Pmm2-Cdg (Cdg-Ia)
Summary
Clinical characteristics.
PMM2-CDG (CDG-Ia) (previously known as congenital disorder of glycosylation type 1a), the most common of a group of disorders of abnormal glycosylation of N-linked oligosaccharides, is divided into three types: infantile multisystem, late-infantile and childhood ataxia-intellectual disability, and adult stable disability. The three types notwithstanding, clinical presentation and course are highly variable, ranging from infants who die in the first year of life to mildly involved adults. Clinical presentations tend to be similar in sibs.
- In the infantile multisystem type, infants show axial hypotonia, hyporeflexia, esotropia, and developmental delay. Feeding problems, vomiting, failure to thrive, and impaired growth are frequently seen. Subcutaneous fat may be excessive over the buttocks and suprapubic region. Two distinct clinical presentations are observed: (1) a non-fatal neurologic form with strabismus, psychomotor retardation, and cerebellar hypoplasia in infancy followed by neuropathy and retinitis pigmentosa in the first or second decade and (2) a neurologic-multivisceral form with approximately 20% mortality in the first year of life.
- The late-infantile and childhood ataxia-intellectual disability type, with onset between age three and ten years, is characterized by hypotonia, ataxia, severely delayed language and motor development, inability to walk, and IQ of 40 to 70; other findings include seizures, stroke-like episodes or transient unilateral loss of function, retinitis pigmentosa, joint contractures, and skeletal deformities.
- In the adult stable disability type, intellectual ability is stable; peripheral neuropathy is variable, thoracic and spinal deformities progress, and premature aging is observed; females lack secondary sexual development and males may exhibit decreased testicular volume. Hyperglycemia-induced growth hormone release, hyperprolactinemia, insulin resistance, and coagulopathy may occur. An increased risk for deep venous thrombosis is present.
Diagnosis/testing.
The diagnosis of PMM2-CDG (CDG-Ia) is established in a proband with type I transferrin isoform pattern and either identification of biallelic pathogenic variants in PMM2 on molecular genetic testing or low levels of phosphomannomutase (PMM) enzyme activity if results of molecular genetic testing are uncertain.
Management.
Treatment of manifestations: Maximal caloric intake including use of a nasogastric tube or gastrostomy tube; anti-gastroesophageal reflux measures; occupational therapy, physical therapy, and speech therapy for developmental delay; hydration and physical therapy for stroke-like episodes; orthopedic intervention for scoliosis; rehabilitation medicine services including wheelchairs, transfer devices, and physical therapy as needed.
Prevention of secondary complications: Attention to coagulation status before surgery because of increased risk of bleeding and/or deep venous thrombosis. Education about risks and symptoms of deep venous thrombosis.
Agents/circumstances to avoid: Cautious use of acetaminophen and other agents metabolized by the liver.
Genetic counseling.
PMM2-CDG (CDG-Ia) is inherited in an autosomal recessive manner. At conception, the theoretic risks to sibs of an affected individual are a 25% risk of being affected, a 50% risk of being an asymptomatic carrier, and a 25% risk of being unaffected and not a carrier; however, based on outcomes of at-risk pregnancies, the risk of having an affected child is closer to 1/3 than to the expected 1/4. Carrier testing for at-risk family members and prenatal diagnosis for pregnancies at increased risk are possible if both PMM2 pathogenic variants in the family have been identified.
Diagnosis
PMM2-CDG (CDG-Ia) is the most common of a group of disorders of abnormal glycosylation of N-linked oligosaccharides.
Suggestive Findings
PMM2-CDG (CDG-Ia) should be suspected in a child, adolescent or adult, or fetus with the following findings.
