Myeloma, Multiple
A number sign (#) is used with this entry because several chromosome aberrations, including recurrent translocations and deletions, have been found to be related to the development or progression of multiple myeloma; see CYTOGENETICS section.
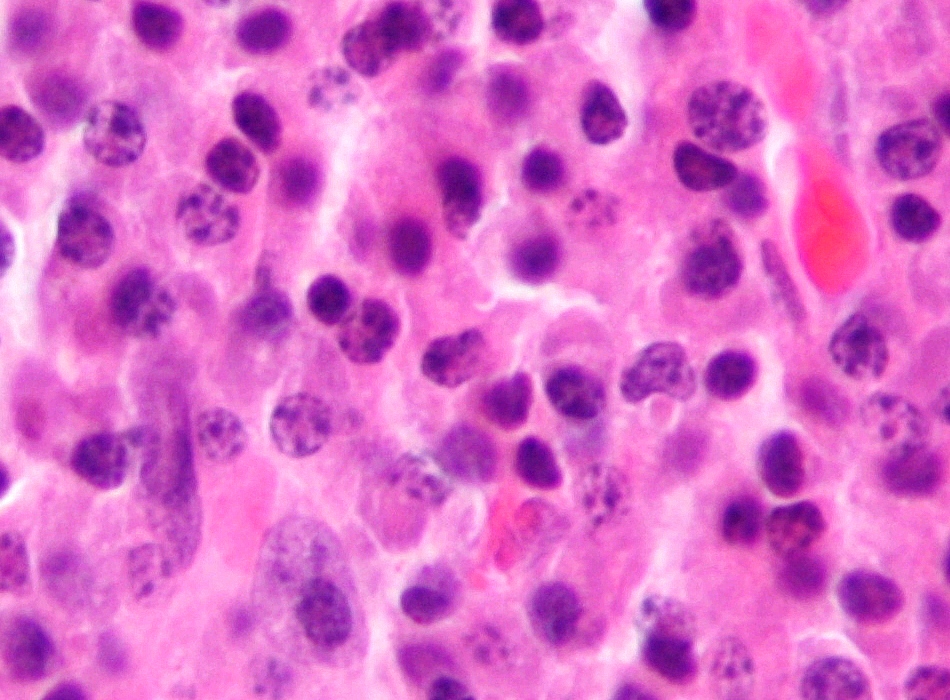
DescriptionMultiple myeloma is a neoplastic plasma cell disorder characterized by clonal proliferation of malignant plasma cells in the bone marrow microenvironment, monoclonal protein in the blood or urine, and associated organ dysfunction (Palumbo and Anderson, 2011).
Clinical FeaturesLeoncini and Korngold (1964) described multiple myeloma in 2 sisters and reviewed the literature on familial cases. Manson (1961) reported affected sisters, one of whom also had pernicious anemia. Myeloma has also been observed in father and son (Nadeau et al., 1956). Thomas (1964) observed myeloma in a brother and sister. Alexander and Benninghoff (1965) described 3 affected black sibs. Whitehouse (1971) observed affected brother and sister.
In a large population survey in Sweden, Axelsson and Hallen (1965) found 2 families, one with 2 and one with 3 sibs, showing high monoclonal (M)-component. In a third family, 2 persons with high M-component were more remotely related. These 7 were from a total group of 59 (out of 7,918) found to have M-component. Their condition was considered to be a variety of essential benign monoclonal hypergammaglobulinemia.
Berlin et al. (1968) described familial occurrence of M-components. One possible explanation for familial paraproteinemia is that plasma cell clones with similar structural genes for the paraprotein synthesized by these cells proliferate in related individuals. This hypothesis predicts that paraproteins from 2 members of the same family would be identical. The paraproteins of a mother with multiple myeloma and a son with probably benign monoclonal gammopathy were isolated by Grant et al. (1971). Light chains were of the lambda type, but had differences on peptide map in both the common and variable regions of the proteins. These data showed that the structural genes operative in paraprotein light chain production in these first-degree relatives are different. The presence of a genetic basis was suggested by the occurrence of 2 different monoclonal gammopathies in 1 patient. Humphrey (1973) described a patient who had an intracranial plasmacytoma that was surgically removed. Six years later she developed a plasmacytoma of 1 kidney. The second tumor produced a different gamma globulin from that released into the cerebrospinal fluid by the brain plasmacytoma.
