Hypothyroidism, Congenital, Nongoitrous, 2
A number sign (#) is used with this entry because of evidence that congenital nongoitrous hypothyroidism-2 (CHNG2) is caused by heterozygous mutation in the PAX8 gene (167415) on chromosome 2q14.
For a general phenotypic description and a discussion of genetic heterogeneity of congenital nongoitrous hypothyroidism, see 275200.
DescriptionIn 80 to 85% of cases, congenital hypothyroidism is associated with, and presumably is a consequence of, thyroid dysgenesis. In these cases, the thyroid gland can be absent (agenesis), ectopically located, and/or severely reduced in size (hypoplasia). When thyroid hormone therapy is not initiated within the first 2 months of life, congenital hypothyroidism can cause severe neurologic, mental, and motor damage (Macchia et al., 1998).
Clinical FeaturesThyroid dysgenesis is the most frequent cause of congenital hypothyroidism, accounting for 85% of cases (Fisher, 1983). Ectopic thyroid gland is the most frequent malformation, with thyroid tissue being found most often at the base of the tongue. Athyreosis is defined as the absence of any detectable thyroid tissue.
Athyreotic cretinism is not as clearly mendelizing as is goitrous cretinism. There is some familial aggregation which may be of the same type as is seen with many common congenital malformations. It is noteworthy that whether goiter is present or not is dependent on age and treatment. Under certain circumstances a patient who has the same defect as in one of the types of goitrous cretinism may appear to be athyreotic (Beierwaltes, 1964).
In an inbred Amish group, Cross et al. (1968) observed 2 sisters with cretinism and the Kocher-Debre-Semelaigne syndrome (myotonia and muscular pseudohypertrophy). Although no thyroid was palpable, sensitive scanning techniques showed the presence of a small amount of thyroid tissue in the neck. Thus, 'agoitrous cretinism' is a better designation than athyreotic cretinism.
Kaplan et al. (1977) described 2 nonconsanguineous Ashkenazi Jewish families in each of which a brother and sister had hypothyroidism associated with ectopia and hypoplasia of the thyroid. They cited another report of familial occurrence of ectopic thyroid (Mahoney and Igo, 1974). Hypothyroidism may not become evident until late childhood or adolescence. Cases reported by Gabr (1962) and Little et al. (1965) had severe cretinism. Thyroid-stimulating hormone was elevated. Rosenberg and Gilboa (1980) described 2 sisters with sublingual thyroid glands and hypothyroidism. A brother had agenesis of the left lobe of the thyroid but normal thyroid function. Donegan and Wood (1985) reported intratracheal thyroid in 2 sisters. In 1, the ectopic thyroid was involved in follicular carcinoma.
A possible relationship to inability to taste PTC (171200) was proposed by Shepard and Gartler (1960), Fraser (1961), Shepard and Andersen (1965). Both newborn athyreotic hypothyroidism and inability to taste PTC have a lower frequency in blacks than in whites. Nearly all patients with athyreotic hypothyroidism are PTC nontasters.
Scriver (2002) reported that he and his colleagues, in an unpublished study, found no disproportionate association of PTC taste type with the nonmendelian form of congenital hypothyroidism.
De Zegher et al. (1988) noted an association between growth hormone deficiency and congenital hypothyroidism. They pointed out the necessity for careful monitoring of growth in children treated for congenital hypothyroidism.
Eberle (1993) reported the case of a boy, almost 12 years old, with short stature, dysplastic epiphyses, and vertebral anomalies thought to be due to spondyloepiphyseal dysplasia. Because of facial appearance, Aarskog syndrome (305400) had been suggested. The importance of recognizing the true nature of this patient's disorder as congenital hypothyroidism is obvious.
PathogenesisBlizzard et al. (1960) suggested that maternal autoantibodies may be responsible for destruction of the fetal thyroid. They observed the birth of 2 successive cretins from a mother with autoantibodies. Antibodies were implicated in the familial cases of Sutherland et al. (1960). This could be a nongenetic mechanism of familial occurrence of athyreotic cretinism.
InheritanceAlthough these cases, like those of panhypopituitarism, are usually sporadic, out of 152 cases reported by Wilkins (1965), 1 sib pair was found. Ainger and Kelley (1955) reported 3 sibs, as did Sutherland et al. (1960). Females are affected about twice as often as males. Greig et al. (1966) described 2 pairs of monozygotic twins, all of whom were affected. One pair was considered athyreotic and the other had residual thyroid and ectopic tissue, respectively. The authors, who referred to the condition as thyroid dysgenesis, also described affected mother and child; the father was unknown and presumably incest was possible, making recessive inheritance likely. Since thyroid-stimulating hormone (188540) and the effects of thyrotropin-releasing hormone (613879) were not tested in the cases of Cross et al. (1968), these and others of the reported cases of 'athyreotic cretinism,' may be instances of 'pituitary cretinism,' i.e., thyrotropin deficiency (275100).
