Williams Syndrome
Summary
Clinical characteristics.
Williams syndrome (WS) is characterized by cardiovascular disease (elastin arteriopathy, peripheral pulmonary stenosis, supravalvar aortic stenosis, hypertension), distinctive facies, connective tissue abnormalities, intellectual disability (usually mild), a specific cognitive profile, unique personality characteristics, growth abnormalities, and endocrine abnormalities (hypercalcemia, hypercalciuria, hypothyroidism, and early puberty). Feeding difficulties often lead to poor weight gain in infancy. Hypotonia and hyperextensible joints can result in delayed attainment of motor milestones.
Diagnosis/testing.
Clinical diagnostic criteria are available for Williams syndrome; however, the diagnosis requires detection of a recurrent 7q11.23 contiguous gene deletion of the Williams-Beuren syndrome critical region (WBSCR) that encompasses the elastin gene (ELN). This contiguous gene deletion can be detected using fluorescent in situ hybridization (FISH) and/or deletion/duplication testing.
Management.
Treatment of manifestations: Early intervention programs, special education programs, and vocational training address developmental disabilities; programs include speech/language, physical, occupational, feeding, and sensory integration therapies. Psychological and psychiatric evaluation and treatment provide individualized behavioral counseling and medications, especially for attention deficit disorder and anxiety. Surgery may be required for supravalvar aortic or pulmonary artery stenosis, mitral valve insufficiency, and/or renal artery stenosis. Treatment of hypercalcemia may include diet modification, oral corticosteroids, and/or intravenous pamidronate. Refer to a nephrologist for management of nephrocalcinosis, persistent hypercalcemia, and/or hypercalciuria. Treatment of hypertension, hyperopia, and recurrent otitis media does not differ from that in the general population. Orthodontic referral should be considered for malocclusion. Infants with feeding problems may benefit from feeding therapy. Constipation should be aggressively managed at all ages. Early puberty may be treated with a gonadotropin-releasing hormone agonist.
Prevention of secondary complications: Range of motion exercises to prevent or ameliorate joint contractures; anesthesia consultation and electrocardiogram prior to sedation and surgical procedures.
Surveillance: Annual medical evaluation, vision screening, hearing evaluation, measurement of blood pressure in both arms, calcium/creatinine ratio in spot urine, and urinalysis. Children younger than age two years should have serum calcium studies every four to six months. Thyroid function should be checked yearly until age three years and every two years thereafter. Additional periodic evaluations for all individuals include: measurement of serum concentration of calcium every two years; cardiology evaluation for elastin arteriopathy at least annually for the first five years and every two to three years thereafter for life; and renal and bladder ultrasound examination every ten years. Additional periodic evaluations during adulthood include: oral glucose tolerance; cardiac evaluation for mitral valve prolapse, aortic insufficiency, hypertension, long QT interval, and arterial stenoses; and ophthalmologic evaluation for cataracts.
Agents/circumstances to avoid: Multivitamins for children because all pediatric multivitamin preparations contain vitamin D.
Genetic counseling.
Williams syndrome is transmitted in an autosomal dominant manner. Most cases are de novo occurrences, but occasionally, parent-to-child transmission is observed. Prenatal testing is possible but is rarely used because most cases occur in a single family member only, and no prenatal indicators exist for low-risk pregnancies.
Diagnosis
Clinical diagnostic criteria are available for Williams syndrome (WS) [Preus 1984, Committee on Genetics 2001, Committee on Genetics 2002].
The WS phenotype is variable, and no single clinical feature is required to establish the diagnosis.
Suggestive Findings
Williams syndrome (WS) should be suspected in individuals with the following findings:
- Cardiovascular disease (elastin arteriopathy). Any artery may be narrowed. Supravalvar aortic stenosis (SVAS) is the most clinically significant and most common cardiovascular finding, occurring in 75% of affected individuals. Peripheral pulmonic stenosis (PPS) is common in infancy.
- Distinctive facies. Broad forehead, bitemporal narrowing, periorbital fullness, a stellate/lacy iris pattern (Figure 1), strabismus, short nose, broad nasal tip, malar flattening, long philtrum, thick vermilion of the upper and lower lips, wide mouth, malocclusion, small jaw, and large ear lobes are observed at all ages (Figure 2). Young children have epicanthal folds, full cheeks, and small, widely spaced teeth (Figure 3), while adults typically have a long face and neck, accentuated by sloping shoulders, resulting in a more gaunt appearance (Figure 4).