Zawadzki et al. (1977) described 19 cases of familial immunopathy, distributed in 9 families. Ten members of 5 families had multiple myeloma, 5 members of 2 families had lanthanic paraproteinemia, and 4 members of 2 families had one or the other of these. 'Lanthanic' is from a Greek word meaning 'to escape.' It is used in place of 'benign' because malignant immunocytic dyscrasia has been known to emerge. The term is intended to convey that the condition was asymptomatic and came to attention only by serendipity. (Actually, in the course of a specific study of relatives of clinically affected probands, this is not serendipity; Walpole's Prince of Serendip set out to find one thing and instead found something else (Cannon, 1945).)
Blattner (1980) gave an excellent review, with a classification of monoclonal gammopathies. Multiple myeloma and Waldenstrom macroglobulinemia (153600) are presumably closely related; both are malignant monoclonal gammopathies. Multiple myeloma is about 2 times more frequent in U.S. blacks than in US whites; it is the eleventh and twentieth most frequent malignancy in the 2 races, respectively.
Horwitz et al. (1985) reported 3 affected sibs and stated that a review of the literature revealed reports of 38 affected pairs of sibs, 8 families with 3 affected sibs, and 4 families with another affected relative (in addition to the pair of affected sibs). Comotti et al. (1987) and Judson et al. (1985) reported identical twins concordant for multiple myeloma.
Jensen et al. (1988) described a brother and sister with progressive mixed axonal and demyelinating polyneuropathy in association with a monoclonal IgM gammopathy of kappa and lambda type, respectively. Sera from both patients contained antibodies directed to bovine peripheral nerve myelin as determined by ELISA technique and to normal human peripheral nerve myelin as demonstrated by indirect immunofluorescence histochemistry. These sibs may have had a genetic predisposition to the formation of autoantibodies with peripheral nerve myelin as the target.
Deshpande et al. (1998) described 5 families in which plasma cell dyscrasia occurred in parent and child generations (6 such pairs), and pooled data with those of 16 other families (with 20 parent-child pairs affected) recorded in the literature. In all 6 previously unreported parent-child pairs with plasma cell dyscrasia and in 18 of 20 such pairs found in the literature, the disease occurred at an earlier age in the child generation. The median age of onset of myeloma in parent and child generations of all 26 pairs was 71 years and 50 years, respectively. The ages of onset of malignant plasma cell dyscrasias in the parent and child generations of these families compared with patients in the general population was significantly different for the child generation but not for the parent generation. It thus appears that anticipation occurs in familial myeloma.
Grosbois et al. (1999) studied 15 families with 2 or more cases of multiple myeloma. In 10 of the 15, myeloma was observed in sibs, in whom the mean age at diagnosis was similar to that in unrelated multiple myeloma cases. In those families with multiple myeloma in successive generations, the mean age at diagnosis was lower. The monoclonal component was identical (IgG kappa) in 7 families. A family history of monoclonal gammopathy of undetermined significance was observed in 3 families. Five other prospective studies of 1,263 patients identified 4 affected families (3.2 per 1,000 cases of multiple myeloma).
Lynch et al. (2008) reported a large African American family in which 5 individuals had multiple myeloma, 3 had monoclonal gammopathy of undetermined significance (MGUS), i.e., without signs of malignant lymphocytic or plasmocytic disease, and 5 had prostate cancer. One additional member had pancreatic cancer. The putative progenitor had died of colon cancer at age 88 years.