In a Child
A child with developmental delay and hypotonia in combination with any of the following clinical and laboratory findings:
- Clinical findings
- Failure to thrive
- Hypothyroidism, hypogonadism
- Esotropia
- Pericardial effusion
- Abnormal subcutaneous fat pattern including increased suprapubic fat pad, skin dimpling, and inverted nipples or subcutaneous fat pads having a toughened, puffy, or uneven consistency
- Seizures
- Stroke-like episodes
- Osteopenia, scoliosis
- Cerebellar hypoplasia/atrophy and small brain stem [Aronica et al 2005] and characteristic findings on brain MRI (see Clinical Description)
- Laboratory findings
- Hepatic dysfunction (elevated transaminases)
- Coagulopathy with low serum concentration of factors IX and XI, antithrombin III, protein C, and/or protein S
- Type I transferrin isoform pattern on analysis of serum transferrin glycoforms (also called "transferrin isoforms analysis" or "carbohydrate-deficient transferrin analysis"). The analysis, based on isoform analysis (by isoelectric focusing (IEF) or other methods (capillary electrophoresis, GC/MS, CE-ESI-MS, MALDI-MS), determines the number of sialylated N-linked oligosaccharide residues linked to serum transferrin [Jaeken & Carchon 2001, Marklová & Albahri 2007, Sanz-Nebot et al 2007].Results of such testing may reveal the following:
- Normal transferrin isoform pattern. Two biantennary glycans linked to asparagine with four sialic acid residues
- Type I transferrin isoform pattern. Decreased tetrasialotransferrin and increased asialotransferrin and disialotransferrin. The pattern indicates defects in the earliest synthetic steps of the N-linked oligosaccharide synthetic pathway.
- Type II transferrin isoform pattern. Increased trisialotransferrins and/or monosialotransferrins. The pattern indicates defects in the later parts of the N-linked glycan pathway.
Note: (1) The diagnostic validity of analysis of serum transferrin glycoforms before age three weeks is controversial [Clayton et al 1992, Stibler & Skovby 1994]. (2) The use of Guthrie cards with whole blood samples is not suggested; however, the use of Guthrie cards with blotted serum yields accurate results [Carchon et al 2006]. (3) Individuals with the clinical diagnosis of PMM2-CDG (CDG-Ia) and biochemical diagnosis of PMM enzyme deficiency with normal transferrin glycosylation have been reported [Fletcher et al 2000, Marquardt & Denecke 2003, Hahn et al 2006]. (4) The possibility that an abnormal transferrin glycoform analysis is the result of a transferrin protein variant can be confirmed with a glycoform analysis of a serum sample from the parents or by a neuraminidase treatment followed by IEF and ESI-TOF MS [Park et al 2014, Zühlsdorf et al 2015]. (5) In adults with milder forms of PMM2-CDG (CDG-Ia), serum transferrin glycoforms can be mildly abnormal or near normal [Wolthuis et al 2014].
In an Adolescent or Adult
An adolescent or adult with any of the following clinical and laboratory findings:
- Clinical findings
- Cerebellar dysfunction (ataxia, dysarthria, dysmetria) and characteristic findings on brain MRI (see Clinical Description)
- Non-progressive cognitive impairment
- Seizures
- Stroke-like episodes
- Peripheral neuropathy with or without muscle wasting
- Absent puberty in females, small testes in males
- Retinitis pigmentosa
- Progressive scoliosis with truncal shortening
- Joint contractures
- Laboratory findings. Type I transferrin isoform pattern on analysis of serum transferrin glycoforms (see In a Child, Laboratory findings, Type I transferrin isoform pattern)
In a Fetus
A fetus with non-immune hydrops fetalis [van de Kamp et al 2007, Léticée et al 2010]
Establishing the Diagnosis
The diagnosis of PMM2-CDG (CDG-Ia) is established in a proband with type I transferrin isoform pattern and identification of either biallelic pathogenic variants in PMM2 on molecular genetic testing (see Table 1) or low levels of phosphomannomutase (PMM) enzyme activity if results of molecular genetic testing are uncertain.
Molecular testing approaches can include single-gene testing, a multigene panel, and more comprehensive genomic testing.
Single-gene testing. Sequence analysis of PMM2 is performed first and followed by gene-targeted deletion/duplication analysis if only one or no pathogenic variant is found.
Note: Three pathogenic variants are common in individuals of European ancestry and may be included on carrier screening panels:
- The pathogenic variant p.Arg141His is found in the compound heterozygous state in approximately 40% of individuals; it is never found in the homozygous state.
- The pathogenic variant p.Phe119Leu is frequently found in northern Europe, where the genotype [p.Arg141His]+[p.Phe119Leu] makes up a majority of all pathogenic variants [Jaeken & Matthijs 2001].
