Asbestosis
Overview
Asbestosis (as-bes-TOE-sis) is a chronic lung disease caused by inhaling asbestos fibers. Prolonged exposure to these fibers can cause lung tissue scarring and shortness of breath. Asbestosis symptoms can range from mild to severe, and usually don't appear until many years after initial exposure.

Bronchioles and alveoli in the lungs
In your lungs, the main airways, called bronchi, branch off into smaller and smaller passageways. The smallest airways, called bronchioles, lead to tiny air sacs called alveoli.
Asbestos is a natural mineral product that's resistant to heat and corrosion. It was used extensively in the past in products such as insulation, cement and some floor tiles.
Most people with asbestosis acquired it on the job before the federal government began regulating the use of asbestos and asbestos products in the 1970s. Today, its handling is strictly regulated. Getting asbestosis is extremely unlikely if you follow your employer's safety procedures. Only trained and accredited asbestos professionals should manage asbestos products. Treatment focuses on relieving your symptoms.
Symptoms
The effects of long-term exposure to asbestos typically don't show up until 10-40 years after initial exposure. Symptoms can vary in severity.

Clubbing of fingers
Clubbing of the fingers, in which the fingertips spread out and become rounder than usual, is often linked to heart or lung conditions.
Asbestosis signs and symptoms may include:
- Shortness of breath
- A persistent, dry cough
- Chest tightness or pain
- Dry and crackling sounds in your lungs when you inhale
- Fingertips and toes that appear wider and rounder than usual (clubbing)
When to see a doctor
If you have a history of exposure to asbestos and you're experiencing increasing shortness of breath, talk to your health care provider about the possibility of asbestosis.
Causes
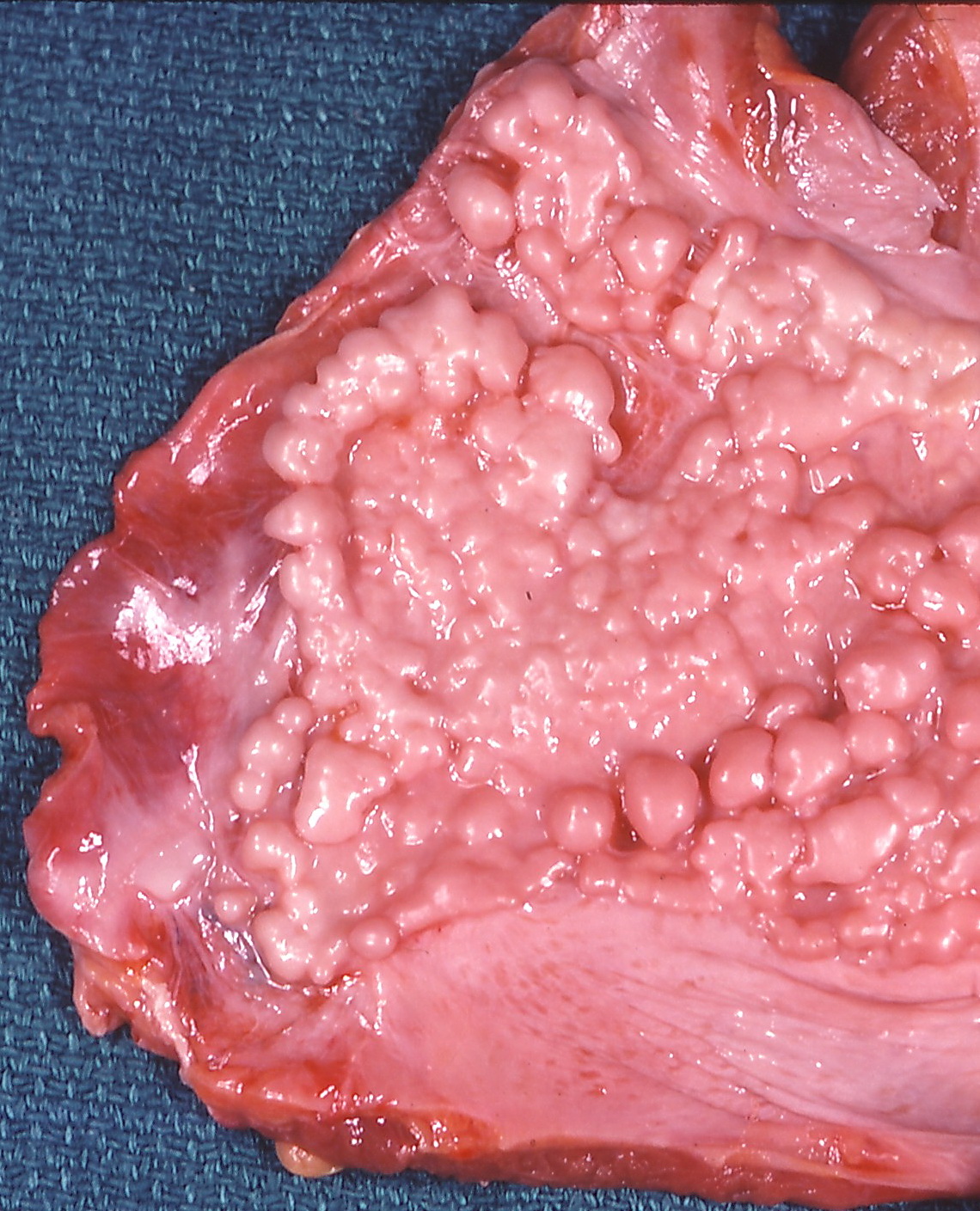
If you are exposed to high levels of asbestos dust over a long period of time, some of the airborne fibers can become lodged within your alveoli — the tiny sacs inside your lungs where oxygen is exchanged for carbon dioxide in your blood. The asbestos fibers irritate and scar lung tissue, causing the lungs to become stiff. This makes it difficult to breathe.
As asbestosis progresses, more and more lung tissue becomes scarred. Eventually, your lung tissue becomes so stiff that it can't contract and expand normally.
Smoking appears to increase the retention of asbestos fibers in the lungs, and often results in a faster progression of the disease.
