Yellow Nail Syndrome
Description
Yellow nail syndrome (YNS) is classically considered to comprise a clinical triad of yellow nails, lymphedema, and respiratory tract involvement. Two of these symptoms are required for the diagnosis, since the complete triad is only observed in about one-third of patients. Onset is usually after puberty (Hoque et al., 2007).
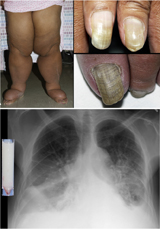
Clinical FeaturesSamman and White (1964) delineated the yellow nail syndrome, reporting 13 cases. The nails are typically slow growing and excessively curved, with a yellowish discoloration, and frequently show ridging due to interrupted growth. Onycholysis can occur in one or more nails. There is associated leg edema.
Wells (1966) described a family with 8 cases in 4 sibships of 2 generations. In the proband, who had yellow nails, lymphedema began in the legs at the age of 51. At times edema also affected the genitalia, hands, face, and vocal cords. Lymphangiograms were interpreted as showing primary hypoplasia of lymphatics. Zerfas and Wallace (1966) described a sporadic case with onset of lymphedema at age 10. Recurrent pleural effusion occurred in some cases.
Govaert et al. (1992) reported a girl who was born at 33 weeks' gestation with nonimmune hydrops and a recurrent left chylothorax to a mother with the yellow nail syndrome. The nonimmune hydrops in this case was diagnosed on a 29-week ultrasound examination. Slee et al. (2000) reported a case of a newborn infant who, at 23 weeks' gestation, was found to have hydrops on antenatal ultrasonography; bilateral chylothorax was found at delivery. The mother had the yellow nail syndrome, with typical nail changes, and bronchiectasis. The infant had a recurrent cough, possibly preceding early onset of bronchiectasis.
Although lymphedema is the most consistent association with yellow nails, other associations include bronchiectasis, sinusitis, chronic cough, and pleural effusions. Nail changes include slow growth, yellow-green discoloration, transverse and longitudinal overcurvature, onycholysis, shedding, cross-ridging, and loss of lunulae and cuticles (Hoque et al., 2007).
In a retrospective study of 11 patients with a diagnosis of YNS, Hoque et al. (2007) found only 1 with a relevant family history that included bronchiectasis and sinusitis, but not yellow nails. Age at onset in the majority of the patients was after 50 years. Four of the 11 patients had complete recovery of their nails over a mean period of 4 to 5 years. A literature review revealed that most of the reported cases have been sporadic. Hoque et al. (2007) concluded that yellow nail syndrome is a sporadic acquired condition rather than a dominantly inherited condition, as currently classified.
Molecular GeneticsFinegold et al. (2001) identified a mutation in the FOXC2 gene (602402.0007) in affected members of a family with lymphedema-distichiasis syndrome (153400). None of these patients were reported as having yellow nails. However, the same mutation was found in 7 affected members of another family with lymphedema-distichiasis syndrome, 3 of whom also had yellow nails. Finegold et al. (2001) concluded that there is phenotypic overlap between lymphedema-distichiasis syndrome and lymphedema-yellow nail syndrome. The authors stated that the phenotypic classification of autosomal dominant lymphedema does not appear to reflect the underlying genetic causation of these disorders, as they may be allelic.
Rezaie et al. (2008) suggested that lymphedema with yellow nails is not a distinct disorder but rather in the spectrum of lymphedema-distichiasis syndrome. They noted that 6 of the 7 patients in the family of Finegold et al. (2001) reported as having yellow-nail syndrome also had distichiasis, which is characteristic of the lymphedema-distichiasis syndrome. In addition, Rezaie et al. (2008) noted that Finegold et al. (2001) found no FOXC2 mutations in 4 additional families with lymphedema and yellow nails. Rezaie et al. (2008) stated that yellow discoloration of the nails is not uncommon with lymphedema, but does not necessarily indicate a diagnosis of so-called 'yellow nail syndrome,' in which the nail changes are very specific. In yellow nail syndrome, the nail plate is yellow and overcurved, but remains translucent and smooth. By contrast, yellow nails in lymphedema syndromes become thickened, rough, and opaque. Associated features such as chronic sinusitis, bronchiectasis or pleural effusion are often essential for a diagnosis of yellow nail syndrome.