Pyomyositis
Pyomyositis (PM) is a rare primary bacterial infection of the skeletal muscle, usually resulting from hematogenous spread or due to muscle injury, and characterized by pain and tenderness in the affected muscle, fever and abscess formation.
Epidemiology
Prevalence is unknown. PM is commonly found in the tropics and is endemic to Eastern Uganda where 400-900 cases are reported annually. Cases in temperate regions such as the U.S. are now increasing in frequency.
Clinical description
PM occurs in all ages with a male predominance. In tropical regions, it usually presents in otherwise healthy, athletic individuals and affects mainly children (aged 2-5) and young adults, while in temperate regions most patients are immunocompromised (due to malnutrition, chemotherapy, diabetes mellitus, HIV infection) or suffer from chronic renal failure or rheumatoid arthritis. Muscles most commonly involved include the serratus anterior, pectoralis major, biceps, the abdominal and spinal muscles, glutei, iliopsoas, quadriceps and gastrocnemius. There are 3 phases seen in disease development. The invasive stage lasts 1-10 days with manifestations of localized muscle ache/pain and swelling (with a lack of warmth or erythema), along with a low grade fever. Symptoms of appendicitis can be reported in those with iliopsoas pyomyositis. The purulent or suppurative stage follows 2-3 weeks after symptom onset with a progressive febrile illness and a soft tissue mass that is tender and painful when touched. If left untreated, the third stage involves sepsis that can lead to bacteremia, septicemia, metastatic abscess, acute renal failure, septic shock and death.
Etiology
The exact etiology is unknown but muscle trauma or vigorous exercise may facilitate hematogenous access of bacteria to the skeletal muscles (usually resistant to these types of infections). Fibronectin binding receptors on muscle cells have been proposed as a possible entry point for bacteria. In most cases the causative organism is Staphylococcus aureus (SA) (up to 90% of tropical cases, 70% of temperate cases) but infections with various other species (ex. Streptococci) have been reported. Methicillin-resistant SA (MRSA) is increasing in frequency as the infectious agent seen in non-tropical PM.
Diagnostic methods
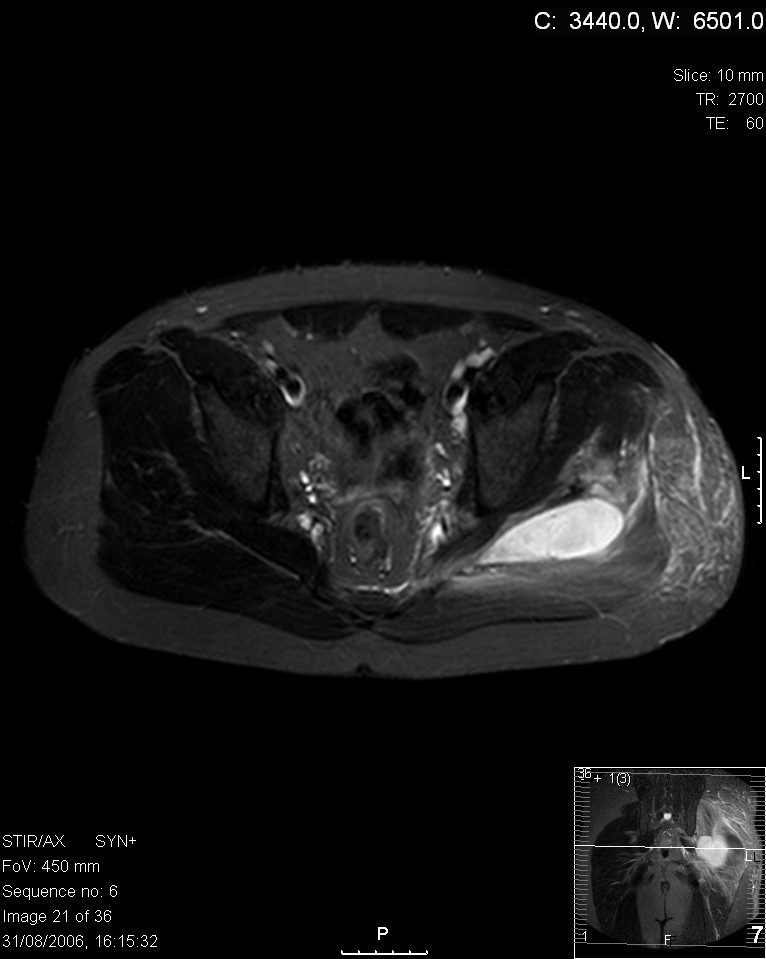
PM is often hard to diagnose. Aspiration of pus from the muscle is usually possible at the purulent stage and can determine a diagnosis. If an abscess is absent, a culture and a muscle biopsy with special staining can equally identify the bacteria responsible and eliminate other possibilities. Diagnostic imaging is useful for diagnosing and treating PM.
Differential diagnosis
Differential diagnoses include parasitic and viral myositis, leptospirosis, polymyositis, trichinellosis (see these terms), osteomyelitis, cellulitis, necrotizing fasciitis, clostridial myonecrosis, septic arthritis, deep vein thrombosis and muscle contusions, hematomas, ruptures or strains.
Management and treatment
Early diagnosis and prompt treatment with antibiotics is essential. Due to the increased occurrence of MRSA, vancomycin, teicoplanin, tigecycline, daptomycin, linezolid, or daptomycin are the antibiotics of choice. Treatment with tetracycline or trimethoprim-sulfamethoxisole may be sufficient in some cases. Antibiotics are taken for 3-4 weeks, or longer, in cases of multiple muscle involvement, poorly drained infections, when initiation of treatment is delayed or when due to mycobacteria or Bartonella. If an abscess forms, treatment involves incision, debridement and muscle drainage or in some cases guided aspiration followed by antibiotic therapy. Muscle drainage is required in 40-70% of cases and repeated drainage in 10% of cases. Treatment should continue until a patient is fever-free for 7-10 days, wound is clean and leukocyte count is back to normal.
Prognosis
The prognosis is good when diagnosed and treated properly and there is very little residual deformity of the muscles, if any. When PM is left untreated, the mortality rate is 0.5 - 2%.