Lung Cancer
Lung cancer, also known as lung carcinoma, is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung. This growth can spread beyond the lung by the process of metastasis into nearby tissue or other parts of the body. Most cancers that start in the lung, known as primary lung cancers, are carcinomas. The two main types are small-cell lung carcinoma (SCLC) and non-small-cell lung carcinoma (NSCLC). The most common symptoms are coughing (including coughing up blood), weight loss, shortness of breath, and chest pains.
The vast majority (85%) of cases of lung cancer are due to long-term tobacco smoking. About 10–15% of cases occur in people who have never smoked. These cases are often caused by a combination of genetic factors and exposure to radon gas, asbestos, second-hand smoke, or other forms of air pollution. Lung cancer may be seen on chest radiographs and computed tomography (CT) scans. The diagnosis is confirmed by biopsy which is usually performed by bronchoscopy or CT-guidance.
Avoidance of risk factors, including smoking and air pollution, is the primary method of prevention. Treatment and long-term outcomes depend on the type of cancer, the stage (degree of spread), and the person's overall health. Most cases are not curable. Common treatments include surgery, chemotherapy, and radiotherapy. NSCLC is sometimes treated with surgery, whereas SCLC usually responds better to chemotherapy and radiotherapy.
Worldwide in 2012, lung cancer occurred in 1.8 million people and resulted in 1.6 million deaths. This makes it the most common cause of cancer-related death in men and second most common in women after breast cancer. The most common age at diagnosis is 70 years. In the United States, five-year survival rate is 19.4%, while in Japan it is 41.4%. Outcomes on average are worse in the developing world.
Signs and symptoms
Signs and symptoms which may suggest lung cancer include:
- Respiratory symptoms: coughing, coughing up blood, wheezing, or shortness of breath
- Systemic symptoms: weight loss, weakness, fever, or clubbing of the fingernails
- Symptoms due to the cancer mass pressing on adjacent structures: chest pain, bone pain, superior vena cava obstruction, or difficulty swallowing
If the cancer grows in the airways, it may obstruct airflow, causing breathing difficulties. The obstruction can also lead to accumulation of secretions behind the blockage, and increase the risk of pneumonia.
Depending on the type of tumor, paraneoplastic phenomena — symptoms not due to the local presence of cancer — may initially attract attention to the disease. In lung cancer, these phenomena may include hypercalcemia, syndrome of inappropriate antidiuretic hormone (SIADH, abnormally concentrated urine and diluted blood), ectopic ACTH production, or Lambert–Eaton myasthenic syndrome (muscle weakness due to autoantibodies). Tumors in the top of the lung, known as Pancoast tumors, may invade the local part of the sympathetic nervous system, resulting in Horner's syndrome (dropping of the eyelid and a small pupil on that side), as well as damage to the brachial plexus.
Many of the symptoms of lung cancer (poor appetite, weight loss, fever, fatigue) are not specific. In many people, the cancer has already spread beyond the original site by the time they have symptoms and seek medical attention. Symptoms that suggest the presence of metastatic disease include weight loss, bone pain, and neurological symptoms (headaches, fainting, convulsions, or limb weakness). Common sites of spread include the brain, bone, adrenal glands, opposite lung, liver, pericardium, and kidneys. About 10% of people with lung cancer do not have symptoms at diagnosis; these cancers are incidentally found on routine chest radiography.
Causes

