Niemann-Pick Disease Type C
Summary
Clinical characteristics.
Niemann-Pick disease type C (NPC) is a slowly progressive lysosomal disorder whose principal manifestations are age dependent. The manifestations in the perinatal period and infancy are predominantly visceral, with hepatosplenomegaly, jaundice, and (in some instances) pulmonary infiltrates. From late infancy onward, the presentation is dominated by neurologic manifestations. The youngest children may present with hypotonia and developmental delay, with the subsequent emergence of ataxia, dysarthria, dysphagia, and, in some individuals, epileptic seizures, dystonia, and gelastic cataplexy. Although cognitive impairment may be subtle at first, it eventually becomes apparent that affected individuals have a progressive dementia.
Older teenagers and young adults may present predominantly with apparent early-onset dementia or psychiatric manifestations; however, careful examination usually identifies typical neurologic signs.
Diagnosis/testing.
The diagnosis of NPC is established in a proband with suggestive findings and biallelic pathogenic variants in either NPC1 or NPC2 identified by molecular genetic testing.
Management.
Treatment of manifestations: No curative therapy for NPC exists. Supportive therapy is provided by specialists from multiple disciplines including among others: neurology, physical therapy, occupational therapy, speech therapy, nutrition, feeding, psychology, social work, and medical genetics.
Treatment with miglustat, approved for the management of neurologic manifestations of NPC in several countries but not the United States, has increased survival by five years from date of diagnosis or approximately ten years from onset of neurologic manifestations.
Surveillance: Routine follow up by multidisciplinary specialists to monitor disease progression and supportive management including psychosocial support to identify new manifestations of disease, and, for those on miglustat, to assess compliance, possible side effects, and appearance of conditions that would prompt discontinuation of therapy.
Agents/circumstances to avoid: Drugs that cause excessive salivation or that may exacerbate seizures directly by interacting with antiepileptic drugs; alcohol as well as many drugs that exacerbate ataxia.
Evaluation of relatives at risk: It is appropriate to clarify the genetic status of apparently asymptomatic older and younger at-risk relatives of an affected individual in order to identify as early as possible those who are symptomatic and would benefit from prompt initiation of treatment.
Genetic counseling.
NPC is inherited in an autosomal recessive manner. If both parents are known to be heterozygous for an NPC-related pathogenic variant, each sib of an affected individual has at conception a 25% chance of being affected, a 50% chance of being a heterozygote, and a 25% chance of being unaffected and not a heterozygote. Once the NPC-causing pathogenic variants have been identified in an affected family member, carrier testing for at-risk relatives, prenatal testing for a pregnancy at increased risk, and preimplantation genetic testing are possible.
Diagnosis
No consensus clinical diagnostic criteria for Niemann-Pick disease type C (NPC) have been published.
Suggestive Findings
NPC should be suspected in individuals with the following clinical findings [Patterson et al 2017] (full text) and preliminary laboratory findings.
Clinical Findings
Typical findings. Presentations may be conveniently considered by age of onset, although this grouping is of necessity arbitrary and includes considerable overlap.
- Early infantile (age <2 years). Fetal ascites or neonatal liver disease, particularly when the latter is accompanied by prolonged jaundice and pulmonary infiltrates
- Late infantile (ages 2 to <6 years). Often presents with hypotonia and developmental delay. With time, vertical supranuclear saccadic palsy becomes apparent. Children later develop clumsiness that evolves into ataxia.
- Juvenile (ages 6 to <15 years). These children may present initially with clumsiness that evolves into ataxia, often with academic difficulties that may be misdiagnosed as attention deficit disorder. With time, more global cognitive impairment and regression become evident. Vertical supranuclear gaze palsy (sometimes called vertical supranuclear saccadic paresis) is almost invariably present in children with neurologic manifestations (and is often present before the emergence of other symptoms). Some children develop seizures, gelastic cataplexy, dystonia, and/or spasticity.
- Adolescent/adult (age >15 years). May include all of the neurologic manifestations, which are often overshadowed, at least initially, by cognitive impairment (early-onset dementia) or psychiatric manifestations (e.g., treatment-resistant depression, schizophreniform illness, apparent bipolar disease).
- Other. Some individuals present with isolated splenomegaly in childhood, and may not develop neurologic manifestations for many years. Occasionally, adults have splenomegaly without neurologic manifestations.
Atypical findings include ataxia, splenomegaly, vertical supranuclear gaze palsy, dysarthria, dysphagia, early-onset dementia, treatment-resistant psychiatric symptoms in young adults, gelastic cataplexy, dystonia, and epilepsy (particularly if treatment-resistant) (see Patterson et al [2017], Table 1).
Suspicion index. The sensitivity of a quantitative scoring system that weighs the manifestations of NPC to assist clinicians in identifying individuals appropriate for further laboratory investigation [Wijburg et al 2012] was improved by separating children into two age groups: ≤4 years and >4 years [Pineda et al 2019].
Preliminary Laboratory Findings
Assay of oxysterols has largely replaced skin biopsy (see Clinical Description), and is now regarded as both a robust screening test and a first-line diagnostic test for NPC [Porter et al 2010, Jiang et al 2011, Geberhiwot et al 2018].