Risk factors
People who worked in mining, milling, manufacturing, and installation or removal of asbestos products before the late 1970s are at highest risk of asbestosis. Examples include:
- Asbestos miners
- Aircraft and auto mechanics
- Boiler operators
- Building construction workers
- Electricians
- Railroad workers
- Refinery and mill workers
- Shipyard workers
- Workers removing asbestos insulation around steam pipes in older buildings
Risk of asbestosis is generally related to the amount and the duration of exposure to asbestos. The greater the exposure is, the greater the risk is of lung damage.
Secondhand exposure is possible for household members of exposed workers, as asbestos fibers may be carried home on clothing. People living close to mines may also be exposed to asbestos fibers released into the air.
Complications
If you have asbestosis, you're at increased risk of developing lung cancer — especially if you smoke or have a history of smoking. Rarely, malignant mesothelioma, a cancer of the tissue around the lung, can occur many years after exposure to asbestos.
Prevention
Reducing exposure to asbestos is the best prevention against asbestosis. In the United States, federal law requires employers in industries that work with asbestos products — such as construction — to take special safety measures.
Many homes, schools and other buildings built before the 1970s have materials such as pipes and floor tiles that contain asbestos. Generally, there's no risk of exposure as long as the asbestos is enclosed and undisturbed. It's when materials containing asbestos are damaged that there's a danger of asbestos fibers being released into the air and inhaled. Always have asbestos products inspected and repaired or removed by trained and accredited asbestos professionals.
Diagnosis
Asbestosis can be difficult to diagnose because its signs and symptoms are similar to those of many other types of respiratory diseases.
Physical exam
As part of your evaluation, your health care provider discusses your health history, occupation and exposure risk to asbestos. During a physical exam, your health care provider uses a stethoscope to listen carefully to your lungs to determine if they make a crackling sound while inhaling.
A variety of diagnostic tests might be needed to help pinpoint the diagnosis.
Imaging tests
These tests show images of your lungs:
- Chest X-ray. Advanced asbestosis appears as excessive whiteness in your lung tissue. If the asbestosis is severe, the tissue in both lungs might be affected, giving them a honeycomb appearance.