Cancer develops after genetic damage to DNA and epigenetic changes. Those changes affect the cell's normal functions, including cell proliferation, programmed cell death (apoptosis), and DNA repair. As more damage accumulates, the risk for cancer increases.
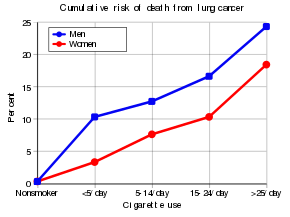
Smoking
Tobacco smoking is by far the main contributor to lung cancer. Cigarette smoke contains at least 73 known carcinogens, including benzo[a]pyrene, NNK, 1,3-butadiene, and a radioactive isotope of polonium – polonium-210. Across the developed world, 90% of lung cancer deaths in men and 70% of those in women during the year 2000 were attributed to smoking. Smoking accounts for about 85% of lung cancer cases. A 2014 review found that vaping may be a risk factor for lung cancer but less than that of cigarettes.
Passive smoking – the inhalation of smoke from another's smoking – is a cause of lung cancer in nonsmokers. A passive smoker can be defined as someone either living or working with a smoker. Studies from the US, the UK and other European countries have consistently shown a significantly-increased risk among those exposed to passive smoking. Those who live with someone who smokes have a 20–30% increase in risk while those who work in an environment with secondhand smoke have a 16–19% increase in risk. Investigations of sidestream smoke suggest that it is more dangerous than direct smoke. Passive smoking results in roughly 3,400 lung cancer-related deaths each year in the US.
Marijuana smoke contains many of the same carcinogens as those found in tobacco smoke, however, the effect of smoking cannabis on lung cancer risk is not clear. A 2013 review did not find an increased risk from light to moderate use. A 2014 review found that smoking cannabis doubled the risk of lung cancer, though cannabis is in many countries commonly mixed with tobacco.
Radon gas
Radon is a colorless and odorless gas generated by the breakdown of radioactive radium, which in turn is the decay product of uranium, found in the Earth's crust. The radiation decay products ionize genetic material, causing mutations that sometimes become cancerous. Radon is the second most-common cause of lung cancer in the US, causing about 21,000 deaths each year. The risk increases 8–16% for every 100 Bq/m³ increase in the radon concentration. Radon gas levels vary by locality and the composition of the underlying soil and rocks. About one in 15 homes in the US have radon levels above the recommended guideline of 4 picocuries per liter (pCi/l) (148 Bq/m³).
Asbestos
Asbestos can cause a variety of lung diseases such as lung cancer. Tobacco smoking and asbestos both have synergistic effects on the development of lung cancer. In smokers who work with asbestos, the risk of lung cancer is increased 45-fold compared to the general population. Asbestos can also cause cancer of the pleura, called mesothelioma – which actually is different from lung cancer.
Air pollution
Outdoor air pollutants, especially chemicals released from the burning of fossil fuels, increase the risk of lung cancer. Fine particulates (PM2.5) and sulfate aerosols, which may be released in traffic exhaust fumes, are associated with a slightly-increased risk. For nitrogen dioxide, an incremental increase of 10 parts per billion increases the risk of lung cancer by 14%. Outdoor air pollution is estimated to cause 1–2% of lung cancers.
Tentative evidence supports an increased risk of lung cancer from indoor air pollution in relation to the burning of wood, charcoal, dung, or crop residue for cooking and heating. Women who are exposed to indoor coal smoke have roughly twice the risk, and many of the by-products of burning biomass are known or suspected carcinogens. This risk affects about 2.4 billion people worldwide, and it is believed to result in 1.5% of lung cancer deaths.
Genetics
About 8% of lung cancer is caused by inherited factors. In relatives of people that are diagnosed with lung cancer, the risk is doubled, likely due to a combination of genes. Polymorphisms on chromosomes 5, 6, and 15 are known to affect the risk of lung cancer. Single-nucleotide polymorphisms (SNPs) of the genes encoding the nicotinic acetylcholine receptor (nAChR) – CHRNA5, CHRNA3, and CHRNB4 – are of those associated with an increased risk of lung cancer, as well as RGS17 – a gene regulating G-protein signaling.
Other causes
Numerous other substances, occupations, and environmental exposures have been linked to lung cancer. The International Agency for Research on Cancer (IARC) states that there is some "sufficient evidence" to show that the following are carcinogenic in the lungs:
- Some metals (aluminium production, cadmium and cadmium compounds, chromium(VI) compounds, beryllium and beryllium compounds, iron and steel founding, nickel compounds, arsenic and inorganic arsenic compounds, and underground hematite mining)
- Some products of combustion (incomplete combustion, coal (indoor emissions from household coal burning), coal gasification, coal-tar pitch, coke production, soot, and diesel engine exhaust)
- Ionizing radiation (X-ray and gamma)
- Some toxic gases (methyl ether (technical grade), and bis-(chloromethyl) ether, sulfur mustard, MOPP (vincristine-prednisone-nitrogen mustard-procarbazine mixture) and fumes from painting)
- Rubber production and crystalline silica dust
- There is a small increase in the risk of lung cancer in people affected by systemic sclerosis.
Pathogenesis
Similar to many other cancers, lung cancer is initiated by either the activation of oncogenes or the inactivation of tumor suppressor genes. Carcinogens cause mutations in these genes that induce the development of cancer.
Mutations in the K-ras proto-oncogene contribute to roughly 10–30% of lung adenocarcinomas. Nearly 4% of non-small-cell lung carcinomas involve an EML4-ALK tyrosine kinase fusion gene.
Epigenetic changes such as alteration of DNA methylation, histone tail modification, or microRNA regulation may result in the inactivation of tumor suppressor genes. Importantly, cancer cells develop resistance to oxidative stress, which enables them to withstand and exacerbate inflammatory conditions that inhibit the activity of the immune system against the tumor.
The epidermal growth factor receptor (EGFR) regulates cell proliferation, apoptosis, angiogenesis, and tumor invasion. Mutations and amplification of EGFR are common in non-small-cell lung carcinoma, and they provide the basis for treatment with EGFR-inhibitors. Her2/neu is affected less frequently. Other genes that are often mutated or amplified include c-MET, NKX2-1, LKB1, PIK3CA, and BRAF.
The cell lines of origin are not fully understood. The mechanism may involve the abnormal activation of stem cells. In the proximal airways, stem cells that express keratin 5 are more likely to be affected, typically leading to squamous-cell lung carcinoma. In the middle airways, implicated stem cells include club cells and neuroepithelial cells that express club cell secretory protein. Small-cell lung carcinoma may originate from these cell lines or neuroendocrine cells, and it may express CD44.
Metastasis of lung cancer requires transition from epithelial to mesenchymal cell type. This may occur through the activation of signaling pathways such as Akt/GSK3Beta, MEK-ERK, Fas, and Par6.
Diagnosis