Family History
Family history is consistent with autosomal recessive inheritance (e.g., affected sibs and/or parental consanguinity). Absence of a known family history does not preclude the diagnosis.
Establishing the Diagnosis
The diagnosis of NPC is established in a proband with suggestive findings and biallelic pathogenic variants in either NPC1 or NPC2 identified by molecular genetic testing (see Table 1).
Note: Identification of biallelic NPC1 or NPC2 variants of uncertain significance (or identification of one known NPC1 or NPC2 pathogenic variant and one NPC1 or NPC2 variant of uncertain significance) does not establish or rule out a diagnosis of this disorder.
Molecular genetic testing approaches can include a combination of gene-targeted testing (multigene panel) and comprehensive genomic testing (exome sequencing, genome sequencing) depending on the phenotype.
Gene-targeted testing requires that the clinician determine which gene(s) are likely involved, whereas genomic testing does not. Individuals with the distinctive findings described in Suggestive Findings are likely to be diagnosed using gene-targeted testing (see Option 1), whereas those in whom the diagnosis of NPC has not been considered are more likely to be diagnosed using genomic testing (see Option 2).
Option 1
A multigene panel that includes NPC1, NPC2, and other genes of interest (see Differential Diagnosis) is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. Panels to consider include those for lysosomal disorders, treatable neurometabolic disorders, mendelian disorders with psychiatric symptoms, and metabolic nonimmune fetal hydrops. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
Chromosomal microarray analysis (CMA) uses oligonucleotide or SNP arrays to detect genome-wide large deletions/duplications (including NPC1 and NPC2) that cannot be detected by sequence analysis.
Option 2
Comprehensive genomic testing does not require the clinician to determine which gene is likely involved. Exome sequencing is most commonly used; genome sequencing is also possible.
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 1.
Molecular Genetic Testing Used in Niemann-Pick Disease Type C
| Gene 1 | Proportion of NPC Attributed to Pathogenic Variants in Gene | Proportion of Pathogenic Variants 2, 3 Detectable by Method | ||
|---|---|---|---|---|
| Sequence analysis 4 | Gene-targeted deletion/duplication analysis 5 | Chromosomal microarray analysis6 | ||
| NPC1 | 95% | 76% | 22% | 2% |
| NPC2 | 5% | 88% | 12% | 0 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on variants detected in these genes.
- 3.
Data derived from the subscription-based professional view of Human Gene Mutation Database [Stenson et al 2017]
- 4.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 5.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 6.
Chromosomal microarray analysis (CMA) uses oligonucleotide or SNP arrays to detect genome-wide large deletions/duplications (including NPC1 and NPC2) that cannot be detected by other methods of deletion/duplication analysis. The ability to determine the size of the deletion/duplication depends on the type of microarray used and the density of probes in the 18q11
.2 region that includes NPC1, and in the 14q24 .3 region that includes NPC2. CMA designs in current clinical use target these regions.
Clinical Characteristics
Clinical Description
Niemann-Pick disease type C (NPC) is a slowly progressive lysosomal disorder whose principal manifestations are age dependent. The manifestations in the perinatal period and infancy are predominantly visceral, with hepatosplenomegaly, jaundice, and (in some instances) pulmonary infiltrates.
From late infancy onward, the presentation is dominated by neurologic manifestations. The youngest children may present with hypotonia and developmental delay, with the subsequent emergence of ataxia, dysarthria, dysphagia, and (in some individuals) epileptic seizures, dystonia, and gelastic cataplexy. Although cognitive impairment may be subtle at first, it eventually becomes apparent that affected individuals have a progressive dementia.
Older teenagers and young adults may present predominantly with apparent early-onset dementia or psychiatric manifestations; however, careful examination usually identifies typical neurologic signs.
Table 2.
Niemann-Pick Disease Type C: Comparison of Age-Related Phenotypes by Select Features
| Feature | Phenotypes | |||
|---|---|---|---|---|
| Visceral neurodegenerative | Neurodegenerative | Psychiatric- neurodegenerative | ||
| Early infantile (age <2 yrs) | Late infantile (2 to <6 yrs) | Juvenile (6 to <15 yrs) | Adult (>15 yrs) | |
| Hepatomegaly | ● | |||
| Splenomegaly | ● | ● | (●) | |
| Ataxia | ● | ● | ● | |
| Epilepsy | ● | ● | (●) | |
| Cataplexy | (●) | ● | ● | |
| Dementia | (●) | ● | ||
| Psychiatric | ● | |||
| Dystonia | (●) | ● | ● | |
| VSGP | ● | ● | ● | |
VSGP = vertical supranuclear gaze palsy; (●) = sometimes present; ● = usually present
Neonatal and Infantile Presentations
The presentation of NPC in early life is nonspecific and may go unrecognized by inexperienced clinicians. On occasion, ultrasound examination in late pregnancy has detected fetal ascites; infants thus identified typically have severe neonatal liver disease with jaundice and persistent ascites.
Infiltration of the lungs with foam cells may accompany neonatal liver disease or occur as a primary presenting feature (pulmonary failure secondary to impaired diffusion).