- The pathogenic variants p.Val231Met and p.Pro113Leu are common all over Europe.
A multigene panel that includes PMM2 and other genes of interest (see Differential Diagnosis) may also be considered. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview; thus, clinicians need to determine which multigene panel is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
More comprehensive genomic testing (when available) including exome sequencing and genome sequencing may be considered if serial single-gene testing (and/or use of a multigene panel that includes PMM2) fails to confirm a diagnosis in an individual with features of PMM2-CDG (CDG-Ia).
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 1.
Molecular Genetic Testing Used in PMM2-CDG (CDG-Ia)
| Gene 1 | Test Method | Proportion of Probands with Pathogenic Variants 2 Detectable by This Method 3 |
|---|---|---|
| PMM2 | Sequence analysis 4 | ~100% 5 |
| Gene-targeted deletion/duplication analysis 6 | Unknown 7 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on allelic variants detected in this gene.
- 3.
Individuals with either an abnormal transferrin isoform pattern on analysis of serum transferrin glycoforms or enzymatically confirmed phosphomannomutase 2 deficiency [Jaeken et al 2014] (full text)
- 4.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 5.
Jaeken et al [2014]
- 6.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include: quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 7.
A 28-kb deletion that includes exon 8 as well as other novel exon or whole-deletions has been reported [Schollen et al 2007].
Phosphomannomutase 2 (PMM2) enzyme activity. In individuals presenting with a severe/classic clinical picture of PMM2-CDG (CDG-Ia), PMM2 enzyme activity in fibroblasts and leukocytes is typically 0% to 10% of normal [Van Schaftingen & Jaeken 1995, Carchon et al 1999, Jaeken & Carchon 2001]. If measurement of enzyme activity is used to verify the diagnosis, use of leukocytes is preferable given that intermediate enzyme activity values (including values in the normal range) in fibroblasts have been reported [Grünewald 2009].
Clinical Characteristics
Clinical Description
The typical clinical course of PMM2-CDG (CDG-Ia) has been divided into an infantile multisystem type, late-infantile and childhood ataxia-intellectual disability type, and adult stable disability type. Recent reports have widened the phenotypic spectrum to include hydrops fetalis at the severe end [van de Kamp et al 2007] and a mild neurologic phenotype in adults with multisystem involvement at the mild end [Barone et al 2007, Coman et al 2007, Grünewald 2009].
Infantile Multisystem Type
Historically, PMM2-CDG (CDG-Ia) was characterized by cerebellar hypoplasia, facial dysmorphism, psychomotor retardation, and abnormal subcutaneous fat distribution; however, the clinical phenotype continues to broaden.
Infants show axial hypotonia, hyporeflexia, esotropia, and developmental delay. Feeding problems and vomiting may cause severe failure to thrive. Growth is significantly impaired [Kjaergaard et al 2002]. Although distinctive facies (high nasal bridge and prominent jaw) and large ears have been reported in the northern European population, these features have not been emphasized in reports of affected individuals in the US [Krasnewich & Gahl 1997, Enns et al 2002]. An unusual distribution of subcutaneous fat over the buttocks and the suprapubic region may be observed. In girls, the labia majora are involved as well. Inverted nipples are common.
In one large study, two distinct clinical presentations were observed [de Lonlay et al 2001]:
- A purely neurologic form with strabismus, psychomotor retardation, and cerebellar hypoplasia early on, and neuropathy and retinitis pigmentosa in the first or second decade. This form was not fatal.
- A neurologic-multivisceral form in which manifestations occur early in life. All organs with the exception of the lungs can be involved. Hepatic fibrosis and renal hyperechogenicity are consistent. Some infants have hepatopathy, pericardial effusion, nephrotic syndrome, renal cysts, and multiorgan failure. Approximately 20% of affected infants die within the first year of life from failure to thrive, hypoalbuminemia, and aspiration pneumonia in what is called the "infantile catastrophic phase" characterized by intractable hypoalbuminemia, anasarca, and respiratory distress [de Lonlay et al 2001, Marquardt & Denecke 2003]. Strabismus and cerebellar hypoplasia are occasionally absent.