Performing a chest radiograph is one of the first investigative steps if a person reports symptoms that may be suggestive of lung cancer. This may reveal an obvious mass, the widening of the mediastinum (suggestive of spread to lymph nodes there), atelectasis (lung collapse), consolidation (pneumonia), or pleural effusion. CT imaging of the chest may reveal a spiculated mass which is highly suggestive of lung cancer, and is also used to provide more information about the type and extent of disease. Bronchoscopic or CT-guided biopsy is often used to sample the tumor for histopathology.
Lung cancer often appears as a solitary pulmonary nodule on a chest radiograph. However, the differential diagnosis is wide. Many other diseases can also give this appearance, including metastatic cancer, hamartomas, and infectious granulomas caused by tuberculosis, histoplasmosis or coccidioidomycosis. Lung cancer can also be an incidental finding, as a solitary pulmonary nodule on a chest radiograph or CT scan done for an unrelated reason. The definitive diagnosis of lung cancer is based on the histological examination of the suspicious tissue in the context of the clinical and radiological features.
Clinical practice guidelines recommend frequencies for pulmonary nodule surveillance. CT imaging should not be used for longer or more frequently than indicated, as the extended surveillance exposes people to increased radiation and is costly.
Classification

| Histological type | Incidence per 100,000 per year |
|---|---|
| All types | 66.9 |
| Adenocarcinoma | 22.1 |
| Squamous-cell carcinoma | 14.4 |
| Small-cell carcinoma | 9.8 |
Lung cancers are classified according to histological type. This classification is important for determining both the management and predicting outcomes of the disease. Lung cancers are carcinomas – malignancies that arise from epithelial cells. Lung carcinomas are categorized by the size and appearance of the malignant cells seen by a histopathologist under a microscope. For therapeutic purposes, two broad classes are distinguished: non-small-cell lung carcinoma and small-cell lung carcinoma.
Non-small-cell lung carcinoma