- Connective tissue abnormalities. Hoarse voice, inguinal/umbilical hernia, bowel/bladder diverticulae, rectal prolapse, joint limitation or laxity, and soft, lax skin are observed.
- Intellectual disability. Most individuals have some degree of intellectual disability, which can range from severe to mild. Some have average intelligence.
- Specific cognitive profile. Strengths in verbal short-term memory and language and extreme weakness in visuospatial construction are typical. The Williams syndrome cognitive profile is independent of IQ.
- Unique personality. Overfriendliness, empathy, generalized anxiety, specific phobias, and attention deficit disorder are commonly observed.
- Growth abnormalities. The growth pattern is characterized by: prenatal growth deficiency, failure to thrive in infancy (70%), poor weight gain and linear growth in the first four years; a rate of linear growth that is 75% of normal in childhood; and a brief pubertal growth spurt. The mean adult height is below the third centile.
- Endocrine abnormalities. Findings include idiopathic hypercalcemia, hypercalciuria, hypothyroidism, subclinical hypothyroidism, and early puberty. An increased frequency of abnormal oral glucose tolerance tests, obesity, and diabetes mellitus is observed, especially in adults.

Figure 1.
Note the stellate iris pattern in an individual with Williams syndrome.

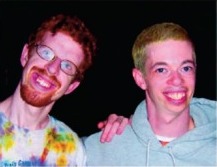
Figure 2.
A broad forehead, bitemporal narrowing, periorbital fullness, strabismus, short nose, broad nasal tip, malar flattening, long philtrum, thick vermilion of the upper and lower lips, wide mouth, malocclusion, small jaw, and large earlobes are observed at (more...)

Figure 3.
Young children with Williams syndrome typically have epicanthal folds, full cheeks, and small, widely spaced teeth as seen in these children at the following ages: A. Newborn

Figure 4.
Adults typically have a long face and neck, accentuated by sloping shoulders, resulting in a gaunt appearance, as seen in this affected individual, age 43 years.
Note: See the National Human Genome Research Institute (NHGRI) Atlas of Human Malformation Syndromes (scroll to ATLAS IMAGES) for photographs of individuals with Williams syndrome from diverse ethnic backgrounds.
Establishing the Diagnosis
The diagnosis of Williams syndrome (WS) is established by detection of the 1.5-1.8-Mb heterozygous microdeletion at chromosome 7q11.23. For this GeneReview, WS is defined as the presence of this recurrent 1.5-1.8-Mb deletion at the approximate position of chr7:72,744,454-74,142,513 in the reference genome (NCBI Build GRCh37/hg19).
Note: The phenotype of significantly larger or smaller deletions within this region may be clinically distinct from WS (see Genetically Related Disorders).
Although several genes of interest (e.g., ELN) are within the 1.5-1.8-Mb recurrent microdeletion, no single gene in which pathogenic variants are causative of WS has been identified (see Molecular Genetics for genes of interest in the deleted region).
Genomic testing methods that determine the copy number of sequences can include chromosomal microarray (CMA) or targeted deletion analysis by fluorescence in situ hybridization (FISH). Note: WS cannot be identified by routine analysis of G-banded chromosomes or other conventional cytogenetic banding techniques.
- Chromosomal microarray (CMA) using oligonucleotide arrays or SNP genotyping arrays can detect the recurrent deletion in a proband. The ability to size the deletion depends on the type of microarray used and the density of probes in the 7q11.23 region.Note: (1) Most individuals with WS are identified by CMA performed in the context of developmental delay, intellectual disability, or autism spectrum disorders. (2) The recurrent deletion was detected by early arrays (e.g., BAC arrays).
- Targeted deletion analysis. A FISH probe targeted to the 7q11.23 region can be reliably used for diagnosis in situations where CMA is not available. FISH analysis may be used to test at-risk relatives of a proband known to have WS. Note: (1) Targeted deletion testing by FISH is not appropriate for the relative of an individual suspected of having WS in whom a deletion was not detected by FISH or by CMA designed to target 7q11.23. BY definition, such individuals do not have WS. (2) It is not possible to size the microdeletion routinely by use of FISH.
Table 1.