Many infants succumb at this stage. Of those who survive, some are hypotonic and delayed in psychomotor development, whereas others may have complete resolution of symptoms, only to present with neurologic disease many years later. Liver and spleen are enlarged in children with symptomatic hepatic disease; however, children who survive often "grow into their organs," so that organomegaly may not be detectable later in childhood. Indeed, many individuals with NPC never have organomegaly. The absence of organomegaly never eliminates the diagnosis of NPC.
Another subgroup of children has minimal or absent hepatic or pulmonary dysfunction and presents primarily with hypotonia and delayed development. Children in this group usually do not have vertical supranuclear gaze palsy (VSGP) at the onset but acquire this sign after a variable period, when other evidence of progressive encephalopathy supervenes.
Childhood Presentations
The classic presentation of NPC is in middle-to-late childhood, with clumsiness and gait disturbance that eventually become frank ataxia. Many observant parents are aware of impaired vertical gaze, which is an early manifestation. VSGP first manifests as increased latency in initiation of vertical saccades, after which saccadic velocity gradually slows and is eventually lost. In late stages of the illness, horizontal saccades are also impaired. The physical manifestations are accompanied by insidiously progressive cognitive impairment, often mistaken at first for simple learning disability. Some children are thought to have primary behavioral disturbances, reflecting unrecognized dyspraxia in some instances. As the disease progresses, it becomes clear that the child is mentally deteriorating.
In addition to the manifestations outlined above, many children develop dystonia, typically beginning as action dystonia in one limb and gradually spreading to involve all of the limbs and axial muscles. Speech gradually deteriorates, with a mixed dysarthria and dysphonia. Dysphagia progresses in parallel with the dysarthria, and oral feeding eventually becomes impossible.
Approximately one third of individuals with NPC have partial and/or generalized seizures. Epilepsy may be refractory to medical therapy in some cases. Seizures usually improve if the child's survival is prolonged, this improvement presumably reflecting continued neuronal loss. About 20% of children with NPC have gelastic cataplexy, a sudden loss of muscle tone evoked by a strong emotional (humorous) stimulus. This can be disabling in those children who experience daily multiple attacks, during which injuries may occur.
Mild demyelinating peripheral neuropathy has been described in a child with otherwise typical late-infantile NPC [Zafeiriou et al 2003]. This finding is likely a rare manifestation of NPC because prospective nerve conduction studies in a cohort of 41 affected individuals participating in a clinical trial of miglustat have identified only one case to date [Patterson, personal communication].
Polysomnographic and biochemical studies have demonstrated disturbed sleep and variable reduction in cerebrospinal fluid hypocretin concentration in individuals with NPC, suggesting that the disease could have a specific impact on hypocretin-secreting cells of the hypothalamus [Kanbayashi et al 2003, Vankova et al 2003].
Death from aspiration pneumonia usually occurs in the late second or third decade [Walterfang et al 2012b].
Adolescent and Adult Presentations
Adolescents or adults may present with neurologic disease as described in the preceding section, albeit with a much slower rate of progression. The author has seen one individual who survived into the seventh decade, having first developed symptoms 25 years earlier. Older individuals may also present with apparent psychiatric illness [Imrie et al 2002, Josephs et al 2003], sometimes appearing to have major depression or schizophrenia. The psychiatric manifestations may overshadow neurologic signs, although the latter can usually be detected with careful examination. An adult presenting with bipolar disorder has been described [Sullivan et al 2005].
A German report describes two individuals with adult-onset dementia associated with frontal lobe atrophy and no visceral manifestations, as is common in adult-onset disease [Klünemann et al 2002].
Other Studies
Imaging. MRI of the brain is usually normal until the late stages of the illness. At that time, marked atrophy of the superior/anterior cerebellar vermis, thinning of the corpus callosum, and mild cerebral atrophy may be seen. Increased signal in the periatrial white matter, reflecting secondary demyelination, may also occur. In one adult, areas of confluent white matter signal hyperintensity mimicked multiple sclerosis [Grau et al 1997]. Quantitative MRI studies in adults with NPC have found widespread gray and white matter abnormalities [Walterfang et al 2010], and reduction in callosal volume as the disease progresses [Walterfang et al 2011]. In addition, the pontine:midbrain ratio correlates with oculomotor function and disease severity [Walterfang et al 2012a].
Studies of magnetic resonance spectroscopy (MRS) suggested that MRS may be a more sensitive imaging technique in NPC than standard MRI [Tedeschi et al 1998]. A French group has reported improvement in MRS parameters with miglustat therapy [Galanaud et al 2009].