The three main subtypes of NSCLC are adenocarcinoma, squamous-cell carcinoma, and large-cell carcinoma. Rare subtypes include pulmonary enteric adenocarcinoma.
Nearly 40% of lung cancers are adenocarcinoma, which usually comes from peripheral lung tissue. Although most cases of adenocarcinoma are associated with smoking, adenocarcinoma is also the most-common form of lung cancer among people who have smoked fewer than 100 cigarettes in their lifetimes ("never-smokers") and ex-smokers with a modest smoking history. A subtype of adenocarcinoma, the bronchioloalveolar carcinoma, is more common in female never-smokers, and may have a better long-term survival.
Squamous-cell carcinoma causes about 30% of lung cancers. They typically occur close to large airways. A hollow cavity and associated cell death are commonly found at the center of the tumor.
About 10 to 15% of lung cancers are large-cell carcinoma. These are so named because the cancer cells are large, with excess cytoplasm, large nuclei, and conspicuous nucleoli.
Small-cell lung carcinoma

In SCLC, the cells contain dense neurosecretory granules (vesicles containing neuroendocrine hormones), which give this tumor an endocrine or paraneoplastic syndrome association. Most cases arise in the larger airways (primary and secondary bronchi). Sixty to seventy percent have extensive disease (which cannot be targeted within a single radiation therapy field) at presentation.
Others
Four main histological subtypes are recognised, although some cancers may contain a combination of different subtypes, such as adenosquamous carcinoma. Rare subtypes include carcinoid tumors, bronchial gland carcinomas, and sarcomatoid carcinomas.
Metastasis
| Histological type | Napsin-A | TTF-1 |
|---|---|---|
| Squamous-cell carcinoma | Negative | Negative |
| Adenocarcinoma | Positive | Positive |
| Small-cell carcinoma | Negative | Positive |
The lungs are a common place for the spread of tumors from other parts of the body. Secondary cancers are classified by the site of origin; for example, breast cancer that has been spread to the lung is called metastatic breast cancer. Metastases often have a characteristic round appearance on chest radiograph.
Primary lung cancers also most commonly metastasize to the brain, bones, liver, and adrenal glands. Immunostaining of a biopsy usually helps determine the original source. The presence of Napsin-A, TTF-1, CK7, and CK20 help confirm the subtype of lung carcinoma. SCLC that originates from neuroendocrine cells may express CD56, neural cell adhesion molecule, synaptophysin, or chromogranin.
Staging
Lung cancer staging is an assessment of the degree of spread of the cancer from its original source. It is one of the factors affecting both the prognosis and the potential treatment of lung cancer.
The evaluation of non-small-cell lung carcinoma (NSCLC) staging uses the TNM classification (tumor, node, metastasis). This is based on the size of the primary tumor, lymph node involvement, and distant metastasis.
|
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Using the TNM descriptors, a group is assigned, ranging from occult cancer, through stages 0, IA (one-A), IB, IIA, IIB, IIIA, IIIB, and IV (four). This stage group assists with the choice of treatment and estimation of prognosis.
| TNM | Stage group |
|---|---|
| T1a–T1b N0 M0 | IA |
| T2a N0 M0 | IB |
| T1a–T2a N1 M0 | IIA |
| T2b N0 M0 | |
| T2b N1 M0 | IIB |
| T3 N0 M0 | |
| T1a–T3 N2 M0 | IIIA |
| T3 N1 M0 | |
| T4 N0–N1 M0 | |
| N3 M0 | IIIB |
| T4 N2 M0 | |
| M1 | IV |
SCLC has traditionally been classified as "limited stage" (confined to one-half of the chest and within the scope of a single tolerable radiotherapy field) or "extensive stage" (more widespread disease). However, the TNM classification and grouping are useful in estimating prognosis.
For both NSCLC and SCLC, the two general types of staging evaluations are clinical staging and surgical staging. Clinical staging is performed before definitive surgery. It is based on the results of imaging studies (such as CT scans and PET scans) and biopsy results. Surgical staging is evaluated either during or after the operation. It is based on the combined results of surgical and clinical findings, including surgical sampling of thoracic lymph nodes.
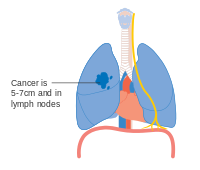
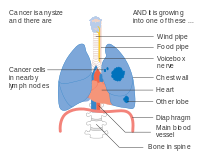
- Diagrams of main features of staging