Note: The relatively specific findings of PMM2-CDG (CDG-Ia) including dysmorphic features, inverted nipples, and abnormal fat pads may disappear with age and are occasionally absent in milder cases [Funke et al 2013].
Congenital cardiac anomalies, hypertrophic cardiomyopathy with transient myocardial ischemia, or cardiac effusions have been reported but are rare [Kristiansson et al 1998, Marquardt et al 2002, Romano et al 2009]. Pericardial effusions are typically without clinical sequelae and usually disappear in a year or two; however, persistent pericardial effusions have been seen in a few more medically involved cases, and have resulted in death in one individual [Truin et al 2008].
Liver function measurements begin to rise in the first year of life. Transaminases (AST and ALT) in young children may be in the range of 1,000 to 1,500 without clinical sequelae. Typically, the ALT and AST return to normal by age three to five years in children with PMM2-CDG (CDG-Ia) and remain normal throughout their lives with occasional mild elevations during intercurrent illnesses. These children do not need a liver biopsy unless warranted by additional clinical evidence. Liver biopsy can demonstrate lamellar inclusions in macrophages and in hepatocyte lysosomes but not in Kupffer cell lysosomes [Jaeken & Matthijs 2001].
In general, children with PMM2-CDG (CDG-Ia) are chemically euthyroid [Miller & Freeze 2003]. Note that measurement of thyroid binding globulin (TBG) may be low and thyroid stimulating hormone (TSH) may be transiently high. Free T4 should also be measured, as clinically relevant hypothyroidism in PMM2-CDG (CDG-Ia) is rare [Mohamed et al 2012].
Seizures, which are usually responsive to antiepileptic drugs, are common. In one study of 23 affected individuals who had seizures, the mean age of the first seizure was 17 months (range: 3-53 months) [Pérez-Dueñas et al 2009].
Renal ultrasound examination in eight infants and children with PMM2-CDG (CDG-Ia) showed no changes in the two with the neurologic form and increased cortical echogenicity and/or small pyramids that may or may not have been hyperechoic in the six with the multivisceral form [Hertz-Pannier et al 2006]. Nephrotic syndrome is rare but has been reported [Sinha et al 2009].
Sibs with PMM2-CDG (CDG-Ia) have been reported with immunologic dysfunction / diminished chemotaxis of neutrophils and poor immune response to vaccinations [Blank et al 2006].
One child with PMM2-CDG (CDG-Ia) and a skeletal dysplasia, characterized by flattening of all vertebrae (platyspondyly), had severe spinal cord compression at the level of the craniocervical junction [Schade van Westrum et al 2006].
Osteopenia, seen on x-ray and also documented by densitometry, is common and remains throughout life.
Lymphatic edema due to abnormal lymphatic vessel development has been described [Verstegen et al 2012]. Note that this differs from the generalized edema resulting from hypoalbuminemia.
Late-Infantile and Childhood Ataxia-Intellectual Disability Type
Late-infantile and childhood ataxia-intellectual disability type occurs between ages three and ten years. Children have a more static course characterized by hypotonia and ataxia. Language and motor development are delayed and walking without support is rarely achieved [Jaeken & Matthijs 2001]. IQ typically ranges from 40 to 70. As the spectrum of PMM2-CDG (CDG-Ia) expands, individuals with borderline and even normal development have been described [Giurgea et al 2005, Pancho et al 2005, Barone et al 2007]. The children usually are extroverted and cheerful. Seizures may occur; they are usually responsive to antiepileptic drugs.
In this type and in adulthood, affected individuals may have stroke-like episodes or transient unilateral loss of function sometimes associated with fever, seizure, dehydration, or trauma. Recovery may occur over a few weeks to several months. Persistent neurologic deficits after a stroke-like episode occasionally occur but are rare. The etiology of these stroke-like episodes has not been fully elucidated. In one person, brain MRI demonstrated different findings after two such episodes, the first an ischemic process and the second edema with subsequent focal necrosis [Ishikawa et al 2009].
Intracranial hemorrhage, while not common, has been described [Stefanits et al 2014].
A progressive peripheral neuropathy may begin in this age range.
Retinitis pigmentosa due to a progressive photoreceptor degeneration [Thompson et al 2013], myopia [Jensen et al 2003], cataract [Morava et al 2009], joint contractures, and skeletal deformities may also occur.