- Computerized tomography (CT) scan. computed tomography (CT) scans combine a series of X-ray views taken from many different angles to produce cross-sectional images of the bones and soft tissues inside your body. These scans generally provide greater detail and might help detect asbestosis in its early stages, even before it shows up on a chest X-ray.
Pulmonary function tests
Pulmonary function tests determine how well your lungs are functioning. These tests measure how much air your lungs can hold and the airflow in and out of your lungs.

Spirometer
A spirometer is a diagnostic device that measures the amount of air you're able to breathe in and out. It also tracks the time it takes you to exhale completely after you take a deep breath.
During the test, you might be asked to blow as hard as you can into an air-measurement device called a spirometer. More-complete pulmonary function tests can measure the amount of oxygen being transferred to your bloodstream.
Diagnostic procedures
In some situations, your health care provider might remove fluid and tissue for testing to identify asbestos fibers or abnormal cells. Tests may include:
- Bronchoscopy. A thin tube (bronchoscope) is passed through your nose or mouth, down your throat and into your lungs. A light and a small camera on the bronchoscope allow the doctor to look inside your lungs' airways for any abnormalities or to get a fluid or tissue sample (biopsy) if needed.
- Thoracentesis. In this procedure, your doctor injects a local anesthetic and then inserts a needle through your chest wall between your ribs and lungs to remove excess fluid for lab analysis and to help you breathe better. Your doctor might insert the needle with the help of ultrasound guidance.
Treatment
There's no treatment to reverse the effects of asbestos on the alveoli. Treatment focuses on slowing the progression of the disease, relieving symptoms and preventing complications.
You'll need routine follow-up care, such as chest X-rays or CT scans and lung function tests, at regular intervals depending on the severity of your condition. Prompt treatment of respiratory infections can help prevent complications.
Therapy
To ease breathing difficulty caused by advanced asbestosis, your health care provider might prescribe supplemental oxygen. This is delivered by thin plastic tubing with prongs that fit into your nostrils or thin tubing connected to a mask worn over your nose and mouth.
Participating in a pulmonary rehabilitation program may help some people. The program offers educational and exercise components such as breathing and relaxation techniques, ways to improve physical activity habits, and education to improve overall health.
Surgery
If your symptoms are severe, you might be a candidate for a lung transplant.
Self care
In addition to medical treatment:
- Don't smoke. Asbestosis increases the risk of lung cancer. Quitting smoking can reduce this risk. Try to avoid secondhand smoke. Smoking may also cause more damage to your lungs and airways, which further reduces your lung reserves.
- Get vaccinated. Talk to your health care provider about the flu and pneumonia vaccines and the COVID-19 vaccine, which can help lower your risk of lung infections.
- Avoid further asbestos exposure. Further exposure to asbestos can worsen your condition.
Preparing for your appointment
You're likely to start by seeing your family health care provider for the disorder's most common symptom — shortness of breath. He or she might refer you to a specialist in lung problems (pulmonologist).
You might want to have a friend or family member accompany you to your appointment. Often, two sets of ears are better than one when you're learning about a complicated medical problem, such as asbestosis. Take notes if this helps.
What you can do
Before your appointment, you might want to prepare answers to the following questions:
- What are your symptoms and when did they start?
- Have your symptoms stayed the same or gotten worse?
- What kind of work have you done in your career? Be specific.
- Have you been involved in any home-remodeling projects or other building renovations occurring over a long period of time?
- Do you or did you smoke? If so, how much and for how long?
- What medications, vitamins, herbs and other supplements do you take, and the dosages?
If you've had chest X-rays or other imaging tests in the past, let your health care provider know so your provider can request copies to compare to your current imaging tests.
What to expect from your doctor
Your health care provider may ask some of the following questions:
- Are you aware of any exposure to asbestos?
- Do you get short of breath easily?
- How long have you had a cough?
- Have you noticed any wheezing when you breathe?
- Do you or have you ever smoked? If so, would you like help in quitting smoking?
Your health care provider will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your appointment time.