Genomic Testing Used in Williams Syndrome
| Deletion 1 | ISCA ID 2 | Region Location 3, 4 | Method | Sensitivity | |
|---|---|---|---|---|---|
| Proband | At-risk family members | ||||
| 1.5-1.8-Mb heterozygous deletion at 7q11.23 | ISCA-37392 | GRCh37/hg19 chr7: 72,744,454-74,142,513 | CMA 5 | 100% | 100% |
| FISH | 100% | 100% 6 | |||
- 1.
See Molecular Genetics for details of the deletion.
- 2.
Standardized clinical annotation and interpretation for genomic variants from the Clinical Genome Resource (ClinGen) project (formerly the International Standards for Cytogenomic Arrays (ISCA) Consortium)
- 3.
Genomic coordinates represent the minimum deletion size associated with the 7q11.23 recurrent microdeletion as designated by ClinGen. Deletion coordinates may vary slightly based on array design used by the testing laboratory. Note that the size of the microdeletion as calculated from these genomic positions may differ from the expected microdeletion size due to the presence of segmental duplications near breakpoints. The phenotype of significantly larger or smaller microdeletions within this region may be clinically distinct from the recurrent 7q11.23 microdeletion (see Genetically Related Disorders).
- 4.
See Molecular Genetics for genes of interest included in this region.
- 5.
Chromosomal microarray analysis (CMA) using oligonucleotide arrays or SNP genotyping arrays. CMA designs in current clinical use target the 7q11.23 region.
- 6.
FISH is not appropriate as a diagnostic method for the relative of an affected individual in whom Williams syndrome was not detected by FISH or by CMA designed to target this region.
Evaluating at-risk relatives. FISH can be used to identify Williams syndrome in at-risk relatives of the proband. Testing of parental samples is indicated only if the relative has signs or symptoms of Williams syndrome (see Genetic Counseling).
Clinical Characteristics
Clinical Description
Infancy. The infant with Williams syndrome (WS) is often born post-term and is small for the family background. Feeding difficulties leading to failure to gain weight are common, including gastroesophageal (G-E) reflux, disordered suck and swallow, textural aversion, and vomiting. Prolonged colic (>4 months) may be related to G-E reflux, chronic constipation, and/or idiopathic hypercalcemia. Other medical problems that often occur in the first year include strabismus, chronic otitis media, rectal prolapse, umbilical and/or inguinal hernia, and cardiovascular disease [Morris et al 1988]. Infants with WS are hypotonic and typically have hyperextensible joints, resulting in delayed attainment of motor milestones. Walking usually occurs by age 24 months. Speech is also delayed but later becomes a relative strength. Fine motor difficulties are present at all ages.
Cognitive abilities. Intellectual disability, usually mild, occurs in 75% of individuals with WS. The cognitive profile is distinctive, consisting of strengths in verbal short-term memory and language but extreme weakness in visuospatial constructive cognition [Mervis et al 2000]. As a result, children with WS usually score higher on verbal subtests than on tests measuring visuospatial construction [Greer et al 1997, Mervis et al 1998]. No gender difference in IQ is reported and the IQ is stable over time in children [Mervis et al 2012b].
Academically, individuals with WS perform relatively well in reading, and adults may read at the high school level, though the range of achievement is wide. Reading skills correlate with cognitive ability rather than language-related skills [Levy et al 2003]. Difficulty with writing, drawing, and mathematics is significant, although many adults with WS are able to perform simple addition.
Adaptive behavior is less than expected for IQ in both children and adults [Davies et al 1997, Howlin & Udwin 2006, Mervis & Pitts 2015], and adversely affects the ability of adults with WS to function independently.
Unique personality/behavior. The characteristic personality profile of WS includes overfriendliness, social disinhibition, excessive empathy, attention problems, and non-social anxiety [Einfeld et al 2001, Doyle et al 2004, Morris 2010, Muñoz et al 2010]. Other common behavior problems include difficulty with sensory modulation/sensory processing, difficulty with emotional regulation, perseveration, and specific phobias (80%) [Dykens 2003, Laws & Bishop 2004, John & Mervis 2010, Pitts et al 2016]. Some have overlapping symptoms with autism spectrum disorder, such as restricted interests and repetitive behavior [Klein-Tasman et al 2009]. Compared to other children with disabilities, children with WS rate high on measures of the following: empathy, gregariousness, people-orientation, tenseness, sensitivity, and "visibility" (easily noticed) [Klein-Tasman & Mervis 2003]. In children, attention deficit disorder occurs in 65% and anxiety disorder in 57% (usually specific phobias) [Leyfer et al 2006]. Anxiety is common across the life span; longitudinal studies of anxiety indicate a prevalence of 80% [Woodruff-Borden et al 2010].