Adult Stable Disability Type
Adults with PMM2-CDG (CDG-Ia) typically demonstrate stable rather than progressive intellectual disability and variable peripheral neuropathy.
Progression of thoracic and spinal deformities can result in severe kyphoscoliosis. Osteopenia and osteoporosis are common in adults [Monin et al 2014].
Previously undiagnosed individuals are now being identified as adults because of multisystem involvement and cerebellar ataxia [Schoffer et al 2006, Barone et al 2007]. Additionally the mild end of the adult phenotypic spectrum has expanded to include normal cognitive abilities; of three affected sibs, all had multisystem involvement, one with significant cognitive impairment and two with normal cognition [Stibler et al 1994, Jaeken & Matthijs 2001, Coman et al 2007, Krasnewich et al 2007].
Women lack secondary sexual development as a result of hypogonadotropic hypogonadism [de Zegher & Jaeken 1995, Kristiansson et al 1995, Miller & Freeze 2003]. In some females, laparoscopy and ultrasound examination have revealed absent ovaries. Males virilize normally at puberty but may exhibit decreased testicular volume.
Other endocrine dysfunction includes hyperglycemia-induced growth hormone release, hyperprolactinemia, insulin resistance, and hyperinsulinemic hypoglycemia [Miller & Freeze 2003, Shanti et al 2009]. Glycosylation and resultant function of IGFBP3 and an acid-labile subunit (ALS) in the IGF pathway are impaired in CDG [Miller et al 2009].
Coagulopathy with decreased serum concentrations of factors IV, IX, and XI, antithrombin III, protein C, and protein S may be present. Deep venous thrombosis in adults has been reported [Krasnewich et al 2007].
Renal microcysts may be identified on renal ultrasound examination but renal function is typically preserved throughout adulthood [Strøm et al 1993].
Neuroimaging. An enlarged cisterna magna and superior cerebellar cistern is observed in late infancy to early childhood. Occasionally, both infratentorial and supratentorial changes compatible with atrophy are present. Dandy-Walker malformations and small white matter cysts have been reported [Peters et al 2002].
Myelination varies from normal to delayed or insufficient [Holzbach et al 1995].
Serial CTs performed on three children with PMM2-CDG (CDG-Ia) revealed that enlargement of the spaces between the folia of the cerebellar hemispheres, especially from the anterior to the posterior aspect, as well as atrophy of the anterior vermis, appeared to progress until around age five years [Akaboshi et al 1995]. Progression of cerebellar atrophy on MRI after age five years is variable. After age nine years, cerebellar atrophy did not appear to progress. Development of the supratentorial structures was normal.
Pathophysiology
PMM2-CDG (CDG-Ia) is caused by deficiency of phosphomannomutase 2 (PMM2) enzyme activity resulting in the defective synthesis of N-linked oligosaccharides, sugars linked together in a specific pattern and attached to proteins and lipids (N-linked glycans link to the amide group of asparagine via an N-acetylglucosamine residue) [Jaeken & Matthijs 2001, Grunewald et al 2002]. Because of the important biologic functions of the oligosaccharides in both glycoproteins and glycolipids, incorrect synthesis of these compounds results in multisystem clinical manifestations [Varki 1993, Freeze 2006].