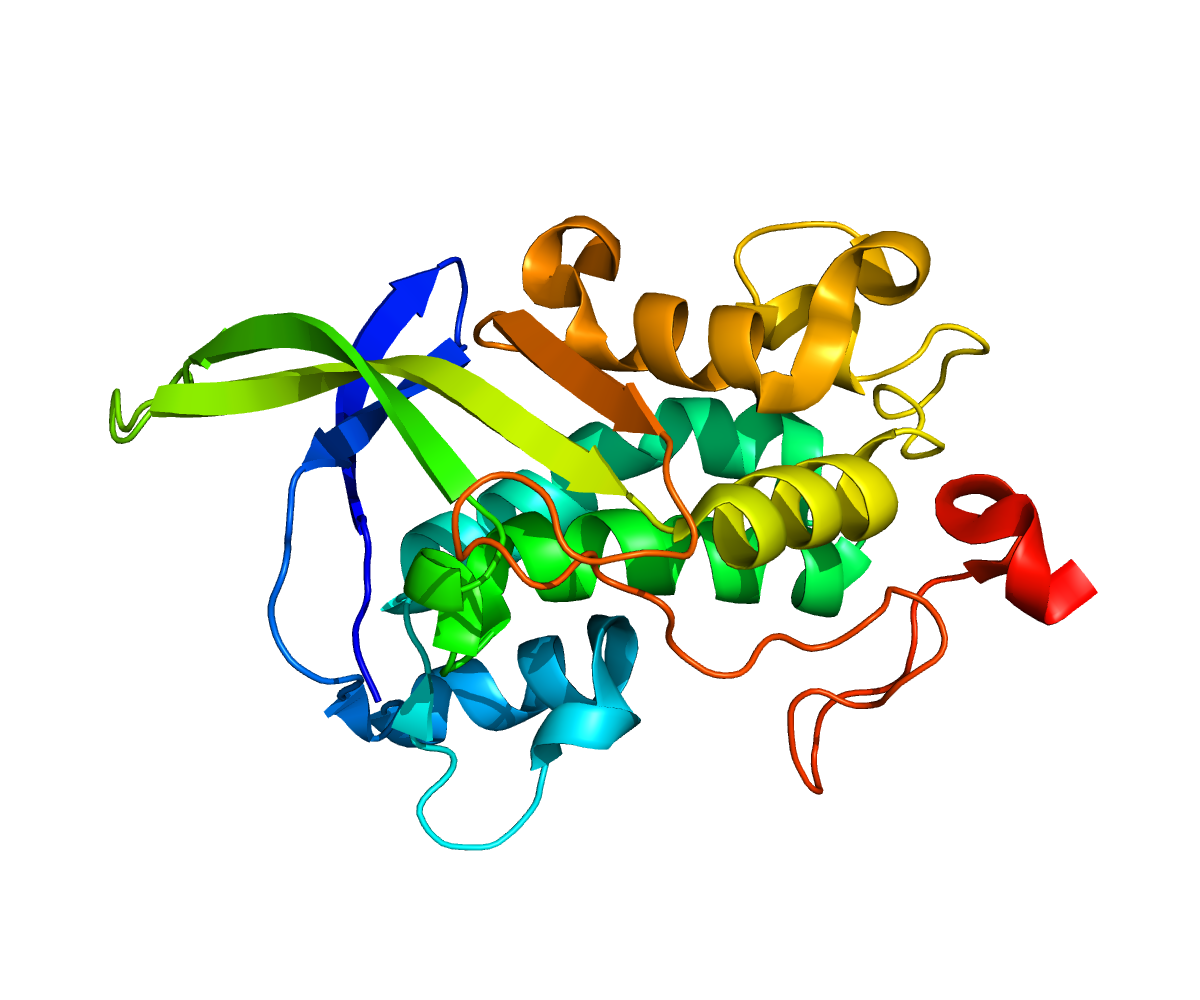
Biochemical. Until recently, definitive diagnosis of NPC required demonstration of abnormal intracellular cholesterol homeostasis in cultured fibroblasts [Pentchev et al 1985]. These cells show reduced ability to esterify cholesterol after loading with exogenously derived LDL cholesterol. Filipin staining demonstrates an intense punctate pattern of fluorescence concentrated around the nucleus, consistent with the accumulation of unesterified cholesterol:
- Classic. Most individuals have zero or very low esterification levels with a classic staining pattern.
- Variant. About 15% of individuals have intermediate or "variant" levels of cholesterol esterification and a less distinctive staining pattern. More precise characterization of the biochemical defect in this group can be achieved by the use of BODIPY-lactosylceramide to identify lipid trafficking abnormalities [Sun et al 2001].
Histology. Other tests, including tissue biopsies and tissue lipid analysis, which were essential for diagnosis before recognition of the biochemical defect in NPC, are now rarely needed. These tests include examination of bone marrow, spleen, and liver, which contain foamy cells (lipid-laden macrophages); sea-blue histiocytes may be seen in the marrow in advanced cases. Electron microscopy of skin, rectal neurons, liver, or brain may show polymorphous cytoplasmic bodies [Boustany et al 1990].
Heterozygotes
In 2004, a report attributed tremor in an individual to presence of a heterozygous NPC1 pathogenic variant [Josephs et al 2004]. More recently a study of 20 obligate heterozygotes for NPC1 pathogenic variants found varying manifestations that are typically seen in compound heterozygotes, including hepatosplenomegaly, increased cholestane triol levels, hyposmia, REM sleep behavior disorder, and typical ocular motor abnormalities [Bremova-Ertl et al 2020]. It will be important for prospective studies of larger cohorts of heterozygotes to confirm these findings.