Sleep. Sleep problems are reported in 65% and include increased sleep latency and decreased sleep efficiency [Goldman et al 2009, Mason et al 2011]. Abnormal or absent nocturnal melatonin peak has been documented in recent studies [Sniecinska-Cooper et al 2015, Santoro et al 2016].
Cardiovascular disease. Elastin arteriopathy is present in 75%-80% of affected individuals and may affect any artery [Morris et al 1988, Pober et al 2008, Del Pasqua et al 2009, Collins et al 2010b].
Peripheral pulmonic stenosis (PPS) is common in infancy but usually improves over time.
The most common arteriopathy is supravalvar aortic stenosis (SVAS), which may worsen over time, especially in the first five years of life [Collins et al 2010b]. The greatest morbidity results from this aortic narrowing, which can be either a discrete hourglass stenosis or diffuse aortic stenosis. If untreated, the resultant increase in arterial resistance leads to elevated left heart pressure, cardiac hypertrophy, and cardiac failure. Middle aortic syndrome, including diffuse narrowing of the thoracic and abdominal aorta, occurs rarely but can be difficult to treat and may require reintervention [Radford & Pohlner 2000].
Individuals with combined SVAS and PPS (biventricular outflow tract obstruction) may develop biventricular hypertrophy and hypertension, increasing the risk for myocardial ischemia, dysrhythmias, and sudden death [Pham et al 2009]. Coronary artery stenosis has been implicated in some cases of sudden death in WS [Bird et al 1996]. The incidence of sudden death in one cohort of 293 individuals with WS was 1/1000 patient years, which is 25 to 100 times higher than the age-matched population [Wessel et al 2004]. Corrected QT prolongation has been reported in 13.6% of individuals with WS; screening for repolarization abnormalities is recommended [Collins et al 2010a].
Anesthesia and sedation is associated with an increased risk for adverse events including cardiac arrest in individuals with WS [Burch et al 2008, Olsen et al 2014]. Sedation and anesthesia risk assessment and management guidelines have been developed [Burch et al 2008, Matisoff et al 2015, Latham et al 2016].
The prevalence of hypertension in individuals with WS is 40%-50%. Hypertension may present at any age [Broder et al 1999, Giordano et al 2001, Eronen et al 2002, Bouchireb et al 2010] and may be secondary to renal artery stenosis in some cases [Deal et al 1992]. Increased vascular stiffness has been documented in WS and responds to antihypertensive medication [Kozel et al 2014].
Mitral valve prolapse and aortic insufficiency have been reported in adults [Morris et al 1990, Kececioglu et al 1993, Collins et al 2010a].
Stenosis of the mesenteric arteries may contribute to abdominal pain.
Neurovascular abnormalities are rarely reported but may result in stroke [Ardinger et al 1994, Soper et al 1995, Cherniske et al 2004].
Eye, ear, nose, and throat. Lacrimal duct obstruction, hyperopia (67%), and strabismus (~50%) are common in individuals with WS [Kapp et al 1995, Weber et al 2014]. Cataracts have been reported in adults [Cherniske et al 2004].
Chronic otitis media is seen in 50% of affected individuals. Increased sensitivity to sound is common (90%), and individuals with WS report discomfort at 20 decibels (db) lower than controls [Gothelf et al 2006]. Many report specific phobias for certain sounds [Levitin et al 2005].
Progressive sensorineural hearing loss has been observed; mild to moderate hearing loss is detected in 63% of children and 92% of adults [Gothelf et al 2006, Marler et al 2010]. Mild to moderate high-frequency sensorineural hearing loss is common in adults, as is excessive build-up of ear wax [Cherniske et al 2004].
Most individuals have a hoarse or low-pitched voice; vocal cord abnormalities secondary to elastin deficiency are likely causative [Vaux et al 2003].
Dental problems include microdontia, enamel hypoplasia, and malocclusion [Hertzberg et al 1994]. One or more permanent teeth are missing in 40% of individuals with WS [Axelsson et al 2003].