Castanet et al. (2000) reported that 2% of congenital hypothyroidism patients with thyroid dysgenesis have a positive familial history. Castanet et al. (2001) described the clinical characteristics of these familial cases and compared them with sporadic cases. Using the French national population-based registry of the first 19-year screening program, they identified 67 patients with a positive family history of congenital hypothyroidism with thyroid dysgenesis (at least 2 affected family members) belonging to 32 multiplex families. Families were identified with ectopic gland (12), athyreosis (7), or both (13). Comparison of familial with isolated cases showed a similar etiologic diagnosis distribution of congenital hypothyroidism (40% vs 33% for athyreosis and 60% vs 67% for ectopic thyroid gland, respectively), whereas a significantly lower predominance of females was found in familial than in isolated cases. Extrathyroidal congenital malformations were found with a similarly higher incidence in familial and isolated congenital hypothyroidism populations compared with the general population (respectively, 9% and 8.2% vs 2.5%). The authors concluded that, although familial cases represent a minority of cases of congenital hypothyroidism caused by thyroid dysgenesis, they were observed in a significantly higher proportion (greater than 15-fold) than would be expected from chance alone. This familial clustering, including athyreosis and ectopic thyroid gland, strongly suggests that genetic factors could be involved in thyroid dysgenesis with a common underlying mechanism for both etiologic groups. Moreover, the high proportion of extrathyroidal congenital malformations in a population affected by congenital hypothyroidism due to thyroid dysgenesis suggests that the potential genetic factors involved in thyroid gland organogenesis are also involved in the development of other organs.
Leger et al. (2002) investigated thyroid developmental abnormalities in first-degree relatives of congenital hypothyroidism children with thyroid dysgenesis, an anomaly which, when present, is sometimes asymptomatic. Thyroid ultrasonography and function were evaluated among 241 first-degree relatives of 84 isolated congenital hypothyroidism children with thyroid dysgenesis. The results were compared with those of an unselected control population of 217. In 19 individuals (7.9% of cases) belonging to 18 families (21.4%), 21 cases of thyroid developmental abnormalities were detected, whereas only 2 subjects (0.9%) were affected in controls (P less than 0.001). These 21 thyroid developmental abnormalities included 14 cases of thyroglossal duct cysts (188455), 3 cases of additional thyroid tissue with presence of a pyramidal lobe, 3 cases of thyroid hemiagenesis, and 1 case of ectopic thyroid tissue. All of these subjects showed normal thyroid function and belonged to nuclear families of congenital hypothyroidism children with athyreosis (8), ectopic thyroid tissue (9), or hemiagenesis (1). A segregation analysis led to the conclusion that thyroid developmental abnormalities are compatible with an autosomal dominant mode of inheritance with a low penetrance estimated at 21% for asymptomatic thyroid developmental abnormalities and a probability of less than 7% of developing congenital hypothyroidism for a carrier of the susceptibility allele. The authors concluded that these observations support the hypothesis of a common genetic component of the disorder with heterogeneous phenotypes.
Perry et al. (2002) noted that since the advent of biochemical screening for congenital hypothyroidism, most reported instances of monozygotic twins with thyroid dysgenesis had been discordant, and most were missed on neonatal screening, presumably due to fetal blood mixing. Perry et al. (2002) hypothesized that there may be a bias leading to preferential reporting of discordant twins and/or of false-negative screening results. In a systematic search for twins in 2 congenital hypothyroidism screening centers, Quebec and Brussels, that used a primary TSH approach, they identified a total of 16 pairs of twins, all discordant for congenital hypothyroidism. These included 5 monozygotic pairs with thyroid dysgenesis. The median increase in TSH between screening and diagnosis was 7-fold in monozygotic twins versus 2-fold in matched singletons, suggesting fetal blood mixing between the twins. Thus, discordance for thyroid dysgenesis appears to be the rule in monozygotic twins, and fetal blood mixing may result in delayed or missed diagnoses. Perry et al. (2002) concluded that a second sample for congenital hypothyroidism screening at 14 days of age should be considered for all same sex twins and that thyroid dysgenesis generally results from epigenetic phenomena, early somatic mutations, or postzygotic stochastic events.
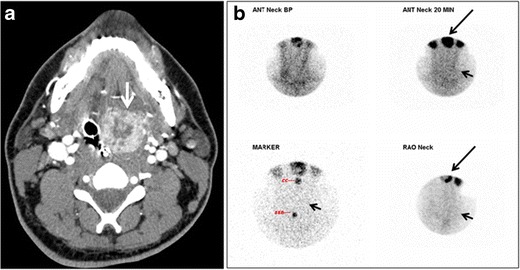
Molecular GeneticsIn 3 infants with congenital hypothyroidism and thyroid hypoplasia, Macchia et al. (1998) identified heterozygosity for 3 different mutations in the PAX8 gene (167415.0002-167415.0004). The first infant had thyroid ectopy and reduced gland size with elevated levels of TSH and thyroglobulin but thyroxin (T4) levels in the normal range. The second infant was diagnosed with thyroid hypoplasia and had TSH levels 100-fold above normal and T4 levels well below normal. The third infant had severe thyroid hypoplasia (cystic thyroid rudiment) and an elevated TSH with below-normal thyroid hormone levels. His mother and sister were heterozygous for the same mutation but displayed clinical variability: the mother had been diagnosed with hypothyroidism at age 10 and had a hypoplastic thyroid gland, whereas the sister had a thyroid of a size at the lower limit of normal, with normal thyroid hormone levels but high TSH values.
