Telangiectasia, Hereditary Hemorrhagic, Type 5
A number sign (#) is used with this entry because of evidence that hereditary hemorrhagic telangiectasia type 5 (HHT5) is caused by heterozygous mutation in the GDF2 gene (605120) on chromosome 10q11.
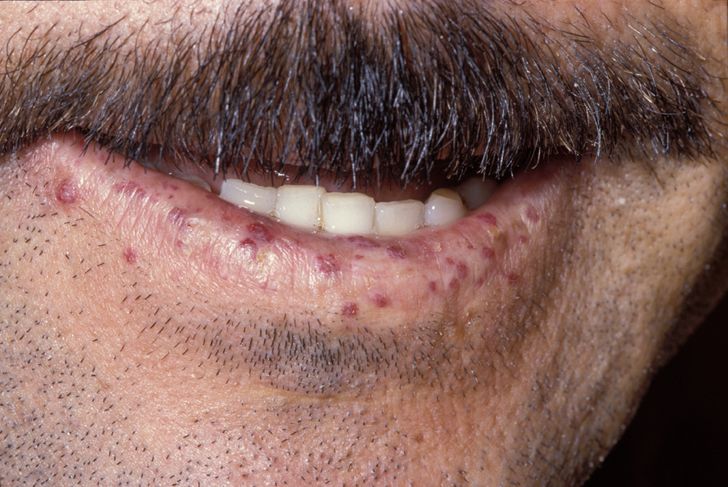
DescriptionHereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant syndrome characterized by telangiectases and arteriovenous malformations (AVMs). Hallmark features are recurrent epistaxis due to telangiectases of the nasal mucosa; telangiectases on the lips, hands, and oral mucosa; solid-organ AVMs, particularly of the lungs, liver, and brain; and a family history of the same. Presentation with 3 of these criteria is considered diagnostic for HHT (summary by Wooderchak-Donahue et al., 2013).
Clinical FeaturesWooderchak-Donahue et al. (2013) studied 3 individuals with features of hereditary hemorrhagic telangiectasia. The first patient was a 33-year-old woman who had onset of epistaxis in early childhood, with approximately 3 episodes a week in adulthood. She had several cutaneous telangiectases on her chest and face. Her father had died suddenly at 45 years of age and was suspected to have had HHT on the basis of autopsy findings, and a sib had recurrent spontaneous nosebleeds and stroke of unknown etiology at 43 years of age. Family members were unavailable for study. The second patient was a 37-year-old woman with onset of epistaxis at 30 years of age, with episodes varying from daily to once every 1 to 2 weeks. She had 15 to 20 dermal vascular malformations on her face, mouth, upper chest, upper mid-back area, and hands. She reported that the larger malformation had faded from a darker to a lighter pink over time. MRI of the brain did not show arteriovenous malformations (AVMs). However, hepatic MRI in this patient, who had abnormal liver enzymes and portal hypertension and had also been diagnosed with hepatopulmonary syndrome, showed vascular findings similar to those seen in HHT, with a slightly heterogeneous arterial phase and prominent, slightly corkscrew smaller branches of the hepatic artery as well as a suggestion of small focal nodular hyperplasia. Her father and sister had infrequent but recurring nosebleeds, but were not available for examination. The third patient was a 14-year-old boy who had onset of epistaxis at 3 years of age, with frequency ranging from once per week to several times per day. He had 80 to 100 telangiectases on his left arm, 2 on the palm of his right hand, and 1 possible lesion on his lower lip; biopsy report confirmed the lesions to be telangiectases. His father reportedly had frequent nosebleeds from childhood to early teens, but was unavailable for study. The first and third patients were not screened for solid organ involvement.
Molecular GeneticsWooderchak-Donahue et al. (2013) performed exome sequencing in 38 unrelated patients who had been diagnosed with HHT, but in whom no mutations were found in the 3 known HHT-associated genes (ENG, 131195; ACVRL1, 601284; SMAD4, 600993), and identified heterozygosity for pathogenic missense variants in the GDF2 gene (605120.0001; 605120.0002) in 2 patients. Sanger sequencing of GDF2 in another 153 unrelated individuals with a suspected diagnosis of HHT revealed 1 more patient with a heterozygous missense mutation (605120.0003). All 3 mutation-positive individuals had epistaxis and dermal lesions described as telangiectases; however, Wooderchak-Donahue et al. (2013) noted that the skin lesions in these patients were less concentrated on the hands and mouth than in individuals with mutations in other HHT-associated genes, and some lesions were more similar in size and shape to the 'atypical capillary malformation' seen in CMAVM (608354), or had a distribution more typical of telangiectases seen in CMAVM.