Gastrointestinal difficulties. Individuals with WS have sensory defensiveness, both auditory [Van Borsel et al 1997] and tactile. The difficulty with food textures leads to problems in transitioning from breast milk or formula to solid foods in infancy.
Chronic abdominal pain is a common complaint of children and adults with WS; possible causes include G-E reflux, hiatal hernia, peptic ulcer disease, cholelithiasis, diverticulitis, ischemic bowel disease, chronic constipation, and somatization of anxiety. The prevalence of diverticulitis is increased in adolescents [Stagi et al 2010] and adults with WS [Partsch et al 2005]. Complications of constipation may include rectal prolapse, hemorrhoids, or intestinal perforation.
Hypercalcemia may contribute to irritability, vomiting, constipation, and muscle cramps; it is more common in infancy but may recur in adults [Morris et al 1990, Pober et al 1993].
Urinary tract abnormalities. Urinary frequency and enuresis (50%) are common in children with WS. Renal artery stenosis is found in 50% of individuals with WS, structural abnormalities of the urinary tract in 10%, bladder diverticulae in 50%, and nephrocalcinosis in fewer than 5% [Pober et al 1993, Pankau et al 1996, Sforzini et al 2002, Sammour et al 2006, Sammour et al, 2014]. Bladder capacity is reduced, and detrusor overactivity is observed in 60% [Sammour et al 2006]. Average daytime urinary continence is at age four years, nocturnal continence occurs in 50% by age ten years. Nocturnal enuresis occurs in an estimated 3% of adults [von Gontard et al 2016].
Musculoskeletal/neurologic problems. The hypotonia and lax joints of the young child lead to abnormal compensatory postures to achieve stability. Older children and adults with WS typically have hypertonia and hyperactive deep-tendon reflexes. Gradual tightening of the heel cords and hamstrings occurs, resulting in a stiff and awkward gait, kyphosis, and lordosis by adolescence [Morris et al 1988, Kaplan et al 1989]. Scoliosis is present in 18% [Morris et al 2010]. Ten percent have radioulnar synostosis [Morris & Carey 1990]. Fine motor function is impaired, leading to difficulty with tool use and handwriting at all ages.
Cerebellar signs in adults include ataxia, dysmetria, and tremor [Pober & Morris 2007].
Neuroimaging. Reduced brain size, reduced gray matter volume especially in the parietal and occipital regions, and increased gyral complexity are seen on brain MRI [Jackowski et al 2009, Eisenberg et al 2010]. Reduced posterior fossa size coupled with preserved cerebellar size may contribute to Chiari 1 malformation found in some affected individuals [Pober & Filiano 1995, Mercuri et al 1997].
Growth. Individuals with WS are short for their family background. Specific growth curves for WS are available [Morris et al 1988, Saul et al 1988, Martin et al 2007]. Poor weight gain is observed in 70% of infants. The growth pattern is characterized by prenatal growth deficiency, poor weight gain, and poor linear growth in the first four years, a rate of linear growth that is 75% of normal in childhood, and a brief pubertal growth spurt. The mean adult height is below the third centile. Obesity is a common problem in older children and adults [Cherniske et al 2004].
Puberty may occur early, and central precocious puberty is present in 18% [Partsch et al 2002]. Hormonal suppression with gonadotropin-releasing hormone is well tolerated by girls with either early or precocious puberty, and treated girls are taller than WS controls [Spielmann et al 2015].
Hypercalcemia. Idiopathic hypercalcemia occurs in 15%-50%, and is most often symptomatic (irritability, vomiting, constipation) in the first two years [Martin et al 1984, Morris et al 1988, Kim et al 2016]. Hypercalcemia is associated with dehydration, hypercalciuria, and nephrocalcinosis; compared to controls, higher median serum calcium levels are found in all age groups [Sindhar et al 2016]. The etiology of hypercalcemia in WS is unknown [Stagi et al 2016].
Endocrine problems. Endocrine abnormalities include hypothyroidism (10%), and early (though not precocious) puberty (50%) [Kim et al 2016]. Subclinical hypothyroidism (TSH elevation with normal T3/T4 levels) occurs in 31%, and occurs more frequently in children than in adults [Palacios-Verdú et al 2015]. Prevalence of impaired glucose tolerance is 26% in adolescents [Stagi et al 2014] and 63% in young adults [Masserini et al 2013]. An increased frequency of abnormal oral glucose tolerance tests and diabetes mellitus is observed in adults with WS [Cherniske et al 2004].