In a mother and daughter with congenital hypothyroidism and aplasia and eutopic hypoplasia of the thyroid gland, respectively, Vilain et al. (2001) identified heterozygosity for a mutation in the PAX8 gene (167415.0005). An unaffected daughter in the family did not carry the mutation.
In a girl with overt congenital hypothyroidism and a hypoplastic thyroid gland, Congdon et al. (2001) identified heterozygosity for a mutation in the PAX8 gene (167415.0007). Her mother, who was also heterozygous for the mutation, had a thyroid gland of normal size and displayed no signs or symptoms of hypothyroidism until age 31, at which time she was diagnosed with mild autoimmune hypothyroidism with positive antibodies. The unaffected father and brother did not have the mutation. Congdon et al. (2001) suggested that PAX8 mutations may have incomplete penetrance or variable expressivity, and noted that phenotypic variability was also reported in the family studied by Macchia et al. (1998).
In 2 children who were found to have congenital hypothyroidism on neonatal screening and their father, Meeus et al. (2004) identified heterozygosity for a mutation in the PAX8 gene (167415.0006). Although neonatal scintigraphy revealed an in situ thyroid gland of normal shape and size in the brother and sister, both were later found to have hypoplastic glands, at age 11.5 and 3.5 years, respectively. The father had been diagnosed with hypothyroidism at age 3; at age 25 his thyroid gland was nonpalpaple and echography showed a 'small amount of thyroid tissue (thickness less than 0.5 cm) in normal position', suggestive of thyroid hypoplasia. The father was also found to have agenesis of the right kidney, and Meeus et al. (2004) noted that PAX8 is also strongly expressed in the kidney during development.
Grasberger et al. (2005) studied 7 members of a nonconsanguineous family who were hypothyroid with an apparent autosomal dominant mode of inheritance but who had striking variability in their initial clinical presentation. The proband and her brother were found to have an elevated TSH and low free T4 on neonatal screening; both had a thyroid gland of normal shape and position on scintigraphy. Their affected mother had been diagnosed with mild hypothyroidism after routine blood testing at age 37. A female cousin was also discovered to have a very elevated TSH and very low free T4 on neonatal screening; she had no thyroidal or ectopic uptake of radioiodine on scintigraphy, consistent with athyreosis. Her 5-year-old brother was subsequently screened and found to have an elevated TSH with normal free T4; their father had been diagnosed with hypothyroidism at age 5. The 67-year-old grandmother of the cousins was screened as a part of this study and diagnosed with 'moderate thyroid failure.' Linkage analysis showed haplotype sharing of the affected family members at the PAX8 locus; sequence analysis revealed heterozygosity for a mutation in the PAX8 gene (167415.0008) in affected family members.
De Felice and Di Lauro (2004) reviewed the development of the thyroid gland and the genetic molecular mechanisms leading to thyroid dysgenesis.
Park and Chatterjee (2005) reviewed the genetics of primary congenital hypothyroidism, summarizing the different phenotypes associated with known genetic defects and proposing an algorithm for investigating the genetic basis of the disorder.
Exclusion Studies
Lapi et al. (1997) screened 61 patients with congenital hypothyroidism for mutations in the TTF1 gene using SSCP and did not identify any mutations. Using direct sequencing, they rescreened 22 patients from that group who had thyroid agenesis but again detected no mutations in TTF1. Lapi et al. (1997) concluded that mutations in the TTF1 gene are not a frequent cause of congenital hypothyroidism.
Investigating the PAX8, TTF1 (600635), FOXE1, and TSHR (603372) genes, all of which were implicated in thyroid development, Castanet et al. (2005) performed linkage analysis followed by mutation analysis in 19 multiplex TD families. The lod score results failed to prove linkage between any of the 4 genes and the TD phenotype, whatever the postulated mode of inheritance. Extended haplotypes confirmed by mutation analysis showed that the 4 genes were excluded in 5 of the 19 families, demonstrating the relevance of other genes in TD.
Population GeneticsThe incidence of newborn athyreotic hypothyroidism in whites and blacks is strikingly different: 1 in 5,526 and 1 in 32,377, respectively (Brown et al., 1981). The relative rarity in blacks has long been recognized (Childs and Gardner, 1954).
A female predominance has been identified (Goujard et al., 1981).
Nomenclature'Athyreotic cretinism' is an unsatisfactory term which shares the negative connotations of 'congenital deafmutism.' Both designations refer to the untreated state; hence the alternative terms listed in the title, any one of which is preferable to athyreotic cretinism.