Genotype-Phenotype Correlations
NPC1. In the approximately 200 pathogenic variants described in NPC1 at the time of the cited studies [Scott & Ioannou 2004, Fernandez-Valero et al 2005], genotype-phenotype correlation was limited because (1) most affected individuals were compound heterozygotes and (2) correlation of the trafficking defects demonstrable in culture and the clinical phenotype was poor.
Nonetheless, the following correlations have been possible for homozygous pathogenic variants and the more common pathogenic variants in the compound heterozygous state:
- No individuals with p.Ile1061Thr had early-infantile NPC in one international study that included the Hispanic population in the upper Rio Grande Valley of the southwestern US, as well as the UK and France [Millat et al 1999].
- Premature-termination-codon variants, variants involving the sterol-sensing domain, and p.Ala1054Thr in the cysteine-rich luminal loop of NPC1 are associated with early-infantile NPC [Millat et al 2001].
- In 40 unrelated individuals of Spanish descent, those who were homozygous for the p.Gln775Pro pathogenic variant had early-infantile NPC and those homozygous for the p.Cys177Tyr pathogenic variant had late-infantile NPC [Fernandez-Valero et al 2005].
- All variants that correlate with the biochemical "variant" phenotype (i.e., patterns of filipin staining in cultured fibroblasts that are less intense than those typically seen in homozygotes or compound heterozygotes and overlap with those seen in heterozygotes) cluster in the cysteine-rich luminal loop [Millat et al 2001].
NPC2
- Of the five pathogenic variants identified by Millat et al [2001], all but c.190+5G>A were associated with early-infantile NPC.
- The two individuals with splice site variants had juvenile-onset disease and prolonged survival.
- Adult-onset disease with frontal lobe atrophy has been described in association with the p.Val39Met variant [Klünemann et al 2002].
- Neonatal or infantile onset and death in early childhood were reported in children homozygous for p.Gln45Ter, p.Cys47Ter, and p.Cys99Arg, whereas prolonged survival into middle adult life has been seen in those homozygous for p.Val39Met and p.Ser67Pro [Chikh et al 2005].
Nomenclature
The older literature on NPC is bedeviled by the large number of terms used to describe individuals now known to have the disease. These include juvenile dystonic idiocy, juvenile dystonic lipidosis, juvenile NPC, neurovisceral lipidosis with vertical supranuclear gaze palsy, Neville-lake disease, sea-blue histiocytosis, lactosylceramidosis, and DAF (downgaze paralysis, ataxia, foam cells) syndrome.
The term Niemann-Pick disease type D describes a genetic isolate from Nova Scotia that is biochemically and clinically indistinguishable from NPC and that also results from biallelic pathogenic variants in NPC1.
The terms Niemann-Pick disease type C1 (NPC1) and Niemann-Pick disease type C2 (NPC2) are now preferred because they correspond with the associated genes (NPC1 and NPC2).
Prevalence
The prevalence of NPC has been estimated at 1:150,000 in Western Europe.
The incidence of NPC in France has been calculated at about 1:120,000, based on the number of postnatally diagnosed individuals in a ten-year period versus the number of births during that same time period. When prenatal cases that did not result in a live-born infant were included, a slightly higher incidence of 1:100,000 was found [Vanier 2010].
The prevalence of NPC in early life is probably underestimated, owing to its nonspecific presentations. The overall prevalence is likely higher than the calculated incidence, owing to relatively prolonged survival in those with later-onset disease, although no comprehensive data are available.
Acadians in Nova Scotia and a Bedouin group in Israel represent genetic isolates with a founder effect (see Table 8).
Differential Diagnosis
Neonatal and infantile presentations include acquired conditions such as biliary atresia, congenital infections (e.g., TORCH), malignancies (leukemia, lymphoma, histiocytosis), and hereditary disorders (see Table 3).
A study from Colorado found that 27% of infants initially diagnosed with idiopathic neonatal cholestasis and 8% of all infants with cholestasis had Niemann-Pick disease type C (NPC) [Yerushalmi et al 2002]. Although this cohort may have been enriched by a local Hispanic genetic isolate, the importance of NPC as a cause of jaundice in infants is appropriately emphasized.
Table 3.
Hereditary Disorders in the Differential Diagnosis of Niemann-Pick Disease Type C – Neonatal and Infantile Presentations
| Gene | Disorder | MOI | Clinical Characteristics |
|---|---|---|---|
| FAH | Tyrosinemia type I | AR | If untreated, usually presents either in young infants w/severe liver involvement or later in 1st yr w/liver dysfunction & significant renal involvement, growth failure, & rickets |
| SERPINA1 | Alpha-1-antitrypsin deficiency | AR | May present w/hepatic dysfunction from infancy, or w/obstructive lung disease &/or bronchiectasis typically after age 30 yrs |
| Storage diseases including: | |||
| GBA | Gaucher disease type 2 (acute or infantile) | AR | CNS involvement, hepatomegaly, splenomegaly, cytopenia, pulmonary disease, & dermatologic changes |
| SMPD1 | Niemann-Pick disease type A | AR | Hepatosplenomegaly is typically noted by age 3 mos; over time liver & spleen become massive. |
| Niemann-Pick disease type B | AR | Later onset & milder in manifestations than NPD-A; hepatosplenomegaly w/progressive hypersplenism & stable liver dysfunction | |
AR = autosomal recessive; MOI = mode of inheritance; NPD-A = Niemann-Pick disease type A
Childhood presentations include acquired conditions such as pineal region or midbrain tumors causing dorsal midbrain syndrome, hydrocephalus, attention-deficit disorder, learning disabilities, absence seizures, other dementing illnesses, pseudodementia (depressive disorder), HIV encephalopathy, sleep disorders, and syncope. Hereditary disorders to consider include subacute necrotizing encephalomyelopathy (see Mitochondrial DNA-Associated Leigh Syndrome and NARP and Nuclear Gene-Encoded Leigh Syndrome Spectrum Overview), mitochondrial disorders, hereditary dystonias, and the conditions summarized in Table 4.