Stage IA and IB lung cancer

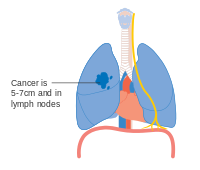
Stage IIA lung cancer
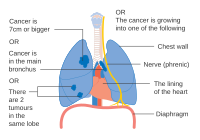
Stage IIB lung cancer
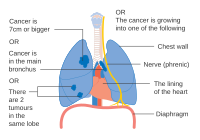
One option for stage IIB lung cancer, with T2b; but if tumor is within 2 cm of the carina, this is stage 3

Stage IIIA lung cancer

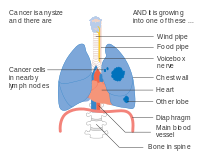
Stage IIIA lung cancer, if there is one feature from the list on each side
Stage IIIA lung cancer

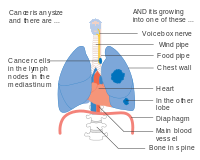
Stage IIIB lung cancer
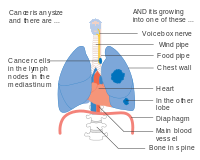
Stage IIIB lung cancer

Stage IV lung cancer
Prevention

Smoking prevention and smoking cessation are effective ways of preventing the development of lung cancer.
Smoking ban
While in most countries industrial and domestic carcinogens have been identified and banned, tobacco smoking is still widespread. Eliminating tobacco smoking is a primary goal in the prevention of lung cancer, and smoking cessation is an important preventive tool in this process.
Policy interventions to decrease passive smoking in public areas such as restaurants and workplaces have become more common in many Western countries. Bhutan has had a complete smoking ban since 2005 while India introduced a ban on smoking in public in October 2008. The World Health Organization has called for governments to institute a total ban on tobacco advertising to prevent young people from taking up smoking. They assess that such bans have reduced tobacco consumption by 16% where instituted.
Screening
Cancer screening uses medical tests to detect disease in large groups of people who have no symptoms. For individuals with high risk of developing lung cancer, computed tomography (CT) screening can detect cancer and give a person options to respond to it in a way that prolongs life. This form of screening reduces the chance of death from lung cancer by an absolute amount of 0.3% (relative amount of 20%). High risk people are those age 55–74 who have smoked equivalent amount of a pack of cigarettes daily for 30 years including time within the past 15 years.
CT screening is associated with a high rate of falsely positive tests which may result in unneeded treatment. For each accurate positive scan there are about 19 false positive scans. Other concerns include radiation exposure and the cost of testing along with follow up. Research has not found two other available tests—sputum cytology or chest radiograph (CXR) screening tests—to have any benefit.
The United States Preventive Services Task Force (USPSTF) recommends yearly screening using low-dose computed tomography in those who have a total smoking history of 30 pack-years and are between 55 and 80 years old until a person has not been smoking for more than 15 years. Screening should not be done in those with other health problems that would make treatment of lung cancer if found not an option. The English National Health Service was in 2014 re-examining the evidence for screening.
Other prevention strategies
The long-term use of supplemental vitamin A, vitamin C, vitamin D or vitamin E does not reduce the risk of lung cancer. Some studies have found vitamin A, B, and E may increase the risk of lung cancer in those who have a history of smoking.
Some studies suggest that people who eat diets with a higher proportion of vegetables and fruit tend to have a lower risk, but this may be due to confounding—with the lower risk actually due to the association of a high fruit and vegetables diet with less smoking. Several rigorous studies have not demonstrated a clear association between diet and lung cancer risk, although meta-analysis that accounts for smoking status may show benefit from a healthy diet.
Management
Treatment for lung cancer depends on the cancer's specific cell type, how far it has spread, and the person's performance status. Common treatments include palliative care, surgery, chemotherapy, and radiation therapy. Targeted therapy of lung cancer is growing in importance for advanced lung cancer. People who have lung cancer should be encouraged to stop smoking. There is no clear evidence which smoking cessation program is most effective for people who have been diagnosed with lung cancer. It is unclear if exercise training is beneficial for people who have advanced lung cancer. Exercise training may benefit people with NSCLC who are recovering from lung surgery. In addition, exercise training can benefit people with NSCLC who have received radiotherapy, chemotherapy, chemoradiotherapy, or palliative care.
Exercise training before lung cancer surgery improves outcomes. A home-based component in rehabilitation is also useful. Even though it is uncertain if home-based prehabilitation leads to less adverse events or hospitalization time, rehabilitation with a home-based component may improve recovery after treatment and overall lung health.
Surgery