Systemic (AL) Amyloidosis
AL amyloidosis, formerly called primary amyloidosis, is a protein conformation disorder associated with a clonal plasma cell dyscrasia (Falk et al., 1997). Multiple organ disease results from the extracellular deposition of monoclonal immunoglobulin light chain fragments in an abnormal insoluble fibrillar form. AL amyloidosis may be associated with myeloma or other B-cell malignancy, but in most cases the underlying plasma cell dyscrasia is subtle and nonproliferating, analogous to MGUS (Guidelines Working Group of UK Myeloma Forum, 2004).
Gertz et al. (1986) reported primary immunoglobulin-related amyloidosis in 2 members of each of 3 families: 2 brothers, a brother and a sister, and 2 first cousins. Primary amyloidosis of this type may be closely akin to multiple myeloma and to Waldenstrom macroglobulinemia.
Miliani et al. (1996) described 3 Italian sibs (2 brothers and a sister) with immunoglobulin-related amyloidosis. Systemic amyloidosis was associated with monoclonal gammopathy in all 3. One of the sibs had Waldenstrom macroglobulinemia, whereas the other 2 had no evidence of multiple myeloma or related diseases. All 3 sibs showed a common pattern of polyneuropathy to different degrees; 2 presented a sicca syndrome and 1 also suffered from nephropathy.
Dispenzieri et al. (2004) concluded that high-dose chemotherapy with peripheral blood stem cell transplantation (PBSCT) in AL patients is associated with higher response rates and higher overall survival than standard chemotherapy. Their conclusion was based on a matched case-control study comparing overall survival of 63 AL patients undergoing transplantation with 63 patients not undergoing transplantation.
CytogeneticsDysregulation of oncogenes by translocations to the IgH locus (147100) on 14q32 is a seminal event in the pathogenesis of B-cell tumors, including multiple myeloma. Translocations to the IgH locus occur in 20 to 60% of cases of myeloma; a diverse array of chromosomal partners have been identified, with 11q13 (see cyclin D1; 168461) being frequently involved. Bergsagel et al. (1996) developed a comprehensive Southern blot assay to identify and distinguish different kinds of IgH switch recombination events. Illegitimate switch recombination fragments (defined as containing sequences from only 1 switch region) are potential markers of translocation events into IgH switch regions and were identified in 15 of 21 myeloma cell lines, including 7 of 8 karyotyped lines that had no detectable 14q32 translocation. These translocation breakpoints involved 6 chromosomal loci: 4p16.3; 6; 8q24.13; 11q13.3; 16q23.1; and 21q22.1.
Chesi et al. (1997) found the novel, karyotypically silent translocation t(4;14)(p16.3;q32.3) in 5 myeloma cells lines and in at least 3 of 10 primary tumors. The chromosome-4 breakpoints were clustered in a 70-kb region centromeric to FGFR3 (134934), which was thought to be the dysregulated oncogene. This translocation selectively expressed an FGFR3 allele containing activating mutations identified previously in thanatophoric dwarfism: tyr373 to cys (134934.0016), lys650 to glu (134934.0004), and lys650 to met (134934.0015). For K650E, the constitutive activation of FGFR3 in the absence of ligand had been proved by transfection experiments. Chesi et al. (1997) proposed that after the t(4;14) translocation, somatic mutation during tumor progression frequently generates an FGFR3 protein that is active in the absence of ligand. Although they could not exclude the possibility that other genes are dysregulated by the translocation t(4;14), several findings pointed to FGFR3. FGFR3 is located no more than 100 kb from the most centromeric breakpoint at 4p16.3, and is on the derivative(14) chromosome that contains the 3-prime IgH enhancer. This is similar to the situation for cyclin D1, which is located 100 to 400 kb from the breakpoint in the translocation t(11;14) that occurs in mantle-cell lymphoma and multiple myeloma tumors. FGFR3 is another example of a gene that can function both as an oncogene and a 'teratogene.'
Palumbo and Anderson (2011) noted that primary early translocations at the Ig switch region at 14q32.33 are commonly juxtaposed to MAF (177075) on chromosome 16q23 and MMSET (602952) on chromosome 4p16.3; the latter results in the deregulation of FGFR3 in 30% of cases.