Table 4.
Hereditary Disorders in the Differential Diagnosis of Niemann-Pick Disease Type C – Childhood Presentations
| Gene | Disorder | MOI | Clinical Characteristics |
|---|---|---|---|
| ATP7B | Wilson disease | AR | Can present w/hepatic, neurologic, or psychiatric disturbances |
| BCKDHA BCKDHB DBT | Maple syrup urine disease | AR | |
| HEXA | Juvenile (subacute) hexosaminidase A deficiency | AR | Variable neurologic findings incl progressive dystonia, spinocerebellar degeneration, & motor neuron disease |
| >12 genes 1 | Neuronal ceroid-lipofuscinosis (OMIM PS256730) | AR AD | |
| Amino acidurias & organic acidopathies including: | |||
| GCDH | Glutaric acidemia type 1 | AR | Encephalopathic crises → acute bilateral striatal injury & subsequent complex movement disorders (Insidious-onset basal ganglia injury may develop in absence of identified acute encephalopathic crisis.) |
| Hereditary disorders w/periodic paralysis including: | |||
| CACNA1S SCN4A | Hypokalemic periodic paralysis | AD | Paralytic episodes w/concomitant hypokalemia 2 |
| SCN4A | Hyperkalemic periodic paralysis type 1 | AD | Attacks of flaccid limb weakness; may incl weakness of muscles of eyes, throat, & trunk |
AR = autosomal recessive; AD = autosomal dominant; MOI = mode of inheritance; NPD = Niemann-Pick disease
- 1.
See Phenotypic Series: Ceroid lipofuscinoses for genes associated with this phenotype in OMIM.
- 2.
Serum potassium <3.5 mmol/L
Adolescent and adult presentations include:
- Alzheimer disease, Pick disease (an adult-onset disorder with dementia associated with characteristic neuronal inclusions called Pick bodies, not related to Niemann-Pick disease), frontotemporal dementias (FTD; e.g. CHMP2B-FTD, GRN-FTD, C9orf72 amyotrophic lateral sclerosis and FTD), and Steele-Richardson-Olzewski syndrome (also known as progressive supranuclear palsy; see OMIM 601104)
- Late-onset lysosomal storage diseases
- Syphilis and HIV dementia
- Primary psychiatric illnesses
Management
Clinical management guidelines for Niemann-Pick C (NPC) have been published [Geberhiwot et al 2018] (full text).
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with NPC, the evaluations summarized in Table 5 (if not performed as part of the evaluation that led to the diagnosis) are recommended.
Table 5.
Recommended Evaluations Following Initial Diagnosis in Individuals with Niemann-Pick Disease Type C
| System/Concern | Evaluation | Comment |
|---|---|---|
| Physical exam | Document growth parameters & organomegaly. | |
| Establish current level of disease severity. | Use NPC clinical severity score 1 to document key features at diagnosis. | |
| Neurologic exam | Assess for neurologic features incl spasticity, cataplexy, movement disorders, sleep disturbance, seizures. |
|
| Developmental assessment for children | Developmental assessment |
|
| Cognitive assessment | Document baseline degree of cognitive impairment. | |
| Bowel dysfunction | Medical history for signs/symptoms of constipation | |
| Mobility / Activities of daily living | Assessment of mobility, balance, core stability, trunk control, spasticity, foot posture, & strength by suitably qualified PT | Assess modifications for safety & improved independence. |
| Speech & language | Comprehensive communication eval by speech & language therapist | Assess for need for speech therapy &/or Augmentative and Alternative Communication. |
| Nutrition/ Feeding | Nutritionist / gastroenterology / feeding team |
|
| Cognitive assessment | Document baseline degree of cognitive impairment. | |
| Ophthalmology exam | Neuro-ophthalmologist | Document saccadic eye movement velocity & presence of vertical gaze palsy. |
| Hearing | Audiometry | To document presence of hearing loss |
| Psychiatric eval | Psychiatrist or mental health professional | Assess for psychosis, behavioral disturbances, depression. |
| Genetic counseling | By genetics professionals 2 | To inform patients & their families re nature, MOI, & implications of NPC to facilitate medical & personal decision making |
| Family support/ resources | Providers at specialized care centers, family physician/pediatrician, & local palliative care services should work closely w/patients & families/caregivers through life span, incl: (1) advance care planning w/regular updating; (2) proper flow of communication & info for patients & families; & (3) designated point of contact for each stage in care pathway. | Assess:
|
MOI = mode of inheritance; PT = physical therapist; VFSS = videofluoroscopic swallowing study
- 1.