Other
- The hair grays prematurely [Morris et al 1988].
- Soft, lax skin is typical.
- Distinctive facial features are present and evolve with age (see Suggestive Findings).
Genotype-Phenotype Correlations
The 7q11.23 recurrent deletions of the WBSCR comprise either 1.55 megabases (Mb) (90%-95% of individuals with WS) or 1.84 Mb (5%-10% of individuals with WS) [Bayés et al 2003, Palacios-Verdú et al 2015].
- Hypertension is less prevalent in those individuals with WS who are hemizygous for NCF1, located in one of the blocks of low copy repeats that flank the WBSCR [Del Campo et al 2006].
- A more severe phenotype with lower cognitive ability is observed in individuals with very large deletions (>2-4 Mb) that include the WBSCR than in individuals with a typical 1.5-1.8-Mb WBSCR deletion [Stock et al 2003, Marshall et al 2008].
Shorter deletions within the WBSCR have a variable phenotype depending on the extent of the deletion.
- Individuals with partial WBSCR deletions that include the usual telomeric breakpoint (including GTF2I) have classic WS features, including intellectual disability [Botta et al 1999, Heller et al 2003].
- Those with partial WBSCR deletions that do not include deletion of GTF2I – including some individuals with de novo short deletions and families with "SVAS plus" – do not have intellectual disability but often demonstrate the WS cognitive profile [Morris et al 2003]. In two families, deletion of ELN and an additional gene, LIMK1, was associated with the WS cognitive profile but not with intellectual disability or other characteristics of WS [Frangiskakis et al 1996]. Another family with a similar deletion did not have the WS cognitive profile [Tassabehji et al 1998].
Deletions within the WBSCR may be of maternal or paternal origin [Ewart et al 1993a, Dutly & Schinzel 1996, Urbán et al 1996]. No phenotypic differences have been related to the parent of origin in some series [Wu et al 1998], while microcephaly has been correlated with maternal origin of the WBSCR deletion in others [Del Campo et al 2006].
Penetrance
Penetrance is 100%; expression of the phenotypic features is variable.
Nomenclature
The first descriptions of WS were incomplete in that they reflected the chief complaint of the individual or the medical specialty of the observer. Thus, nephrologists and endocrinologists described "idiopathic infantile hypercalcemia" (IHC), and cardiologists reported "supravalvular aortic stenosis syndrome" (SASS).
Early reports also noted dysmorphic facial features that were thought to resemble elves of legend: for a time, the term “Williams elfin facies syndrome” was used.
After the reports of Williams et al [1961] and Beuren et al [1962], the condition was called Williams syndrome in the US and Williams-Beuren syndrome in Europe.
Prevalence
A study of WS in Norway reported a prevalence of 1:7500 [Strømme et al 2002].
Differential Diagnosis
Williams syndrome (WS) should be distinguished from other syndromes characterized by developmental delay, attention deficit hyperactivity disorder, short stature, distinctive facies, and/or congenital heart disease. These include: Noonan syndrome, deletion 22q11.2 (DiGeorge syndrome), Smith-Magenis syndrome, Kabuki syndrome, and fetal alcohol syndrome.
Individuals with supravalvular aortic stenosis (SVAS) should be evaluated to determine if WS or autosomal dominant SVAS (OMIM 185500) is the appropriate diagnosis.
Table 2.
Disorders to Consider in the Differential Diagnosis of Williams Syndrome
| Disorder | Gene(s) | MOI | Clinical Features of the Disorder | ||
|---|---|---|---|---|---|
| Most Common Congenital Heart Disease | Distinguishing Facial Features | Additional Features | |||
| Williams syndrome | See footnote 1 | AD | Supravalvar aortic stenosis |
|
|
| Noonan syndrome | PTPN11 SOS1 RAF1 RIT1 KRAS NRAS BRAF MAP2K1 | AD | Pulmonary valve stenosis |
|
|
| 22q11.2 deletion syndrome | See footnote 2 | AD | Conotruncal heart defects |
|
|
| Smith-Magenis syndrome | RAI1 3 | See footnote 3 | Septal defects |
|
|
| Kabuki syndrome | KMT2D | AD 4 | Coarctation of the aorta |
|
|
| KDM6A | XL 5 | ||||
| Fetal alcohol syndrome | NA 6 | Septal defects |
|
| |
AD = autosomal dominant; AR = autosomal recessive; MOI = mode of inheritance; NA = not applicable; XL = X-linked
- 1.
