Gestational Trophoblastic Neoplasm
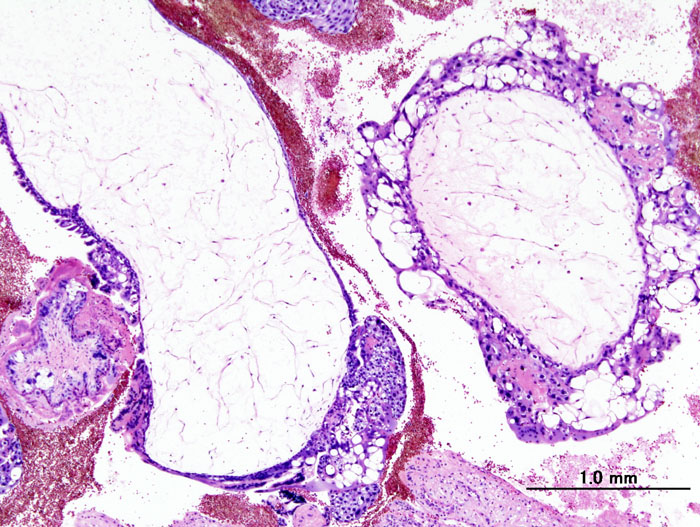
Gestational trophoblastic tumors (GTT) are malignant forms of gestational trophoblastic disease. The tumor always follows pregnancy, most often molar pregnancy (hydatidiform mole; see this term). Four histological subtypes have been described: invasive mole, gestational choriocarcinoma, placental site trophoblastic tumor and epithelioid trophoblastic tumor (see these terms).
Epidemiology
Exact annual incidence is not known but it is estimated to be about 1/1,000,000 women.
Clinical description
GTTs occur following hydatidiform moles (see this term) (15% of complete moles and about 3% of partial moles), following spontaneous miscarriage (1/150) or childbirth (1/40,000). Indicative signs are an absence of normalization or a secondary elevation of total serum chorionic gonadotropin (hCG) levels after evacuation of a hydatidiform mole (more than 60% of cases), persistent unexplained metrorrhagia following spontaneous miscarriage or voluntary termination of pregnancy (VTP) (about 30% of cases) and very occasionally, unexplained metrorrhagia in the weeks or months following normal childbirth or ectopic pregnancy (about 10% of cases). Exceptionally, metastasis may be a sign of the disease in women of childbearing age.
Etiology
The etiology of gestational trophoblastic tumors is not known. Identification of a GTT is based on a total serum hCG assay, which is recommended following hydatidiform moles in patients with metrorrhagia persisting for more than six weeks after pregnancy, and in any patient of childbearing age who has metastasis (lung, liver, brain, kidney, vagina) with no known primary tumor.
Diagnostic methods
Diagnosis of a post-molar GTT relies on one of the following four criteria: stable hCG levels (variation of less than 10%) with at least four weekly assays over a period of at least three weeks (days 1, 7, 14, 21), increase of at least 10% in hCG with at least three weekly assays over at least two weeks (days 1, 7, 14), persistence of detectable hCG values for more than six months following mole evacuation or based on histological diagnosis of a choriocarcinoma.
Differential diagnosis
GTTs must not be confused with hydatidiform moles (see this term) and, for choriocarcinomas, with non-gestational choriocarcinomas, which are most often ovarian.
Management and treatment
As soon as the diagnosis is made, staging must be performed to identify frequent metastases. Staging involves endovaginal pelvic color doppler ultrasound, pelvic and cerebral MRI, and abdominal/chest CT. A lung X-ray must be performed to calculate the FIGO 2000 score (International Federation of Obstetrics and Gynecology) in case of lung metastasis on CT. This score makes it possible to distinguish between low-risk GTTs (score of 6 or lower) and high-risk GTTs (score of 7 or higher). Management should be multidisciplinary and must be discussed by a panel of physicians in a specialized center. Low-risk tumors are treated by systemic single-agent chemotherapy, e.g. methotrexate (marketing authorization). High-risk tumors are treated first line with systemic multi-agent chemotherapy. Hysterectomy can of course not be considered for first-line treatment in women who wish to become pregnant, unless there is no option. Placental site trophoblastic tumors and epithelioid trophoblastic tumors are special cases: the FIGO score is not appropriate and total hysterectomy is the standard treatment as these tumors are usually chemo-resistant.
Prognosis
The overall recovery rate is around 99%. The prognosis is very closely related to the rapidity of diagnosis, the risk level of the tumor (low or high) and the suitability of treatment.