In multiple myeloma cell lines, Iida et al. (1997) identified a t(6;14)(p25;q32) translocation in 2 of 11 cell lines. The translocation juxtaposes the immunoglobulin heavy-chain (IGHG1; 147100) locus to the MUM1 gene (IRF4; 601900), a member of a gene family known to be active in the control of B-cell proliferation and differentiation. As a result of the translocation, the MUM1/IRF4 gene is overexpressed, an event that may contribute to tumorigenesis, as Iida et al. (1997) showed that MUM1/IRF4 has oncogenic activity in vitro.
In a study of 32 patients with AL (24 with systemic and 8 with localized disease), Harrison et al. (2002) found translocations involving IGH and in addition found deletions of 13q, using dual-color interface fluorescence in situ hybridization. IGH translocations were observed in 11 patients, of whom 9 had the IGH/CCND1 (168461) fusion from t(11;14)(q13;q32).
Mohamed et al. (2007) reviewed the chromosome aberrations in a series of 120 multiple myeloma cases with abnormal karyotypes.
PathogenesisBCLB (BCL2L10; 606910) is an antiapoptotic BCL2 (151430) family protein that is expressed predominantly in B lymphocytes. Using flow cytometric and Western blot analyses, Hamouda et al. (2016) found high expression of BCLB in MM patients compared with low or undetectable expression in MGUS patients and healthy donors. Hamouda et al. (2016) proposed that BCLB may be a robust marker of MM.
Molecular GeneticsShaffer et al. (2008) used a loss-of-function, RNA interference-based genetic screen to demonstrate that inhibition of IRF4 (601900) is toxic to myeloma cell lines, regardless of transforming oncogenic mechanism. Gene expression profiling and genomewide chromatin immunoprecipitation analysis uncovered an extensive network of IRF4 target genes and identified MYC (190080) as a direct target of IRF4 in activated B cells and myeloma. Unexpectedly, IRF4 was itself a direct target of MYC transactivation, generating an autoregulatory circuit in myeloma cells. Shaffer et al. (2008) suggested that although IRF4 is not genetically altered in most myelomas, they are nonetheless addicted to an aberrant IRF4 regulatory network that fuses the gene expression programs of normal plasma cells and activated B cells.
Roddam et al. (2002) investigated the potential impact of 2 LIG4 polymorphisms--ala3 to val (A3V; 601837.0005) and thr9 to ile (T9I; 601837.0006), both caused by C-to-T transitions--on predisposition to several lymphoproliferative disorders, including leukemia, lymphoma, and multiple myeloma (254500), a tumor characterized by aberrant immunoglobulin class switch recombination. The A3V CT and T9I CT and TT genotypes were significantly associated with reduction in risk of developing multiple myeloma. The polymorphisms were in linkage disequilibrium, and a protective effect associated with them was found to be the result of the inheritance of the A3V-T9I CT and A3V-T9I TT haplotypes. These data suggested that genetic variants of NHEJ LIG4 may modulate predisposition to multiple myeloma.
One complication of multiple myeloma patients on bisphosphonate therapy is osteonecrosis of the jaw. In a genomewide association study of 2 series of patients with multiple myeloma, 1 group of 22 with osteonecrosis of the jaw and another group of 65 patients without osteonecrosis of the jaw, Sarasquete et al. (2008) found a significant association between development of the complication and 4 SNPs (rs1934951, rs1934980, rs1341162, and rs17110453) mapping to chromosome 10q23 in the CYP2C8 gene (601129) (p values ranging from 1.07 x 10(-6) to 6.22 x 10(-6)). One SNP, rs1934951, remained significant even after Bonferroni correction (p corrected value = .02). Genotyping revealed an overrepresentation of the T allele of this SNP in cases compared to controls (48% vs 12%). Individuals homozygous for the T allele had a significantly increased likelihood of developing osteonecrosis of the jaw (odds ratio of 12.75).