Williams syndrome is caused by a contiguous gene deletion of the Williams-Beuren syndrome critical region (WBSCR) that encompasses the elastin gene (ELN).
- 2.
22q11.2 deletion syndrome is caused by deletion of genes within the DiGeorge chromosome region (DGCR). About 93% of probands have a de novo deletion of 22q11.2 and 7% have inherited the 22q11.2 deletion from a parent.
- 3.
Smith-Magenis syndrome is caused by deletion or mutation of RAI1 on chromosome 17p11.2. Virtually all occurrences are de novo.
- 4.
KMT2D-related Kabuki syndrome is inherited in an autosomal dominant manner.
- 5.
To date, only six individuals with Kabuki syndrome caused by pathogenic variants or deletions of KDM6A have been reported; all have had a proven or apparent de novo variant. While X-linked inheritance is theoretically possible, no familial cases of Kabuki syndrome resulting from pathogenic variants in KDM6A have been reported.
- 6.
Fetal alcohol syndrome is caused by prenatal exposure to alcohol.
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with Williams syndrome (WS), and to guide medical management, the following evaluations are recommended [Committee on Genetics 2001, Committee on Genetics 2002]:
- Complete physical and neurologic examination
- Plotting of growth parameters on Williams syndrome growth charts
- Cardiology evaluation
- Full clinical evaluation by a cardiologist with experience in treating WS
- Measurement of blood pressure in all four limbs
- Echocardiogram, including Doppler flow studies
- Electrocardiogram
- Additional cardiovascular imaging studies (computed tomography, magnetic resonance angiography, or cardiac catheterization) may be required in individuals with diminished pulses, bruits, or signs of diffuse thoracic aortic stenosis.
- Urinary system evaluation
- Ultrasound examination of the bladder and kidneys
- Serum concentration of BUN and creatinine
- Urinalysis
- Calcium determinations
- Serum concentration of calcium or ionized calcium
- Calcium/creatinine determination on a spot urine sample (See Sargent et al [1993] for normal values.)
- Thyroid function tests
- Ophthalmologic evaluation
- Baseline audiologic evaluation
- Multidisciplinary developmental evaluation, including assessment of motor, speech, language, personal-social, general cognitive, and vocational skills
- Assessment of behavior including attention, anxiety, and adaptive skills
- Consultation with a clinical geneticist and/or genetic counselor
Treatment of Manifestations
Cognitive/behavioral. Developmental disabilities should be addressed by early intervention programs, special education programs, and vocational training. Recommended therapies include speech/language, physical, and occupational therapy. Consider hippotherapy (use of equine movement during speech, physical, and/or occupational therapy).
- Verbal strengths can be used to assist in learning spatial tasks.
- Phonics methods are recommended to teach reading [John & Mervis 2010].
- Mastery of daily living skills contributes to adult well-being and should be encouraged.
Psychological evaluation, polysomnography, and psychiatric evaluation should guide therapy for the individual.
- Behavior in young children may be addressed using techniques based on applied behavior analysis [Mervis & John 2010].
- Behavioral counseling and psychotropic medication are often used to manage behavior problems, especially attention deficit disorder and anxiety, which require pharmacologic treatment in approximately 50% [Cherniske et al 2004].
- Self-calming techniques can help manage anxiety.
Cardiovascular. Surgical correction of SVAS is performed in 20%-30% [Kececioglu et al 1993, Bruno et al 2003, Collins et al 2010b]. Surgical treatment of mitral valve insufficiency or renal artery stenosis may be required.
Hypertension is usually treated medically. In one series, calcium channel blockers were used successfully [Bouchireb et al 2010]. Antihypertensive therapy also results in improvement in vascular stiffness [Kozel et al 2014]. Lifelong monitoring of the cardiovascular system by a cardiologist familiar with treating WS is recommended.
Hypercalcemia. Management of hypercalcemia involves the following:
- Hydration status should be assessed; increase water intake as indicated.