If investigations confirm NSCLC, the stage is assessed to determine whether the disease is localized and amenable to surgery or if it has spread to the point where it cannot be cured surgically. CT scan and positron emission tomography (PET-CT), non-invasive tests, can be used to help rule out malignancy or mediastinal lymph node involvement. If mediastinal lymph node involvement is suspected using PET-CT, the nodes should be sampled (using a biopsy) to assist staging, a PET-CT scan is not accurate enough to be used alone. Techniques used for obtaining a sample include transthoracic needle aspiration, transbronchial needle aspiration (with or without endobronchial ultrasound), endoscopic ultrasound with needle aspiration, mediastinoscopy, and thoracoscopy. Blood tests and pulmonary function testing are used to assess whether a person is well enough for surgery. If pulmonary function tests reveal poor respiratory reserve, surgery may not be possible.
In most cases of early-stage NSCLC, removal of a lobe of lung (lobectomy) is the surgical treatment of choice. In people who are unfit for a full lobectomy, a smaller sublobar excision (wedge resection) may be performed. However, wedge resection has a higher risk of recurrence than lobectomy. Radioactive iodine brachytherapy at the margins of wedge excision may reduce the risk of recurrence. Rarely, removal of a whole lung (pneumonectomy) is performed. Video-assisted thoracoscopic surgery (VATS) and VATS lobectomy use a minimally invasive approach to lung cancer surgery. VATS lobectomy is equally effective compared to conventional open lobectomy, with less postoperative illness.
In SCLC, chemotherapy and/or radiotherapy is typically used. However the role of surgery in SCLC is being reconsidered. Surgery might improve outcomes when added to chemotherapy and radiation in early stage SCLC.
The effectiveness of lung cancer surgery (resection) for people with stage I - IIA NSCLC is not clear, however, weak evidence suggests that a combined approach of lung cancer resection and removing the mediastinal lymph nodes (mediastinal lymph node dissection) may improve survival compared to lung resection and a sample of mediastinal nodes (not a complete node dissection).
Radiotherapy

Radiotherapy is often given together with chemotherapy, and may be used with curative intent in people with NSCLC who are not eligible for surgery. This form of high-intensity radiotherapy is called radical radiotherapy. A refinement of this technique is continuous hyperfractionated accelerated radiotherapy (CHART), in which a high dose of radiotherapy is given in a short time period. Radiosurgery refers to the radiotherapy technique of giving a precise high-dose of radiotherapy that is guided by a computer. Postoperative (adjuvant) thoracic radiotherapy generally should not be used after curative-intent surgery for NSCLC. Some people with mediastinal N2 lymph node involvement might benefit from post-operative radiotherapy.
For potentially curable SCLC cases, chest radiotherapy is often recommended in addition to chemotherapy. The ideal timing of these therapies (the optimal time to give radiotherapy and chemotherapy for improving survival) is not known.
If cancer growth blocks a short section of bronchus, brachytherapy (localized radiotherapy) may be given directly inside the airway to open the passage. Compared to external beam radiotherapy, brachytherapy allows a reduction in treatment time and reduced radiation exposure to healthcare staff. Evidence for brachytherapy, however, is less than that for external beam radiotherapy.
Prophylactic cranial irradiation (PCI) is a type of radiotherapy to the brain, used to reduce the risk of metastasis. PCI is most useful in SCLC. In limited