Geberhiwot et al [2018], Table 4
- 2.
Medical geneticist, certified genetic counselor, or certified advanced genetic nurse
Treatment of Manifestations
No curative therapy for NPC exists.
Supportive therapy by multidisciplinary specialists is summarized in Table 6.
Treatment with miglustat, which was approved for the management of neurologic manifestations of NPC in several countries (but not the United States), follows Table 6.
Table 6.
Treatment of Manifestations in Individuals with Niemann-Pick Disease Type C
| Manifestation/Concern | Treatment | Considerations/Other | |
|---|---|---|---|
| Developmental delay / Intellectual disability | See Developmental Delay / Intellectual Disability Management Issues. | ||
| Neurologic | Spasticity | PT | Antispasticity drugs; rarely surgery |
| Cataplexy | Modafinil, protriptyline | Usually effective & well tolerated | |
| Movement disorders | Trihexyphenydil for dystonia | The effects of this agent may not be sustained. | |
| Sleep disturbance | A nocturnal sedative may be indicated; melatonin is often effective & well tolerated. | Consider formal eval by sleep specialist. | |
| Seizures | Appropriate antiseizure medications for seizure types; no special considerations for NPC | Treatment must be individualized based on seizure semiology & EEG findings. | |
| Bowel dysfunction | Regular bowel program to prevent severe constipation | Constipation may manifest as ↑ seizure frequency &/or ↑ spasticity. | |
| Mobility / Activities of daily living |
| Proactively seek strategies to maintain optimal mobility & ↓ falls such as providing appropriate walking/mobility aids, ankle-foot orthotics, & exercise programs. | |
| Speech & language | Speech therapy | Consider eval for alternative means of communication (e.g., Augmentative and Alternative Communication) for those w/expressive language difficulties. | |
| Nutrition/Feeding | Thickened feeds, small boluses, as tolerated | Consider gastrostomy tube placement when aspiration &/or nutritional compromise is a concern. | |
| Eye movement disorder | No specific therapy, although changes may be slowed by miglustat | ||
| Hearing impairment |
| Use of amplification should be guided by clinical needs & recommendations of treating audiologist. | |
| Psychosis, behavioral disturbances, depression | Appropriate psychotropic medications & supportive counseling | Psychiatric manifestations may be resistant to standard drug therapies. | |
| Family/caregiver needs | General supportive care incl respite for primary caregivers is crucial to maintenance of family unit. | ||
PT = physical therapy
Developmental Delay / Intellectual Disability Management Issues
The following information represents typical management recommendations for individuals with developmental delay / intellectual disability in the United States; standard recommendations may vary from country to country.
Ages 0-3 years. Referral to an early intervention program is recommended for access to occupational, physical, speech, and feeding therapy as well as infant mental health services, special educators, and sensory impairment specialists. In the US, early intervention is a federally funded program available in all states that provides in-home services to target individual therapy needs.
Ages 3-5 years. In the US, developmental preschool through the local public school district is recommended. Before placement, an evaluation is made to determine needed services and therapies and an individualized education plan (IEP) is developed for those who qualify based on established motor, language, social, or cognitive delay. The early intervention program typically assists with this transition. Developmental preschool is center based; for children too medically unstable to attend, home-based services are provided.
All ages. Consultation with a developmental pediatrician is recommended to ensure the involvement of appropriate community, state, and educational agencies (US) and to support parents in maximizing quality of life. Some issues to consider:
- IEP services:
- An IEP provides specially designed instruction and related services to children who qualify.
- IEP services will be reviewed annually to determine whether any changes are needed.
- As required by special education law, children should be in the least restrictive environment feasible at school and included in general education as much as possible and when appropriate.
- Vision and hearing consultants should be a part of the child's IEP team to support access to academic material.
- PT, OT, and speech services will be provided in the IEP to the extent that the need affects the child's access to academic material. Beyond that, private supportive therapies based on the affected individual's needs may be considered. Specific recommendations regarding type of therapy can be made by a developmental pediatrician.
- As a child enters the teen years, a transition plan should be discussed and incorporated in the IEP. For those receiving IEP services, the public school district is required to provide services until age 21.
- A 504 plan (Section 504: a US federal statute that prohibits discrimination based on disability) can be considered for those who require accommodations or modifications such as front-of-class seating, assistive technology devices, classroom scribes, extra time between classes, modified assignments, and enlarged text.
- Developmental Disabilities Administration (DDA) enrollment is recommended. DDA is a US public agency that provides services and support to qualified individuals. Eligibility differs by state but is typically determined by diagnosis and/or associated cognitive/adaptive disabilities.
- Families with limited income and resources may also qualify for supplemental security income (SSI) for their child with a disability.