- The diet should be adjusted with the help of a nutritionist so that the calcium intake is not higher than 100% of the recommended daily intake (RDI) [Ross et al 2011]. If the serum concentration of calcium remains elevated, dietary calcium should be reduced; but the serum concentration of calcium must be monitored. Parents should be counseled not to restrict dietary intake of calcium without medical supervision.
- Vitamin supplements containing vitamin D should be avoided. If vitamin D deficiency is suspected, it is important to check vitamin D levels prior to initiating therapy, and calcium levels must be monitored during treatment. Absorption of calcium from the gut is increased in Williams syndrome (cause unknown) and vitamin D promotes calcium absorption.
- Refractory hypercalcemia may be treated with oral steroids.
- Intravenous pamidronate has been used successfully to treat infants with severe symptomatic hypercalcemia [Cagle et al 2004, Oliveri et al 2004].
- Referral to an endocrinologist and/or nephrologist is recommended for treatment of persistent hypercalcemia, hypercalciuria, and/or nephrocalcinosis.
Eye, ear, nose, and throat. Hyperopia is treated with corrective lenses; strabismus is treated with patching of one eye or surgery; dacrostenosis is treated as in the general population.
Recurrent otitis media may be treated with tympanotomy tubes.
Hypersensitivity to sounds may be treated with ear protection when increased noise levels can be predicted.
Dental care may require assistance with daily brushing and flossing. Dental cleaning frequency should be increased to every four months in adolescents and adults. Orthodontic referral should be considered for treatment of malocclusion.
Gastrointestinal.The treatment of feeding problems in infancy and abdominal pain in children and adults depends on the cause (e.g., G-E reflux, hypercalcemia, hiatal hernia, and/or diverticulitis). Infants often benefit from feeding therapy.
Constipation must be aggressively managed at all ages due to the increased risk for early onset diverticulosis/diverticulitis. Treatment usually includes dietary increase in water and fiber followed by osmotic laxative treatment. Severe abdominal pain may indicate diverticulitis and/or intestinal perforation, which may occur at a young age in WS.
Urinary tract abnormalities. Individuals with febrile urinary tract infections will likely require investigation of the lower urinary tract such as voiding cystourethrogram to direct treatment.
Endocrine. Early puberty may be treated with a gonadotropin-releasing hormone agonist [Partsch et al 2002, Pober 2010]. Hypothyroidism is treated with oral thyroxine therapy; subclinical hypothyroidism typically is monitored but does not require treatment.
Prevention of Secondary Complications
The following are indicated:
- Exercise and a balanced diet to avoid insulin resistance/diabetes mellitus
- Range of motion exercises to prevent or ameliorate joint contractures
- Because of the increased risk for myocardial insufficiency in individuals with biventricular outflow tract obstruction, especially during induction of anesthesia [Horowitz et al 2002] and because there is an increased risk for adverse events with sedation or anesthesia in WS, anesthesia consultation for surgical procedures. Guidelines for sedation and anesthesia risk assessment and anesthetic management for WS have been published [Burch et al 2008, Matisoff et al 2015, Latham et al 2016]. Electrocardiogram prior to surgery.
- Awareness of the risk for myocardial insufficiency and cardiac arrest; for surgical procedures, use of a center equipped for cardiopulmonary resuscitation
Surveillance
Table 3.
Surveillance for Williams Syndrome
| Interval / Age | Test/Measurement |
|---|---|
| In infants – toddlers |
|
| Annual / all ages 1 |
|
| Every 2 years |
|
| Every 10 years |
|
| In adults |
|
- 1.
Except as noted
- 2.
If normal, OGTT should be repeated every five years.
Agents/Circumstances to Avoid
Children with WS should not be given multivitamins because all pediatric multivitamin preparations contain vitamin D.
Evaluation of Relatives at Risk
See Genetic Counseling for issues related to testing of at-risk relatives for genetic counseling purposes.
Pregnancy Management
Pregnancies in women with WS are high risk. They should be monitored for the development of pregnancy-induced hypertension, arrhythmias, and heart failure. Regular urinalyses should be performed in late gestation due to the increased risk for urinary tract infection. Ultrasound monitoring of the fetus is suggested [Lin et al 2008].
Therapies Under Investigation
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for access to information on clinical studies for a wide range of diseases and conditions. Note: There may not be clinical trials for this disorder.