) are determining factors.
Diagnostic methods
Diagnosis of HIT is suspected from the clinical picture based on the ''4 T's'' (Thrombocytopenia, Timing, Thrombosis, no oTher cause of platelet fall) or the HIT Expert Probability (HEP) scoring system. It is supported by detection of anti-PF4/heparin antibodies, most often by ELISA (although 50% of ELISA-positive patients do not have HIT), and confirmed by detection of pathologic platelet-activating antibodies with the serotonin-release assay or the heparin-induced platelet activation test.
Differential diagnosis
Differential diagnosis includes nonimmune heparin-associated thrombocytopenia (due to the direct interaction of heparin with circulating platelets, occurring during the first days of heparin administration), as well as postoperative hemodilution, sepsis, non-HIT drug-induced thrombocytopenia, disseminated intravascular coagulation, and multiorgan system failure.
Management and treatment
For certain patient populations receiving heparin, a regular monitoring of platelet counts is recommended. In case of strongly-suspected or confirmed HIT, treatment consists of stopping heparin and initiating alternative anticoagulant treatment, either with non-heparin anti-factor Xa therapies (danaparoid, fondaparinux), or with direct thrombin inhibitors (e.g., argatroban, bivalirudin). Warfarin is contraindicated during the acute thrombocytopenic phase as it can cause microvascular thrombosis, with potential for ischemic limb necrosis (venous limb gangrene syndrome). Thrombocytopenia generally resolves to greater than 150 x 109/L at a median of 4 days, although 1 week to 1 month can be required in some cases.
Prognosis
The prognosis for platelet count recovery is excellent; however, long-term post-thrombotic sequelae (e.g. limb amputation in 5-10% of HIT patients, disabling stroke, bilateral adrenal hemorrhagic necrosis with adrenal failure) can occur. HIT-related mortality (e.g. fatal pulmonary embolism) is observed in 5-10% of cases.