Isovaleric Acidemia
A number sign (#) is used with this entry because of evidence that isovaleric acidemia (IVA) is caused by homozygous mutation in the isovaleryl CoA dehydrogenase gene (IVD; 607036) on chromosome 15q15.
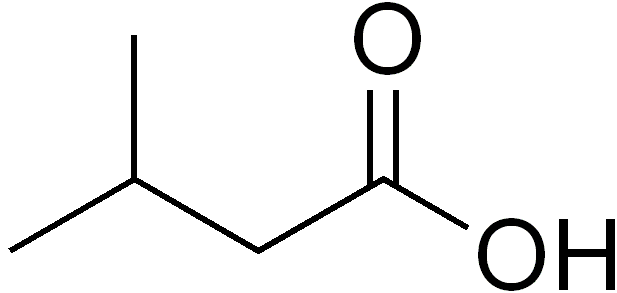
DescriptionIsovaleric acidemia is an inborn error of leucine metabolism caused by a deficiency of isovaleryl-CoA dehydrogenase. It can present with severe neonatal ketoacidosis leading to death, but in milder cases recurrent episodes of ketoacidosis of varying degree occur later in infancy and childhood (summary by Vockley et al., 1991).
Clinical FeaturesTwo forms of isovaleric acidemia are recognized: the acute neonatal form, leading to massive metabolic acidosis from the first days of life and rapid death (e.g., Newman et al., 1967), and a chronic form in which periodic attacks of severe ketoacidosis occur with asymptomatic intervening periods (e.g., Tanaka et al., 1966).
Budd et al. (1967) observed brother and sister who, before the age of 6 months, showed retarded psychomotor development, a peculiar odor resembling sweaty feet, an aversion to dietary protein, and pernicious vomiting, leading to acidosis and coma. The unusual smell was identified as isovaleric acid, an intermediary of leucine, by experts of the Arthur D. Little Co., Industrial Consultants, Cambridge, Mass.
Sidbury et al. (1967) observed that 3 of 4 children of a second-cousin marriage died in the first 2 weeks of life with the following symptoms after the first 3 days: convulsions, lethargy, dehydration, moderate hepatomegaly, depressed platelets and leukocytes, and an unusual urinary odor like that of sweaty feet. Postmortem examination showed mainly changes related to the hematologic findings: hypoplastic marrow, scattered hemorrhages of viscera, and terminal septicemia. The unusual odor was the result of butyric and hexanoic acids. They suggested that it is an inborn error of short-chain fatty acid metabolism and, more specifically, that a defect in green acyl dehydrogenase may be involved. In a second family a brother and sister with unrelated parents had a similar ailment. These cases are considered to have been instances of isovaleric acidemia.
Ando et al. (1971) showed that isovaleric acidemia can produce hyperglycinemia and leukopenia, as well as episodic ketoacidosis, thus resembling propionic acidemia and methylmalonic acidemia.
Gerdes et al. (1988) described a patient with the chronic intermittent type of the disease, who was born to unrelated Icelandic parents.
In a review of inherited metabolic disorders and stroke, Testai and Gorelick (2010) noted that patients with branched-chain organic aciduria, including isovaleric aciduria, propionic aciduria (606054), and methylmalonic aciduria (251000) can rarely have strokes. Cerebellar hemorrhage has been described in all 3 disorders, and basal ganglia ischemic stroke has been described in propionic aciduria and methylmalonic aciduria. These events may occur in the absence of metabolic decompensation.
Clinical ManagementCohn et al. (1978) demonstrated that administration of glycine reduces isovaleric acidemia in neonates by conjugating isovaleric acid, with urinary excretion of the conjugate. Naglak et al. (1988) also demonstrated that, in addition to restriction of leucine intake, glycine supplementation can be useful in management. They suggested that clinical and biochemical measures should be used as guides to determine the amount of leucine that can be tolerated and the optimum glycine supplement for each patient.
PathogenesisThe phenotypic abnormalities in this disorder result from an accumulation of isovaleric acid, which is toxic to the central nervous system. An alternative pathway through glycine-N-acylase (EC 2.3.1.13) allows detoxification by producing isovalerylglycine, which is excreted.
Rhead and Tanaka (1980) demonstrated a specific deficiency of mitochondrial isovaleryl-CoA dehydrogenase activity in skin fibroblasts from patients with IVA. Mitochondrial butyryl-CoA dehydrogenase activity was maintained at normal levels. Although clinical heterogeneity is observed, cell-fusion studies (Dubiel et al., 1983) involving 12 cell lines, each from a different patient and representing a variety of clinical presentation, showed no complementation. Complementation was observed when IVA cells were fused with those from glutaric aciduria IIB (231680). The authors concluded that the same gene, coding for isovaleryl CoA dehydrogenase, was mutated in all cell lines.
Molecular GeneticsDespite the findings from complementation studies indicating the involvement of a single IVD gene in this disorder (Dubiel et al., 1983), analysis of the variant enzyme in 15 IVA fibroblast cell lines showed 5 distinct classes of variants which differed in subunit molecular size. Ikeda et al. (1985) suggested that these variants, in which residual enzyme activity was reduced to 0 to 3% of normal, were caused by point mutations or premature terminations.
In a patient with type I isovaleric acidemia, Vockley et al. (1991) demonstrated a change of thymine-125 to cytosine in the IVD gene, which was predicted to cause a substitution of proline for leucine at position 13 of the mature IVD protein (L13P; 607036.0001).
Since the implementation, in many states and countries, of newborn screening by tandem mass spectrometry, presymptomatic diagnosis of isovaleric acidemia has been possible. Molecular genetic analysis of the IVD gene in 19 subjects whose condition was detected through newborn screening led to the identification of 1 recurring mutation, 932C-T (A282V; 607036.0007) in 47% of mutant alleles (Ensenauer et al., 2004). Surprisingly, family studies identified 6 healthy older sibs with identical genotype and biochemical evidence of isovaleric acidemia. The findings indicated the frequent occurrence of a novel mild and potentially asymptomatic phenotype of IVA. This has significant consequences for patient management and counseling.