Hereditary Fructose Intolerance
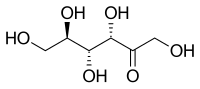
Hereditary fructose intolerance (HFI) is an autosomal recessive disorder of fructose metabolism (see this term), resulting from a deficiency of hepatic fructose-1-phosphate aldolase activity and leading to gastrointestinal disorders and postprandial hypoglycemia following fructose ingestion. HFI is a benign condition when treated, but it is life-threatening and potentially fatal if left untreated.
Epidemiology
The estimated prevalence is 1 in 20,000 in Europe and the carrier frequency is about 1 in 70. The prevalence of HFI in adult population is not known.
Clinical description
HFI usually presents in infancy at the time of weaning (when fructose is added to the diet), manifesting with hypoglycemia, lactic acidosis, ketosis with recurrent vomiting, abdominal pain and systemic manifestations following consumption of fructose-containing foods. Persistent ingestion of fructose and related sugars (such as sucrose and sorbitol) may lead to growth retardation, hepatomegaly, proximal tubular dysfunction, liver and renal failure, seizures, coma and risk of death. All patients achieve adulthood, develop a natural aversion to fruit/sweets and report a life long history of vomiting and hypoglycemia following fructose ingestion. Dental caries are absent in a significant proportion of adult population with HFI (which may give a clue to the diagnosis). Sometimes, the diagnosis may be made in an adult who has, owing to his aversion to fructose, excluded all fructose-containing food since childhood.
Etiology
HFI is caused by mutations in the ALDOB (9q22.3) gene, encoding the enzyme aldolase B. Affected individuals fail to metabolize fructose completely in the liver, intestine and kidneys because of fructose-1-phosphate aldolase B deficiency, leading to accumulation of the substrate fructose-1-phosphate and subsequent depletion of adenosine triphosphate.
Diagnostic methods
Early diagnosis is essential, as patients can live a symptom-free life by eliminating fructose from their diet. When clinical features, nutritional and family history are suggestive, HFI is confirmed by molecular diagnosis on DNA from peripheral leucocytes. Very rarely, when no mutation can be found, liver biopsy may be performed to assess aldolase B activity.Early diagnosis is essential, as patients can live a symptom-free life by eliminating fructose from their diet. When clinical features, nutritional and family history are suggestive, HFI is confirmed by molecular diagnosis on DNA from peripheral leucocytes. Very rarely, when no mutation can be found, liver biopsy may be performed to assess aldolase B activity.
Differential diagnosis
Differential diagnoses include pyloric stenosis, gastro-esophageal reflux,galactosemia, tyrosinemia, glycogen storage disease, ornithine transcarbamoylase deficiency, Wilson disease, tumor of hematopoietic and lymphoid tissue (see these terms) and fructose malabsorption.
Antenatal diagnosis
Prenatal diagnosis is technically possible in families with known mutations, but it is not indicated due to the benign nature of this condition.
Genetic counseling
HFI is an autosomal recessive condition.
Management and treatment
Whenever HFI is suspected, fructose should be eliminated from diet. This involves avoiding all types of food in which fructose, sucrose and/or sorbitol is found, either naturally or added during processing, including certain pharmacological preparations and infant formulae. The beneficial clinical and chemical effects of withdrawal are usually seen within a few days. Multivitamin preparation may be prescribed to substitute vitamins, especially vitamin C and folates. Intensive care and supportive measures may be required in case of acute intoxication
Prognosis
HFI prognosis is favorable with normal growth, intelligence and lifespan.