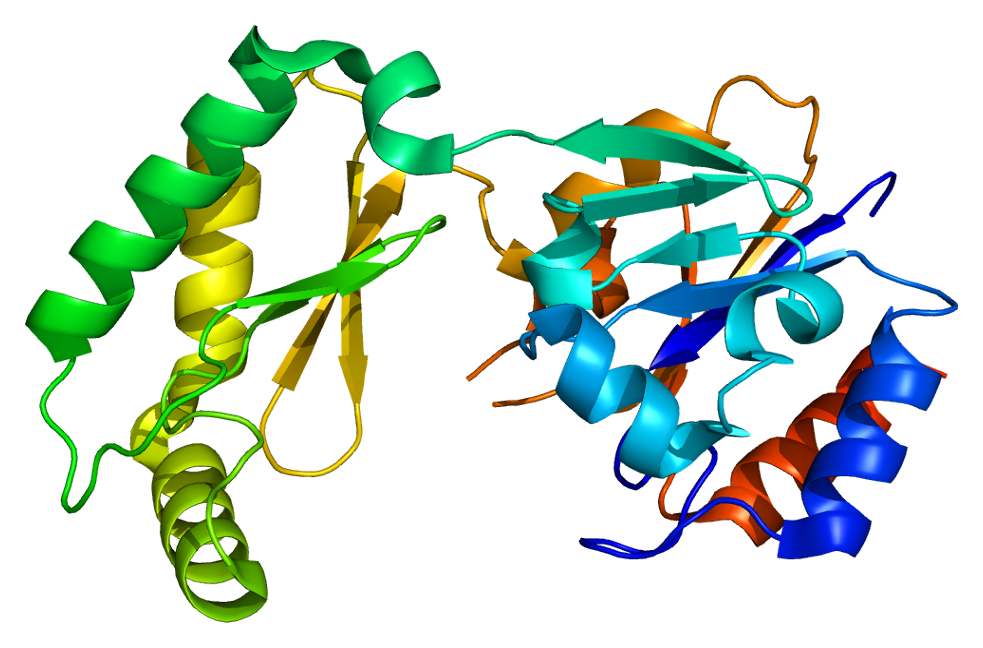
See Figure 1.

Figure 1.
N-linked glycans are synthesized by adding individual charged sugars in a specific order to the growing multi-sugar structure, or oligosaccharide. The enzyme PMM2 is required for synthesis of one of these charged sugars, mannose-1-phosphate (man-1-P) (more...)
Genotype-Phenotype Correlations
Lack of correlation between genotype and phenotype in PMM2-CDG (CDG-Ia) has been reported [Erlandson et al 2001, Jaeken & Matthijs 2001, Westphal et al 2001]. In general, individuals with all genotypes show the basic signs of the disorder; i.e., developmental delay, cerebellar atrophy, peripheral neuropathy, stroke-like episodes or comatose episodes, epilepsy, retinal pigmentary degeneration, strabismus, skeletal abnormalities, and hepatopathy. However, the extent of the non-neurologic findings varies depending on the genotype:
- C-terminal pathogenic variants, including p.His218Leu, p.Thr237Met, and p.Cys241Ser, may be associated with a milder phenotype [Matthijs et al 1999, Tayebi et al 2002].
- The phenotypic spectrum of the [p.Arg141His]+[p.Phe119Leu] genotype, the most prevalent genotype in PMM2-CDG (CDG-Ia), was studied in Scandinavia [Kjaergaard et al 2001]. Individuals with the [p.Arg141His]+[p.Phe119Leu] genotype probably represent the severe end of the clinical spectrum of CDG-Ia. Presentation was uniformly early with severe feeding problems, severe failure to thrive, severe hypotonia, developmental delay obvious before age six months, and hepatic dysfunction. Asymptomatic pericardial effusions were common in the first year of life. The functional outcome in ambulation and speech was variable.
- A severe phenotype presenting with a high mortality rate was observed with the [p.Asp188Gly]+[p.Arg141His] genotype: in the study by Matthijs et al [1998], four of five children with this genotype died before age two years. The remaining child, age ten years, was severely affected.
- de Lonlay et al [2001] reported several compound heterozygous genotypes (including [p.Arg141His]+[ p.Thr226Ser], [p.Arg141His]+[p.Ile132Thr], and [p.Arg141His]+[p.Glu139Lys]) that appear to be associated with a milder phenotype termed the "neurologic form" without pericardial effusions, coagulation defects, or nutritional disturbances. Some individuals are able to walk independently.
- The pathogenic variant p.Val231Met is associated with high early mortality and severe multiorgan insufficiency.
- Homozygosity or compound heterozygosity for pathogenic variants with virtually no residual activity (e.g., p.Arg141His) is likely incompatible with life [Matthijs et al 2000].
- The pathogenic variant p.Leu32Arg, which is particularly frequent in Italy, is associated with a milder phenotype with preserved ambulation and mild cognitive impairment despite cerebellar hypoplasia on brain MRI [Barone et al 2015].
- A relatively common mild ALG6 variant (p.Phe304Ser) in combination with confirmed PMM2-CDG (CDG-Ia) may exacerbate the clinical severity in PMM2-CDG (CDG-Ia); however, this information cannot currently be used to predict clinical outcome [Westphal et al 2002, Bortot et al 2013].