Preuss et al. (2009) screened a human fetal brain-derived macroarray with the IgA or IgG paraprotein-containing sera of 192 consecutive patients with monoclonal gammopathy of undetermined significance (MGUS) or multiple myeloma, and found that 29 (15.1%) of the 192 paraproteins reacted with a protein they designated 'paratarg-7,' which was found to be identical to stomatin-like protein-2 (STOML2; 608292).
Grass et al. (2009) studied 35 probands with MGUS or multiple myeloma who had an antiparatarg-7 paraprotein and found that all 35 patients expressed hyperphosphorylated paratarg-7 (615121), whereas hyperphosphorylation was not observed in 217 other patients with MGUS or multiple myeloma whose paraprotein did not bind to paratarg-7. Paratarg-7 hyperphosphorylation was also found in 4 (2%) of 200 healthy blood donors, none of whom had monoclonal immunoglobulins in their serum. Thus, hyperphosphorylation of paratarg-7 appeared to be associated with a significantly increased risk of developing MGUS or multiple myeloma (odds ratio, 7.9; p = 0.0001). Analysis of 8 of the 35 families with paratarg-7-specific paraprotein in their serum showed that the hyperphosphorylated state of paratarg-7 was inherited in an autosomal dominant fashion. Grass et al. (2009) noted that there were healthy carriers of hyperphosphorylated paratarg-7 who were older than the respective index patient, indicating that factors other than age determine if and when a carrier of hyperphosphorylated paratarg-7 develops a paratarg-7-specific paraprotein.
Chapman et al. (2011) reported the massively parallel sequencing of 38 tumor genomes and their comparison to matched normal DNAs from individuals with multiple myeloma. Several new and unexpected oncogenic mechanisms were suggested by the pattern of somatic mutation across the data set. These included the mutation of genes involved in protein translation (seen in nearly half of the patients), genes involved in histone methylation, and genes involved in blood coagulation. In addition, a broader than anticipated role of NF-kappa-B (see 164011) signaling was indicated by mutations in 11 members of the NF-kappa-B pathway. Of potential immediate clinical relevance, activating mutations of the kinase BRAF (164757) were observed in 4% of patients, suggesting the evaluation of BRAF inhibitors in multiple myeloma clinical trials.
Weinhold et al. (2013) found an association between the 870G allele of a polymorphism in the CCND1 gene (168461.0001) and risk of t(11;14) multiple myeloma.
Li et al. (2017) noted that genomewide association studies have suggested that variation at chromosome 5q15 influences risk of MM. They identified a G-C SNP, rs6877329, within a predicted enhancer element that physically interacted with the transcription start site of ELL2 (601874), which is critical for B-cell differentiation. The C risk allele of rs6877329 was associated with reduced enhancer activity and lower ELL2 expression. Li et al. (2017) proposed that reduced ELL2 expression may contribute to arrest of plasma-cell development and facilitate MM clonal expansion.
Animal ModelPlasma cell tumor induction in mice by pristane is under multigenic control. Backcross and congenic strain analyses indicated that at least 4 genes determine the susceptibility to mouse plasmacytomagenesis. One of these genes, Pctr1, resides in the mid-portion of mouse chromosome 4 near the alpha-interferon locus. Zhang et al. (1998) presented evidence that Cdkn2a (600160) is a strong candidate for the Pctr1 locus.
Hamouda et al. (2016) noted that the closest homolog of human BCLB in mouse exhibits different expression and function than the human protein. They generated transgenic mice expressing human BCLB exclusively in B lymphocytes. Mice expressing BCLB developed an MM-like disease. Survival of homozygous (+/+) BCLB-expressing mice was significantly lower than wildtype, and hemizygous (-/+) BCLB-expressing mice had intermediate survival with increased numbers of Cd138 (SDC1; 186355)-positive plasmocytes. Hemizygous Bclb-expressing mice exhibited monoclonal hypergammaglobulinemia. Malignant plasma cells of hemizygous Bclb-expressing mice were both transplantable and treatable with conventional MM therapies. Hamouda et al. (2016) proposed that BCLB-expressing mice recapitulate the pathogenesis of human MM and may be valuable in evaluating novel MM therapies.