Treatment with Miglustat
Based on clinical studies that supported a role of miglustat in stabilizing mice with the murine NPC, miglustat was approved for the management of neurologic manifestations of NPC in several countries [Patterson et al 2012], but not the United States. A recent literature review of the effect of miglustat on clinical, biomarker, and imaging measures supported its efficacy in ameliorating the course of NPC [Pineda et al 2018]. Analysis of data on long-term survival in NPC from several historical data sets as well as a prospective registry suggested that individuals treated with miglustat experienced a mean increase in survival of five years when measured from date of diagnosis or approximately ten years when measured from onset of neurologic manifestations [Patterson et al 2020]. This positive effect was supported by a three-year (median) prospective study of 50 individuals with NPC taking miglustat in whom swallowing function and the risk of aspiration stabilized [Solomon et al 2020].
Thus, in countries where it is an approved therapy, individuals with a confirmed diagnosis of NPC should be considered for miglustat therapy, except individuals with NPC who:
- Have advanced neurologic disease / dementia
- Have another life-threatening illness and an estimated life span <1 year
- Have only spleen/liver enlargement
- Are presymptomatic
Note that miglustat may produce loose stools and excessive flatus; these effects may be managed with dietary modification (by reduction or removal of lactose and other sugars). Physiologic tremor may be enhanced in some individuals.
Surveillance
Table 7.
Recommended Surveillance for Individuals with Niemann-Pick Disease Type C
| System/Concern | Evaluation | Frequency |
|---|---|---|
| Interval medical history | Establish rate of disease progression. | Every 6 mos |
| For those on miglustat therapy | Monitor for:
| Review every 6 mos for indications, efficacy, & adverse effects. |
| Physical exam | Document growth parameters, assess for neurologic features & organomegaly. | Every 6-12 mos |
| NPC clinical severity score 1 | Document progression & response to therapy of key disease features. | Every 6 mos |
| Mobility / Activities of daily living | Assessment of mobility, balance, core stability, trunk control, spasticity, foot posture, & strength by suitably qualified PT | Every 6 mos in children; every 12 mos in adults |
| Developmental or cognitive assessment | Monitor educational needs in children & cognitive abilities in adults. | |
| Speech & language | Comprehensive communication eval by speech & language therapist | |
| Ophthalmology assessment | Document progression of saccadic eye movement velocity & presence of gaze palsy, response to miglustat therapy. | At 6 and 12 mos; after starting treatment; frequency after 12 mos TBD by clinical response |
| Hearing impairment | Audiometry for new-onset hearing loss or its progression | Every 12 mos |
| Nutrition/Feeding | Document nutritional status, presence/progression of dysphagia, & aspiration risk. | Every 6 mos in children; in adults, frequency could be ↓ to every 12 mos if asymptomatic & disease is stable |
| Psychosis, behavioral disturbances, & depression | By mental health care provider |
|
| Sleep hygiene | Medical history for sleep disturbances | Review every 12 mos. |
| Driving | Monitor those who hold a driver's license for relevant motor &/or sensory impairments. | Every 12 mos |
| Family/caregiver needs |
| Every 6-12 mos |
PT = physical therapist
- 1.
Geberhiwot et al [2018], Table 4
Agents/Circumstances to Avoid
Avoid the following:
- Drugs that cause excessive salivation or that may exacerbate seizures directly by interacting with antiepileptic drugs
- Alcohol as well as many drugs that exacerbate ataxia
Evaluation of Relatives at Risk
It is appropriate to clarify the genetic status of apparently asymptomatic older and younger at-risk relatives of an affected individual in order to identify as early as possible those who are symptomatic and would benefit from prompt initiation of treatment (see Table 6).
See Genetic Counseling for issues related to testing of at-risk relatives for genetic counseling purposes.
Therapies Under Investigation
Based on results of studies of hydroxypropyl beta cyclodextrin in the murine model of NPC [Abi-Mosleh et al 2009, Davidson et al 2009], uncontrolled clinical studies of intrathecal 2-hydroxypropyl-β-cyclodextrin suggested amelioration of disease progression [Ory et al 2017, Berry-Kravis et al 2018]. However, a recent controlled clinical trial of this therapy (ClinicalTrials.gov identifier: NCT02534844) failed to show a difference between controls and the intervention group [publicly presented, unpublished data]. Further investigations of this therapy are in progress.
Studies of intravenous and combined intravenous and intrathecal cyclodextrins are currently in progress.
Studies of recombinant human heat shock protein 70 [rh HSP70] in tissue culture and animal models suggested potential benefit in NPC and other lysosomal diseases [Kirkegaard et al 2016]. Because the administration of rh HSP70 was not feasible for humans, a controlled trial of arimoclomol, an agent known to induce the expression of HSP70, was undertaken (ClinicalTrials.gov identifier: NCT02612129). The results of this trial, which demonstrated slowing of disease progression over the course of one year, have been publicly presented, but not yet published. A new drug application is currently under consideration by the FDA.
N-acetyl-L-leucine has shown benefit in ameliorating ataxia in NPC (and ataxia in several other disorders) in open label studies [Kalla & Strupp 2019]. A controlled clinical trial is currently in progress (ClinicalTrials.gov identifier: NCT03759639).
Treatment of certain NPC fibroblast cell lines with an HDAC inhibitor produced marked reduction of cholesterol storage [Pipalia et al 2011]; a Phase I/II clinical trial (ClinicalTrials.gov identifier: NCT02124083) has been completed, but no results have been reported.
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for access to information on clinical studies for a wide range of diseases and conditions.