Nomenclature
In 2009 the nomenclature for all types of CDG was changed to include the official gene symbol (not in italics) followed by "-CDG." If the type has a known letter name, it follows in parenthesis; thus the new nomenclature for this disorder is PMM2-CDG (CDG-Ia) [Jaeken et al 2009].
PMM2-CDG was previously referred to as CDGS1a; carbohydrate-deficient glycoprotein syndrome, type 1a; and Jaeken syndrome.
Prevalence
PMM2-CDG (CDG-Ia) is the most common form of congenital disorders of glycosylation. The prevalence could be as high as 1:20,000 [Jaeken & Matthijs 2001].
The expected carrier frequency for a PMM2 pathogenic variant in the Danish population is 1:60 to 1:79 [Matthijs et al 2000].
Differential Diagnosis
Any child with evidence of coagulopathy, hepatopathy, elevated thyroid stimulating hormone (TSH), or cerebellar hypoplasia and the triad of hypotonia, developmental delay, and failure to thrive should be evaluated for PMM2-CDG (CDG-Ia).
Other genetic disorders to consider in the differential diagnosis
- Prader-Willi syndrome
- Congenital muscular dystrophies including Fukuyama congenital muscular dystrophy (FCMD) caused by mutation of FKTN, muscle-eye-brain (MEB) disease caused by mutation of POMGNT1 [Yoshida et al 2001, Martin & Freeze 2003], and Walker-Warburg syndrome, caused by mutation of POMT1
- Congenital myopathies (e.g., X-linked myotubular myopathy, multiminicore disease [OMIM 606210, 180901])
Many metabolic and genetic disorders that present in infancy share at least some of the clinical features of PMM2-CDG (CDG-Ia). The following metabolic disorders are in the differential diagnosis of hypotonia, developmental delay, and failure to thrive:
- Mitochondrial disorders (see Mitochondrial Disorders Overview)
- Peroxisome biogenesis disorders, Zellweger syndrome spectrum
- Urea cycle defects (see Urea Cycle Disorders Overview)
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with PMM2-CDG (CDG-Ia) the following evaluations are recommended [Jaeken & Carchon 2001, Jaeken & Matthijs 2001, Grunewald et al 2002, Kjaergaard et al 2002, Miller & Freeze 2003, Grünewald 2009]:
- Liver function tests
- Measurement of serum albumin concentration
- Thyroid function tests to evaluate for decreased thyroid binding globulin, elevated serum concentration of TSH, and low serum concentration of free T4
- Coagulation studies including protein C, protein S, antithrombin III, and factor IX
- Urinalysis to evaluate for proteinuria
- Measurement of serum concentration of gonadotropins in adolescent and adult women to look for evidence of hypogonadotropic hypogonadism
- Echocardiogram to evaluate for pericardial effusions
- Renal ultrasound examination to evaluate for microcysts
- Formal ophthalmologic evaluation since ocular anomalies are frequent and can involve both the structural components (development of the lens and retina) as well as ocular mobility and intraocular pressure [Morava et al 2009, Thompson et al 2013]
- Consultation with a clinical geneticist and/or genetic counselor with inclusion in a multidisciplinary team if needed
Treatment of Manifestations
Failure to thrive. Infants and children can be nourished with any type of formula for maximal caloric intake. They can tolerate carbohydrates, fats, and protein. Early in life, children may do better on elemental formulas. Their feeding may be advanced based on their oral motor function. Some children require placement of a nasogastric tube or gastrostomy tube for nutritional support until oral motor skills improve.
Oral motor dysfunction with persistent vomiting. Thickening of feeds, maintenance of an upright position after eating, and antacids can help children who experience gastroesophageal reflux and/or persistent vomiting. Consultation with a gastroenterologist and nutritionist is often necessary. Children with a gastrostomy tube should be encouraged to eat by mouth if the risk of aspiration is low. Continued speech therapy and oral motor therapy aid transition to oral feeds and encourage speech when the child is developmentally ready.
Developmental delay. Occupational therapy, physical therapy, and speech therapy should be instituted. As the developmental gap widens between children with PMM2-CDG (CDG-Ia) and their unaffected peers, parents need continued counseling and support.
