Acute Intermittent Porphyria
A rare, severe form of the acute hepatic porphyrias characterized by the occurrence of neuro-visceral attacks without cutaneous manifestations.
Clinical description
Patients suffer intermittent neuro-visceral attacks that can persist for several days and that repeat over several weeks. These attacks manifest as intense abdominal pain (>95% of cases) and neurological and/or psychological symptoms. The abdominal pain is often associated with lumbago irradiating to the thighs, and with nausea, vomiting and relentless constipation. Psychological symptoms are variable: irritability, emotionality, depression, considerable anxiety and, more rarely, auditory and visual hallucinations, disorientation, mental confusion. Neurological manifestations can affect the central nervous system as much as the peripheral nervous system (myalgia, paresis, ascending flaccid paralysis of the limbs, or convulsions) and can lead to severe complications such as motor paralysis. Tachycardia and hyponatremia are common during attacks. In cases with cardiac arrhythmia and respiratory paralysis (rare), attacks can be fatal. The attacks are most commonly triggered by exogenous factors (porphyrinogenic drugs, alcohol, infections, a hypo-calorific diet, stress), and/or endogenous factors (hormonal, linked to menstrual cycle).
Etiology
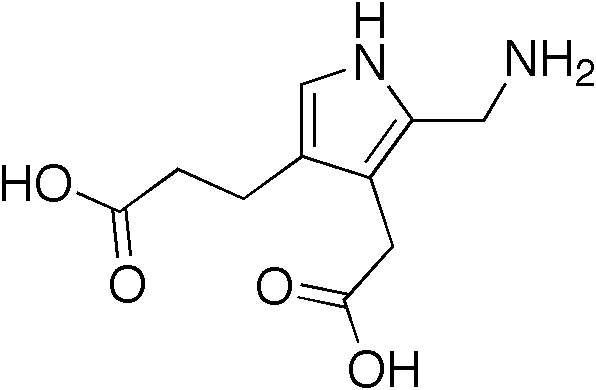
Acute intermittent porphyria is caused by a deficiency of porphobilinogen deaminase (PBG-D; the third enzyme in the heme biosynthesis pathway) that leads to an accumulation of the precursors of porphyrins in the liver (delta-aminolevulinic acid, ALA and porphobilinogen, PBG). The enzyme deficiency is caused by mutations of the HMBS gene (11q23.3) coding for PBG-D. Transmission is autosomal dominant and penetrance is very weak.
Diagnostic methods
The observation of urine that is pink orred after exposure to light evokes the diagnosis of the disease. Diagnosis is based on the evidence of elevated concentrations of PBG and ALA in the urine and residual PBG-D activity in 50% of red blood cells (not always found during attacks). Diagnosis can be confirmed by the identification of a causal mutation of the HMBS gene.
Differential diagnosis
Differential diagnoses with other acute hepatic porphyrias is dependent on the concentration of porphrins in urine and, particularly, in stools and plasma.
Genetic counseling
Genetic counseling should be offered to patients and their families to identify individuals susceptible to developing or transmitting the disease.
Management and treatment
When an acute attack is confirmed, urgent treatment with an injection of human hemin and/or perfusion of carbohydrates is required. Management includes the suppression of triggering factors, relief from pain (opiates), vomiting and anxiety, and the prevention of attacks (by avoiding triggering factors, particularly drugs).
Prognosis
In certain patients attacks recur, resulting in the need for repeated and more frequent injections of human hemin. Crippling attacks can possibly indicate the need for a hepatic transplant. However, in the majority of cases, no attacks of acute intermittent porphyria occur during all adult life and the disease is rarely progressive.