"Infantile catastrophic phase." Very rarely, infants may have a complicated early course presenting with infection or seizure and hypoalbuminemia with third spacing that may progress to anasarca. Some children are responsive to aggressive albumin replacement with lasix, others may have a more refractory course. Symptomatic treatment in a pediatric tertiary care center is recommended. Parents should also be advised that some infants with PMM2-CDG (CDG-Ia) never experience a hospital visit while others may require frequent hospitalizations.
Strabismus. Intervention by a pediatric ophthalmologist early in life is important to preserve vision through glasses, patching, or surgery.
Hypothyroidism. Thyroid function tests are frequently abnormal in children with PMM2-CDG (CDG-Ia). However, free thyroxine analyzed by equilibrium dialysis, the most accurate method, has been reported as normal in seven individuals with PMM2-CDG (CDG-Ia). Diagnosis of hypothyroidism and L-thyroxine supplementation should be reserved for those children and adults with elevated TSH and low free thyroxine measured by equilibrium dialysis.
Stroke-like episodes. Supportive therapy includes hydration by IV if necessary and physical therapy during the recovery period.
Coagulopathy. Low levels of coagulation factors, both pro- and anti-coagulant, rarely cause clinical problems in daily activities but must be acknowledged if an individual with PMM2-CDG (CDG-Ia) undergoes surgery. Consultation with a hematologist (to document the coagulation status and factor levels) and discussion with the surgeon are important. When necessary, infusion of fresh frozen plasma corrects the factor deficiency and clinical bleeding. The potential for imbalance of the level of both pro- and anti-coagulant factors may lead to either bleeding or thrombosis. Caregivers, especially of older affected individuals, should be taught the signs of deep venous thrombosis.
Osteopenia. While present from infancy there does not appear to be a significant increased risk of fracture. Should fracture occur, management should follow standards of medical care.
Additional management issues of adults with PMM2-CDG (CDG-Ia)
Orthopedic issues – thorax shortening, scoliosis/kyphosis. Management involves appropriate orthopedic and physical medicine management, well-supported wheelchairs, appropriate transfer devices for the home, and physical therapy. Occasionally, surgical treatment of spinal curvature is warranted.
Deep venous thrombosis (DVT). DVT has been reported in two adults with PMM2-CDG (CDG-Ia). Rapid diagnosis and treatment of DVT are essential to minimize the risk of pulmonary emboli; sedentary affected adults and children are at increased risk for DVT.
Independent living issues. Young adults with PMM2-CDG (CDG-Ia) and their parents need to address issues of independent living. Aggressive education throughout the school years in functional life skills and/or vocational training helps the transition when schooling is completed. Independence in self-care and the activities of daily living should be encouraged. Support and resources for parents of a disabled adult are an important part of management.
Prevention of Secondary Complications
Because infants with PMM2-CDG (CDG-Ia) have less physiologic reserve than their peers, parents should have a low threshold for evaluation by a physician for prolonged fever, vomiting, or diarrhea. Aggressive intervention with antipyretics, antibiotics if warranted, and hydration may prevent the morbidity associated with the "infantile catastrophic phase."
Although only one individual with skeletal dysplasia in PMM2-CDG (CDG-Ia) has been reported, plain spine films assessing cervical spine anomalies may be useful [Schade van Westrum et al 2006].
Surveillance
Annual
- Assessment by a physician with attention to overall health and referral for speech therapy, occupational therapy, and physical therapy
- Eye examination
- Liver function tests, thyroid panel, protein C, protein S, factor IX, and antithrombin III
Other
- Periodic assessment of bleeding and clotting parameters by a hematologist
- Monitoring for osteopenia/osteoporosis and counseling about the risk of fractures
- Follow up with an orthopedist when scoliosis becomes evident
Agents/Circumstances to Avoid
Acetaminophen and other agents metabolized by the liver should be used with caution.
Evaluation of Relatives at Risk
See Genetic Counseling for issues related to testing of at-risk relatives for genetic counseling purposes.
Therapies Under Investigation
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for access to information on clinical studies for a wide range of diseases and conditions. Note: There may not be clinical trials for this disorder.